Forehead Flap a Workhorse Flap for Facial Reconstruction- Our Experience at Tertiary Care Institute
Seema Mittal*, Jaskirat Singh Makkar, Dilpreet Singh, Raman Mittal
Department of Surgery, Shri Guru Ram Das Institute of Medical Sciences, Amritsar, India
*Corresponding Author: Seema Mittal, Department of Surgery, Shri Guru Ram Das Institute of Medical Sciences, Amritsar, India/p>
Received: 05 January 2024; Accepted: 18 January 2024; Published: 22 February 2024
Article Information
Citation: Seema Mittal, Jaskirat Singh Makkar, Dilpreet Singh, Raman Mittal. Forehead Flap a Workhorse Flap for Facial Reconstruction- Our Experience at Tertiary care institute. Journal of Surgery and Research. 7 (2024): 72-75.
View / Download Pdf Share at FacebookAbstract
Background: Managing post-traumatic or post-oncosurgical facial defects presents challenges. Minor defects may be treated with skin grafts or small local flaps, while larger ones necessitate advanced techniques like tissue expanders, prefabricated flaps, or free flaps. The enduring utilization of the forehead flap over centuries underscores its reliability in reconstructing substantial and intricate facial defects.
Aim: Assess the viability and adaptability of forehead flap for facial reconstruction.
Materials and Methods: 20 patients who underwent coverage of facial defects after trauma or tumor excision using forehead flaps were retrospectively analysed. The patient satisfaction and flap-related complications were analyzed.
Results: 20 patients (18 males and two females) underwent reconstruction of different facial defects using 20 forehead flaps. The complication occurred in one patient only. The remaining 19 patients showed no complications and passed an uneventful follow-up period. All the patients were fully satisfied.
Conclusion: The forehead flap effectively addresses facial defects, likely offering optimal results with its excellent skin match in color, texture, and thickness. Despite the rising popularity of free flaps, the forehead flap remains a valid and secure choice, ensuring both aesthetic and functional success in covering facial defects.
Keywords
<p>Facial Reconstruction, Facial Defects, Forehead Flap</p>
Article Details
Introduction
Facial reconstruction refers to the procedure of re-establishing the appearance and function of the face, typically after trauma, surgery, congenital anomalies, or other conditions that result in facial defects. This specialized field involves various surgical techniques and procedures aimed at rebuilding facial structures, such as the skin, underlying tissues, and bone, to enhance both aesthetics and functionality.
The goal of facial reconstruction is to achieve a natural and pleasant-sounding appearance while restoring essential functions, such as breathing, eating, and facial expression.
Reconstructing complicated facial defects presents an ongoing challenge for plastic surgeons. Various absent components must be evaluated and reconstructed based on the individual patient's requirements. The earliest account of nasal reconstruction using the mid-forehead flap dates back to approximately 600 A.D. [1].
The initial English documentation of the mid-forehead flap surfaced in the Madras Gazette in 1793 and, a year later, was published in the Gentleman's Magazine of London. In 1816, the English surgeon J.C. Carpue reported two successful cases of nasal reconstruction utilizing the forehead flap [1]. Kazanjian popularized the classic mid-forehead flap with a vertical orientation, situated in the midline of the frontal region, in the United States in 1946 [2].
The paramedian forehead flap is a commonly used and reliable facial tissue graft, particularly beneficial in midface reconstruction. Its excellence is evident in reconstructing the distal nose, capitalizing on similarities in sebaceous gland quality and tissue thickness with the forehead.
In 700 BC, nasal tip amputation was a common punishment for a variety of crimes. Its treatment was described in a medical treatise entitled the Sushruta Samita [3]. Millard innovated the paramedian position by excluding central glabellar skin, reducing morbidity while preserving viability. Menick enhanced Millard's design by narrowing the pedicle, offering increased versatility in movement and length [4]. A skilfully executed forehead flap yields a natural, durable, and inconspicuous nasal reconstruction [5].
The purpose of this study was to showcase the adaptability of the forehead flap in reconstructing various anatomical facial units. Emphasizing the importance of repeating and refining surgical techniques is crucial until achieving a facial contour and definition that meets satisfactory standards.
Aim and Objective
This study aims to demonstrate the versatility of forehead flap in the reconstruction of facial defects, which provides adequate contour and good aesthetic outcome.
Material and Methods
This is a retrospective study done in the department of general surgery at tertiary care center from January 2018 to January 2022. All the patients where forehead flap was done to cover facial defects due to various indications were taken for study. Forehead flap is a two stage procedure. All flaps underwent a second stage for flap separation three weeks post-operation. The analysis included evaluating the size of the harvested flap, the timing of harvesting, outcomes of the transferred flaps, patient satisfaction, and complications related to the flaps. Severe complications were characterized by more than one-fourth total flap loss, while moderate complications involved less than one-fourth flap loss. Minor complications were described as instances of dehiscence or hematoma leading to wound healing impairment. Patient satisfaction categories were defined as very satisfied (VS), satisfied (S), and not satisfied (NS).
Operative technique: Forehead Flap was done in two stages. In stage 1, The patient underwent general anaesthesia, and strict aseptic measures were observed throughout the procedure. We performed a wide local excision with appropriate margins in cases involving Basal Cell Carcinoma (BCC) and Squamous Cell Carcinoma (SCC). The defect area was meticulously recreated for defects resulting from Mucor Mycosis or traumatic injuries.
After recreating the defect, we identified a paramedian flap based on the ipsilateral supratrochlear vessel, located approximately 1.5cm from the midline. It was crucial to ensure that the base of the paramedian flap had a minimum width of 1.5cm. The flap was extended into the hair-bearing scalp in areas where additional length was needed. The forehead flap was carefully raised in a distal to proximal direction, preserving all scalp layers, including the skin, subcutaneous tissue, and frontalis muscle, except for the periosteum. Primary donor site closure was performed, and the flap was utilized to cover the defect. In stage 2: After a healing period of 21 days, the flap was detached and carefully inset into its final position. The post-operative recovery period proceeded without any complications (Figures 1-5).
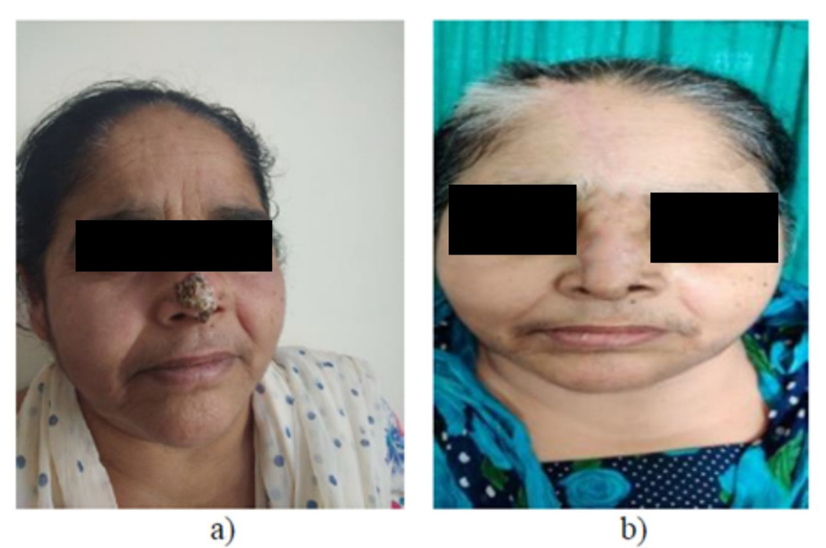
Figure 1: a) 55year old female with Basal Cell Carcinoma of tip of nose. b) 10 days post-operative picture (after flap division)
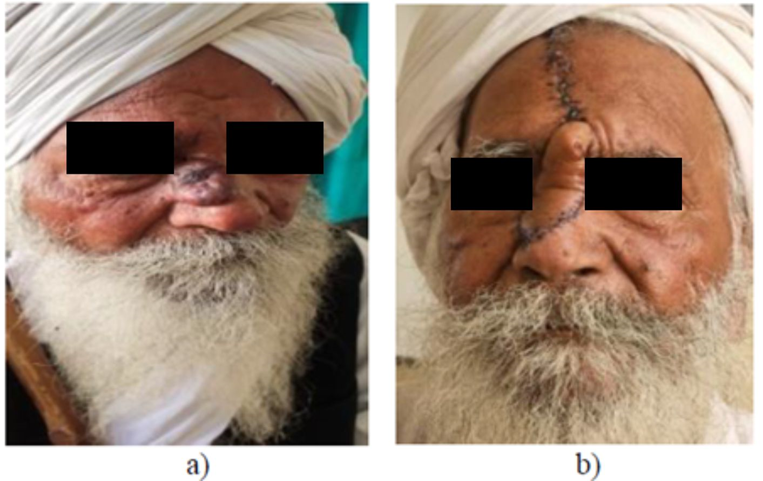
Figure 2: a) 70 year old male with Basal Cell Carcinoma over dorsum of nose as well as right lateral wall of nose. b) 10 days postoperative pic with forehead flap in situ
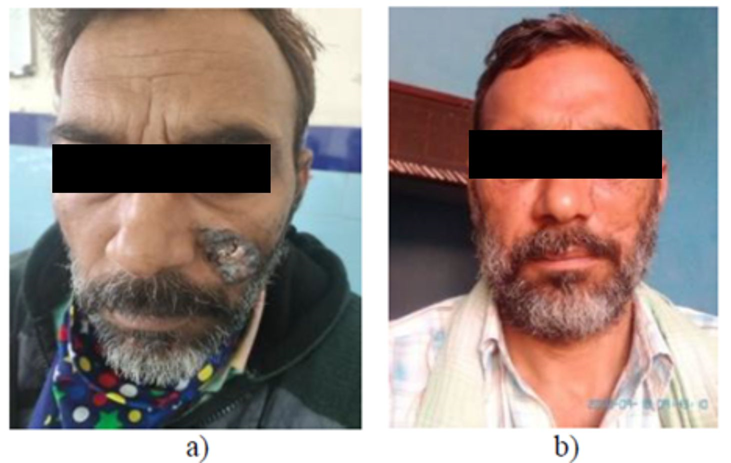
Figure 3: a) 45 year old with Basal cell carcinoma of Left cheek. b) late postoperative pic

Figure 4: a) 10yr old male child with defect of nasal tip and left Ala due to injury by Pitbull, showing marking for forehead flap. b) intraoperative pic showing flap elevation. c) intra-operative pic showing flap insetting. d) intraoperative pic after flap division (second stage)
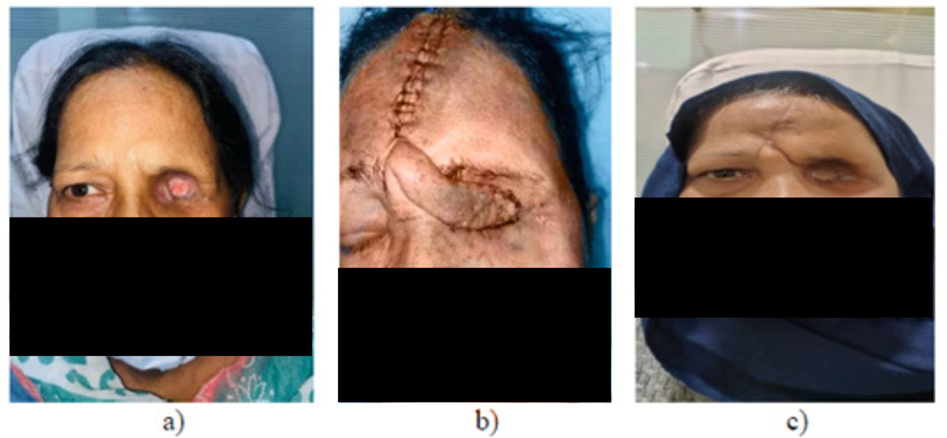
Figure 5: a) 55 year old female after left orbital exenteration due to Mucor mycosis (defect in left orbital socket). b) socket reconstruction using forehead flap, 7 days postoperative pic. c) pic after flap detachment and insetting
Results
In this study, out of the 20 patients, 18 were males, and only two females underwent facial reconstruction of different defects using forehead flaps. The mean age of patients was 37.3±16.6 years, the Minimum age of patients was 10, and the maximum age was 70 years. The facial defects involved Basal cell carcinoma, post-COVID orbital Mucor Mycosis, Squamous Cell Carcinoma nose and Post Traumatic Defect Nose 50%, 25%, 15% and 10%, respectively. Five patients had defects on their noses, another five in the orbital region, and the remaining ten patients exhibited defects on their cheeks (Figure 6).
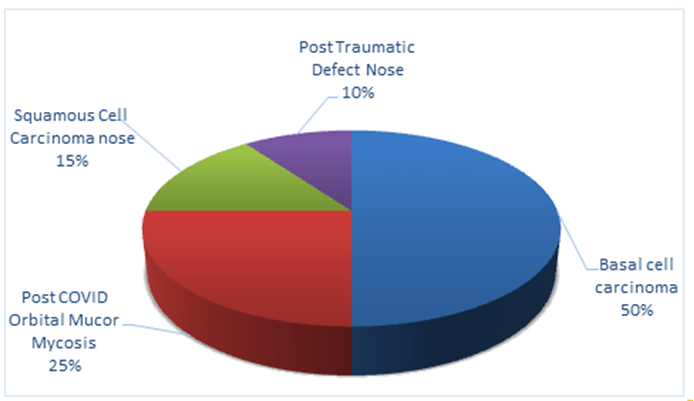
Figure 6: Distribution of patients on the basis of facial defects
The average time of flap produce was between 30 minutes to 45 minutes in this study. Mean flap sizes was from (2 cm×10 cm) to (3 cm × 12 cm).
The complications happened in one patient only, i.e. hair on the nose, which was later treated with a laser hair removal procedure. The 95% of patients representing no complications and passed an uneventful follow-up period. Overall, patient satisfaction is delivered 100%. The flap survival rate was seen to be 100%. Mean hospital stay was 10.2±5.7 days, ranging from 3 to 21 days. Follow up ranged from 6 to 12 months.
Discussion
The forehead is the optimal donor site for facial resurfacing thanks to its favourable skin quality, size, and vascularity. Blood supply comes from the supratrochlear and supraorbital vessels inferiorly and from the superficial temporal, postauricular, and occipital vessels superiorly and laterally [6].
None of the flaps experienced full-thickness necrosis or congestion, necessitating medical intervention. These findings align with the outcomes observed by Stephen and Park, who conducted single-stage forehead flap reconstructions on ten patients. Of these cases, only one patient experienced epidermolysis, while the remaining patients had an uncomplicated postoperative recovery [7].
We concur with Millard's perspective that the midline forehead skin flap is versatile for facial or nasal reconstructions, spanning from extensive tip and alar loss to complete nasal defects. This flap allows for aesthetic and functional reconstruction, harmonizing the created nose with the overall facial features [8].
Indeed, free flaps are widely recognized as the benchmark in numerous head and neck reconstruction cases. Nevertheless, a growing body of data has been accumulating, albeit gradually, indicating the successful application of pedicled flaps in similar scenarios. In many cases, both pedicled regional and microvascular soft tissue flaps vie for the same indications, with each technique offering its distinct advantages and drawbacks. This evolving landscape underscores the importance of selecting the most appropriate method based on the patient's specific needs and the surgical context's intricacies [9].
The forehead flap has consistently effectively addressed various nasal defects, yielding favorable outcomes and minimal complications. Remarkably, even in the context of free flap reconstructions, regional flaps continue to play a significant role and remain competitive in achieving excellent aesthetic results while covering nasal defects.
Limitation of the study
In order to thoroughly evaluate the viability and adaptability of the forehead flap in facial reconstruction, it is imperative to broaden the study to include a larger patient population. This expansion will contribute to a more comprehensive and robust understanding of the capabilities of the forehead flap in various reconstructive scenarios.
Conclusion
The forehead flap remains a workhorse, a successful and minimally complicated flap covering various facial defects, providing good aesthetic outcomes. Despite the emergence of free flap reconstructions, regional flaps, mainly the forehead flap and its variants, continue to play a crucial role, competing favourably in achieving both aesthetic and functional success in facial defect coverage. In conclusion, the forehead flap is a valid and secure choice for managing facial defects, offering optimal results in color, texture, and thickness matching.
Funding:
No funding sources
Conflict of interest:
None declared
Ethical approval:
Approved by the Institutional Ethics Committee
Acknowledgement
We express our sincere gratitude to the patients who participated in this study, their willingness and cooperation was essential to the success of our research.
References
- Cintra HPL, Bouchama A, Holanda T, et al. Uso do retalho médio-frontal na reconstrução do nariz. Rev Bras Cir Plást 28 (2013): 212-217.
- Menick FJ. Nasal Reconstruction: Forehead Flap. Plast Reconstr Surg 113 (2004): 100e-111e.
- Jackson IT. Local Flaps in Head and Neck Reconstruction. St. Louis, MO: Mosby (1985).
- Menick FJ. Aesthetic refinements in use of forehead for nasal reconstruction: the paramedian forehead flap. Clin Plast Surg 17 (1990): 607-622.
- Converse JM. Philadelphia, PA: WB Saunders; 1977. Reconstructive Plastic Surgery, (2nd edtn), pp: 694.
- Menick FJ. Nasal reconstruction. Plast Reconstr Surg 125 (1977): 138-150.
- Park SS. The single-stage forehead flap in nasal reconstruction an alternative with advantages. Arch Facial Plast Surg 4 (2020): 32-36.
- Millard DR. Midline Forehead Skin Flap. In: Berish S, editor. Grabb’s Encyclopedia of Flaps. Philadelphia: Lippincott Williams & Wilkins 11 (2009): 99-100.
- Colletti G, Tewfik K, Bardazzi A, et al. Regional flaps in head and neck reconstruction: a reappraisal. J Oral Maxillofac Surg 73 (2015): 571.e1-571.e10.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 