Food Bolus Ileus as a Cause of High-Grade Bowel Obstruction: A Case Report
Jin Kook Kang, MD1,2* Zhifei Sun, MD1
1Department of Surgery, MedStar Georgetown University Medical Center, Washington, DC, USA
2Department of Surgery, MedStar Washington Hospital Center, Washington, DC, USA
*Corresponding Author: Jin Kook Kang, Department of Surgery, MedStar Georgetown University Medical Center, Washington, DC, USA
Received: 15 February 2023; Accepted: 23 February 2022; Published: 27 March 2023
Article Information
Citation: Jin Kook Kang, Zhifei Sun. Food Bolus Ileus as a cause of High-Grade Bowel Obstruction: A Case Report. Journal of Surgery and Research 6 (2023): 137-139.
View / Download Pdf Share at FacebookAbstract
Small bowel obstruction is often caused by previous surgical scar or cancer. High grade bowel obstruction secondary to food bolus impaction is very rare especially in a young patient who has otherwise no medical or surgical history. We are presenting a unique case in a young male who presented with acute abdomen with initial CT scan suggestive of Meckel’s diverticulitis. During exploratory laparotomy, patient was found to have a severe degree of bowel obstruction with one definitive transition point caused by food bolus impaction. Food bolus ileus is a rare cause of bowel obstruction requiring surgical intervention. However, definitive intervention should not be delayed when patients present with concerning clinical signs.
Keywords
Small bowel obstruction, Food bolus ileus, Case Report
Case Report articles
Small bowel obstruction articles Small bowel obstruction Research articles Small bowel obstruction review articles Small bowel obstruction PubMed articles Small bowel obstruction PubMed Central articles Small bowel obstruction 2023 articles Small bowel obstruction 2024 articles Small bowel obstruction Scopus articles Small bowel obstruction impact factor journals Small bowel obstruction Scopus journals Small bowel obstruction PubMed journals Small bowel obstruction medical journals Small bowel obstruction free journals Small bowel obstruction best journals Small bowel obstruction top journals Small bowel obstruction free medical journals Small bowel obstruction famous journals Small bowel obstruction Google Scholar indexed journals Food bolus ileus articles Food bolus ileus Research articles Food bolus ileus review articles Food bolus ileus PubMed articles Food bolus ileus PubMed Central articles Food bolus ileus 2023 articles Food bolus ileus 2024 articles Food bolus ileus Scopus articles Food bolus ileus impact factor journals Food bolus ileus Scopus journals Food bolus ileus PubMed journals Food bolus ileus medical journals Food bolus ileus free journals Food bolus ileus best journals Food bolus ileus top journals Food bolus ileus free medical journals Food bolus ileus famous journals Food bolus ileus Google Scholar indexed journals Meckel’s diverticulitis articles Meckel’s diverticulitis Research articles Meckel’s diverticulitis review articles Meckel’s diverticulitis PubMed articles Meckel’s diverticulitis PubMed Central articles Meckel’s diverticulitis 2023 articles Meckel’s diverticulitis 2024 articles Meckel’s diverticulitis Scopus articles Meckel’s diverticulitis impact factor journals Meckel’s diverticulitis Scopus journals Meckel’s diverticulitis PubMed journals Meckel’s diverticulitis medical journals Meckel’s diverticulitis free journals Meckel’s diverticulitis best journals Meckel’s diverticulitis top journals Meckel’s diverticulitis free medical journals Meckel’s diverticulitis famous journals Meckel’s diverticulitis Google Scholar indexed journals GIA stapler articles GIA stapler Research articles GIA stapler review articles GIA stapler PubMed articles GIA stapler PubMed Central articles GIA stapler 2023 articles GIA stapler 2024 articles GIA stapler Scopus articles GIA stapler impact factor journals GIA stapler Scopus journals GIA stapler PubMed journals GIA stapler medical journals GIA stapler free journals GIA stapler best journals GIA stapler top journals GIA stapler free medical journals GIA stapler famous journals GIA stapler Google Scholar indexed journals Resected small bowel articles Resected small bowel Research articles Resected small bowel review articles Resected small bowel PubMed articles Resected small bowel PubMed Central articles Resected small bowel 2023 articles Resected small bowel 2024 articles Resected small bowel Scopus articles Resected small bowel impact factor journals Resected small bowel Scopus journals Resected small bowel PubMed journals Resected small bowel medical journals Resected small bowel free journals Resected small bowel best journals Resected small bowel top journals Resected small bowel free medical journals Resected small bowel famous journals Resected small bowel Google Scholar indexed journals Peri-intestinal lymph nodes articles Peri-intestinal lymph nodes Research articles Peri-intestinal lymph nodes review articles Peri-intestinal lymph nodes PubMed articles Peri-intestinal lymph nodes PubMed Central articles Peri-intestinal lymph nodes 2023 articles Peri-intestinal lymph nodes 2024 articles Peri-intestinal lymph nodes Scopus articles Peri-intestinal lymph nodes impact factor journals Peri-intestinal lymph nodes Scopus journals Peri-intestinal lymph nodes PubMed journals Peri-intestinal lymph nodes medical journals Peri-intestinal lymph nodes free journals Peri-intestinal lymph nodes best journals Peri-intestinal lymph nodes top journals Peri-intestinal lymph nodes free medical journals Peri-intestinal lymph nodes famous journals Peri-intestinal lymph nodes Google Scholar indexed journals food bolus impaction articles food bolus impaction Research articles food bolus impaction review articles food bolus impaction PubMed articles food bolus impaction PubMed Central articles food bolus impaction 2023 articles food bolus impaction 2024 articles food bolus impaction Scopus articles food bolus impaction impact factor journals food bolus impaction Scopus journals food bolus impaction PubMed journals food bolus impaction medical journals food bolus impaction free journals food bolus impaction best journals food bolus impaction top journals food bolus impaction free medical journals food bolus impaction famous journals food bolus impaction Google Scholar indexed journals high-grade bowel obstruction articles high-grade bowel obstruction Research articles high-grade bowel obstruction review articles high-grade bowel obstruction PubMed articles high-grade bowel obstruction PubMed Central articles high-grade bowel obstruction 2023 articles high-grade bowel obstruction 2024 articles high-grade bowel obstruction Scopus articles high-grade bowel obstruction impact factor journals high-grade bowel obstruction Scopus journals high-grade bowel obstruction PubMed journals high-grade bowel obstruction medical journals high-grade bowel obstruction free journals high-grade bowel obstruction best journals high-grade bowel obstruction top journals high-grade bowel obstruction free medical journals high-grade bowel obstruction famous journals high-grade bowel obstruction Google Scholar indexed journals inflammatory bowel disease articles inflammatory bowel disease Research articles inflammatory bowel disease review articles inflammatory bowel disease PubMed articles inflammatory bowel disease PubMed Central articles inflammatory bowel disease 2023 articles inflammatory bowel disease 2024 articles inflammatory bowel disease Scopus articles inflammatory bowel disease impact factor journals inflammatory bowel disease Scopus journals inflammatory bowel disease PubMed journals inflammatory bowel disease medical journals inflammatory bowel disease free journals inflammatory bowel disease best journals inflammatory bowel disease top journals inflammatory bowel disease free medical journals inflammatory bowel disease famous journals inflammatory bowel disease Google Scholar indexed journals
Article Details
Introduction
Small bowel obstruction is a common disease that represents 12 to 16% of surgical admissions and more than 300,000 operations annually in the United States [1]. Most common cause is adhesions from prior abdominal surgery. Other common causes include incarcerated hernias, neoplastic processes, and inflammatory bowel diseases. Small bowel obstruction from impacted food bolus is a rare but well documented phenomenon [2]. We present an interesting case of high-grade small bowel obstruction caused by food bolus impaction in a young, healthy patient whose CT scan initially suggested small bowel obstruction from Meckel’s diverticulitis.
Case Report
A 22-year-old male with no past medical or surgical history presented to our emergency department with a 15-hour history of sharp periumbilical abdominal pain associated with nausea and vomiting after eating a cucumber for dinner. He had passed a small amount of flatus since the pain started. His last bowel movement was one day prior to presentation. He had no medication history or known drug allergies. He endorsed occasional cigarette, marijuana, and alcohol use. He’s a visiting student from Germany. He did not have specific diet restrictions and denied any changes of diet recently.
His initial vital signs upon presentation were stable with temperature 36.5°C, blood pressure 151/83mmHg, heart rate 77, and oxygen saturation 100% on room air. His labs on admission were remarkable for white blood cell count of 19.4K/uL, hemoglobin of 17.9mg/dL, and calcium level of 10.8mg/dL. Lactic acid level was normal at 1.8mmol/L. Abdominal exam showed soft, mildly distended, and mildly tender to palpation predominantly in periumbilical and right hemiabdomen. Abdominal CT scan with only IV contrast showed progressive distention of small bowel up to 4.5cm in diameter and stasis of the intraluminal content at the level of the transition point in the left pelvis (Figure 1). A segment of small bowel at the level of transition point had thickened wall with mesenteric edema that appeared to be blind ending, which raised a suspicion for Meckel’s diverticulitis (Figure 2). Given patient’s overall clinical presentation and CT findings, we decided to perform a diagnostic laparoscopy.
During the case, there was a clear transition point from dilated bowel to normal small bowel in the jejunum. Upon palpation, there was a nodular appearance in the bowel and adjacent mesentery appeared to have some desmoplastic reaction. Unlike CT finding, there was no evidence of Meckel’s diverticulum or associated inflammation (Figure 3). Bowels appeared viable. Decision was made to perform small bowel resection and primary anastomosis in case of a mass lesion. Upon enterotomy, it was noted to have significant amount of digested materials in the small bowel lumen. We resected the involved segment of small bowel and performed primary anastomosis with GIA stapler. Resected small bowel was sent to pathology lab for detailed review. Common enterotomy was closed with a TA stapler and reinforced with absorbable sutures in Lembert fashion. Entire small bowels were examined and showed no other abnormalities. 19Fr drain was placed. Fascia and skin were subsequently closed. Patient had an uneventful hospital course and was discharged on post-operative day 6. Pathology of the specimen showed submucosal edema without necrosis or hemorrhage. There was no evidence of neoplasm or other significant abnormalities including Meckel’s diverticulum. Peri-intestinal lymph nodes were normal.
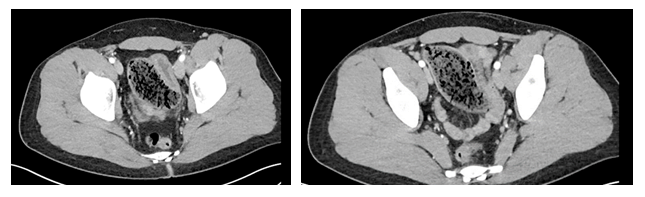
Figure 1: Abdominal CT scan with findings of stasis of intraluminal content

Figure 2: Abdominal CT with findings of segment of small bowel with blind ending

Figure 3: Intraoperative picture demonstrating a clear transition point but no Meckel’s diverticulum
Discussion
Small bowel obstruction from food bolus impaction is a rarely known phenomenon [2]. According to some reports, it is associated with significant morbidity and mortality up to 5% [3,4]. Some reports suggest 4% of small bowel obstruction is associated with this etiology [5]. This is more frequently observed in elderly patients with no teeth, those who had previous gastric surgery, and small bowel diverticula [6]. History of gastric surgery has been a well known cause of food bolus obstruction as gastric stasis and reduction in acid secretion increases the chance of bezoar formation [7]. Certain food such as persimmons, pineapples, and prickly pears (cactus fruit/figs) are known to be associated with bezoar formation [8]. Some literature suggests one of the most commonly impacted sites is near the ileocecal valve, which is the narrowest part of the small bowel with least peristaltic activities [9], although other sites such as jejunum, sigmoid colon, and rectum can also be involved [10]. There is usually a smooth tapering of collapsed bowel distal to the obstruction.
Clinical diagnosis of small bowel obstruction secondary to food impaction should be made with thorough history and physical, physical exam, and laboratory and imaging findings. One can present with broad symptoms of obstruction including severe abdominal pain with intermittent cramps, nausea, vomiting, diarrhea, constipation, and distended abdomen [10]. High-pitched bowel sounds may or may be present. Abdominal CT is the best imaging modality as it provides important diagnostic information that is not readily apparent in other radiographs such as abdominal X-ray, barium studies, or ultrasound. One study suggests that CT has a positive predictive value of 20% in diagnosing phytobezoar, demonstrating stool-like mass with a solid rim and heterogenous, “mottled-gas” appearing center that did not take up contrast [10-12]. However, CT may not provide precise etiology of the small bowel obstruction as seen in our presented case.
In case of concerning clinical presentations of high-grade bowel obstruction such as severe abdominal pain, unstable vitals signs, and/or abnormal lab findings (leukocytosis, lactic acidosis, etc.), one should not delay exploratory laparotomy for both diagnostic and therapeutic intervention. Operating surgeon may attempt to break up the food bolus and milk down through the ileocecal valve [10]. If this fails, an enterotomy should be made in order to extract the intraluminal contents. Small bowel resection should be considered in the setting of suspicious mass lesion or compromised bowel. Finally, surgeon must examine the entire bowel to evaluate additional sites of obstruction because, if missed, patient may experience worsening obstruction, eventually requiring additional operations [10].
One retrospective study of 31 Chinese patients who had food bolus obstruction showed 42% of the study population had intact gastrointestinal intact (no abdominal surgeries or medical conditions that predispose to gastric stasis such as hypothyroidism or diabetes) [13]. It should be noted that their normal diet consisted of high dietary intake of vegetables and fruits which may increase the risk of bezoar formation. Our case is interesting as patient demonstrated no risk factors such as previous gastric surgery, abnormally high fiber diet, or other medical conditions.
Conclusion
Small bowel obstruction due to food bolus impaction is a rare but well reported disease. Although more frequently associated with previous gastric surgeries, certain diets, and inflammatory bowel disease, it can be manifested in patients with no identifiable risk factors. Correct diagnosis is often made during diagnostic or exploratory laparotomy as CT may not detect exact cause. Surgeons should always keep in mind that food bolus impaction can cause high-grade small bowel obstructions and that surgical intervention should not be delayed in patients with concerning presentations.
Conflicts of interest
Authors disclose no conflicts of interests and sources of funding.
References
- Maung AA, Johnson DC, Piper GL, et al. Eastern Association for the Surgery of Trauma. Evaluation and management of small-bowel obstruction: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 73 (2012):S362-S369.
- Davies DG, Lewis RH. Food obstruction of the small intestine: a review of 15 cases. Br Med J 2 (1959): 545-548.
- Schlang HA, McHenry LE. Obstruction of the small bowel by orange in the postgastrectomy patient. Ann Surg 159 (1964): 611-622.
- Van Eeden A, Retief P. Intestinal obstruction and dried peaches. S Afr Med J. 64 (1983): 377.
- Bevan P. Acute intestinal obstruction in the adult. Br J Hosp Med 28 (1982): 258-265.
- Jane? J. Bolus ileus-an occasional cause of small bowel obstruction-case report. International Journal of Research in Medical Sciences 5 (2017): 5447.
- Hayes PG, Rotstein OD. Gastrointestinal phytobezoars: presentation and management. Can J Surg 29 (1986): 419-420.
- Manning EP, Vattipallly V, Niazi M, Shah A. PhytobezoarInduced Small Bowel Obstruction in a Young Male with Virgin Abdomen. J Gastrointest Dig Syst. 5 (2015): 266.
- Katzka DA, Jaffe DL. Clinical Challenges and Images in GI. Gastroenterology 133 (2007): 176-178.
- Knott-Craig CJ, Du Toit DF, Van Schalkwyk P, et al. Bolus obstruction of the intestine. Case reports. S Afr Med J 67 (1985):1025-1026.
- Smerieri N, Barbieri I, Fumagalli M, et al. A rare cause of mechanical bowel obstruction: ingested vinyl glove. Unexpected diagnosis at laparoscopy. Clin Case Rep 5 (2017): 1026-1027.
- Bedioui H, Daghfous A, Ayadi M, et al. A report of 15 cases of small-bowel obstruction secondary to phytobezoars: predisposing factors and diagnostic difficulties. Gastroenterol Clin Biol 32 (2008): 596-600.
- Lee JF, Leow CK, Lai PB, et al. Food bolus intestinal obstruction in a Chinese population. Aust N Z J Surg. 67 (1997): 866-868.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 