Hepatocellular Carcinoma in Transposition of Great Arteries (TGA) with Atrial Switch Procedure: A Case Report and Review of the Literature
Pierre-Alexandre Fontanges1, Olivia Domanski1*, Francois Godart1
Department of Pediatric and Congenital Heart Diseases, CHU Lille, 59000, Lille, France
*Corresponding Author: Pierre-Alexandre Fontanges, Department of Pediatric and Congenital Heart Diseases, CHU Lille, 59000, Lille, France
Received: 16 August 2022; Accepted: 24 August 2022; Published: 31 October 2022
Article Information
Citation: Pierre-Alexandre Fontanges, Olivia Domanski, Francois Godart. Hepatocellular Carcinoma in Transposition of Great Arteries (TGA) with Atrial Switch Procedure: A Case Report and Review of the Literature. Journal of Surgery and Research 5 (2022): 578-580.
View / Download Pdf Share at FacebookAbstract
Primary liver cancer is the seventh most frequently occurring cancer in the world [1]. Alcohol, steatosis and hepatotrophic viruses the main causes of liver fibrosis and known to have direct oncogenics effects. Steatosis is now the first cause in developed countries. Another less common mechanism of HCC is congestive liver disease as in Budd Chiari Syndrome [2] or Fontan procedure [3-5]. Non-pulsatile flow secondary to a Fontan procedure lead to a congestive and chronicle elevated central veins pressure resulting in Fontan-associated liver disease (FALD) [5]. Incidence of liver fibrosis and HCC in other congenital heart diseases is not known while life expectancy has increased in this population.
Keywords
<p>Carcinoma, Liver cancer, Budd Chiari Syndrome</p>
Article Details
Introduction
Primary liver cancer is the seventh most frequently occurring cancer in the world [1]. Alcohol, steatosis and hepatotrophic viruses the main causes of liver fibrosis and known to have direct oncogenics effects. Steatosis is now the first cause in developed countries. Another less common mechanism of HCC is congestive liver disease as in Budd Chiari Syndrome [2] or Fontan procedure [3-5]. Non-pulsatile flow secondary to a Fontan procedure lead to a congestive and chronicle elevated central veins pressure resulting in Fontan-associated liver disease (FALD) [5]. Incidence of liver fibrosis and HCC in other congenital heart diseases is not known while life expectancy has increased in this population. We report the second case of HCC in a 51-year-old patient with D-TGA operated by Mustard procedure, who had no history of other hepatitis risks factors (no alcohol, no steatosis, no viral infection).
Case Presentation
A 51-year-old male with history of D-TGA who underwent a atrial switch procedure at 4 years old, enter our institution for right heart failure, poor general state and hepatalagia (Figure 1). Blood test revealed an important cytolysis rate, with cholestasis. Hepatic data from 6 months before was normal expect for middle elevated alanine aminotransferase 48UI/ml. In 3 days, congestive symptoms decreased under intra-venous diuretics treatment as the cytolysis. Hepatalgia and moderate cytolysis >2N remained and a CT (computerized tomography) imaging was performed showing a portal trunk thrombosis and a large right liver mass compatible with a hepatocellular carcinoma (Figure 2).
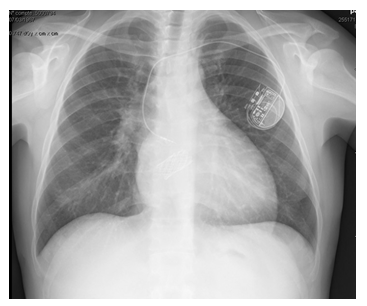
Figure 1: Chest radiograph demonstrating IVC stent placement.
Alpha-fetoprotein was elevated to 23000 ng/ml (N<9). Liver biopsy was not performed cause of bleeding risk. Experts confirmed HCC and to their opinion, patient was unlikely to tolerate or benefit from classic systemic chemotherapy and recommended a palliative treatment with immunotherapy. Unfortunately, immunotherapy was complicated, treatment had to be stopped and patient died within 10 weeks. During his follow up the patient presented no clinical symptoms of chronic heart failure (CHF) and was monitored with regular blood tests and echocardiography. He presented at 26 years old a baffle stenosis treated by balloon dilatation 12 years later. Despite the baffle dilatation, high pressure of 16 mmHg persists in the inferior vena cava (IVC). He also presented a right heart dysfunction evaluated by MRI at 37%. At this time, we recorded no hepatic cytolysis. Three years later, the patient had an baffle restenosis and two endovascular stents were inserted (Figure 1). IVC pressure post procedure was still 15 mmHg but no hepatic veins dilatation was noted. Patient had a monochamber pace maker implantation at age 45 due to sinusal dysfunction. From his 45 to his 50 years old serial echocardiography data showed stable cardiac function with moderate right heart dysfunction, no sub-hepatic veins dilatation, moderately dilated IVC at 18mm. Right catherization found IVC pressure at 19 mmHg and computerized tomography (CT) found no hepatic lesions or concerning features of cirrhosis. The patient had no background of alcohol intake. The serology was negative for HCV (hepatitis C virus) and HBV (hepatitis B virus). Lab evaluation was not consistent with Non Alcoolic steatosis hepatitis (NASH). Triglycerides and cholesterol were within normal limits.
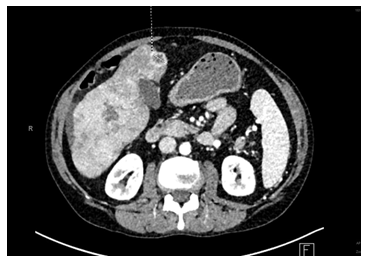
Figure 2: Abdominal CT showing hepatocellular carcinoma
Discussion
Liver fibrosis is a common complication in patients with univentricular hearts palliated with Fontan circulation. Sik Yoon et al. in Cancers 2020 reported 97.7% incidence of cirrhosis at 30 years of Fontan Reparation [5]. To this day, very few cases of hepatic complication have been reported in congenital heart diseases except Fontan correction. Yuko Izumi et al. reported in 2004 a juvenile HCC in a 31-year-old patient with TGA that underwent a Mustard procedure who presented right cardiac insufficiency for several years before [6]. In 2017, Yoshihara et al. published in 2017 a case of an hepatocellular carcinoma due to a baffle obstruction after the mustard operation without previous cardiac insufficiency [7]. In the transposition of the great arteries, Carole Warnes insisted that IVC obstruction is less common but in rare cases may cause hepatic congestion or cirrhosis [8]. In 2013 and 2021, McCabe and Huyn Sung published respectively in the United States and Japan the case of a 45-year-old male and a 34-years-old lady with a history of tetralogy of Fallot diagnosed with HCC with no steatosis nor viral hepatitis nor alcohol cirrhosis [9-11]. Recently, Sakano et al. published in clincical Journal of Gastroenterology 2021 the first case of HCC derived from Rastelli procedure related congestive liver disease to a 41-years-old patient without comorbidity [12]. Considering ours and other case resports of the literature, there is concern that chronic hepatic congestion in patients with a variety of congenital heart diseases are at increased risk of liver fibrosis and HCC. There are no curent guidelines for hepatic surveillance in congenital heart disease at risk of right heart failure. Sik Yoon et al. are giving ideas to help in diagnosis and follow up of liver disease for Fontan patient [5]. Authors suggest that screening for cirrhosis be started 10 years after the Fontan operation. In the limits of the case report, we can highlight other possible causes of HCC in our patient as cumulative radiation exposure or hepatotoxique medication. Unfortunately, our patient was a poor candidate for MRI given his pacemaker, and underwent several CT scans and heart catheterization procedures. Cumulative radiation doses on the last ten years is estimated to 164 mSv but which is less than 1200 mSv considered as the necessary dose to increase the risk of cancer by 1%. Our patient was under amiodarone treatment for years, known to be hepatotoxic and increase risks of liver cancer [13,14].
Conclusion
In this case, we tried to highlight the importance of liver screening to track HCC and fibrosis in patients with congenital heart disease and chronic right heart failure or IVC elevated pressure. We think that a close liver screening with abdominal imaging (using echography) and liver biology (with apha-fetoprotein dosage, alanine aminotransferase, aspartate aminotransferase, total bilirubin) should be recommended to this population to track down HCC like in Fontan patient.
References
- McGlynn KA, Petrick JL, El-Serag HB. Epidemiology of Hepatocellular Carcinoma. Hepatology. Janv 73 (2021): 4-13.
- Shrestha SM. Liver cirrhosis in hepatic vena cava syndrome (or membranous obstruction of inferior vena cava). World J Hepatol 7 (2015): 874-884.
- Conroy MR, Moe TG. Hepatocellular carcinoma in the adult Fontan patient. Cardiol Young. mars 27 (2017): 407-409.
- Mazzarelli C, Cannon MD, Hudson M, et al. Hepatocellular Carcinoma as a Complication of Vascular Disease of the Liver After Fontan Procedure. Hepatology. févr 69 (2019): 911-913.
- Yoon JS, Lee DH, Cho EJ, et al. Risk of Liver Cirrhosis and Hepatocellular Carcinoma after Fontan Operation: A Need for Surveillance. Cancers (Basel) 12 (2020): 15-30.
- Izumi Y, Hiramatsu N, Itose I, et al. Juvenile hepatocellular carcinoma with congestive liver cirrhosis. J Gastroenterol. févr 40 (2005): 204-208.
- Yoshihara T, Sakamori R, Furuta K, et al. Hepatocellular carcinoma due to a baffle obstruction after the mustard operation: A case report. Hepatology 67 (2018): 2471-2473.
- Warnes CA. Transposition of the great arteries. Circulation 114 (2006): 2699-2709.
- McCabe N, Farris AB, Hon H, et al. Hepatocellular carcinoma in an adult with repaired tetralogy of fallot. Congenit Heart Dis 8 (2013): 139-144.
- Hyun Sung J, Sakamori R, Yamada R, et al. Hepatocellular Carcinoma in a Patient with Tetralogy of Fallot: A Case Report and Literature Review. Intern Med 19 (2021): 19-25
- Yugawa K, Kohashi K, Itoh S, et al. Combined hepatocellular-cholangiocarcinoma after tetralogy of Fallot repair: a case report and review of literature. Pathol Res Pract 216 (2020): 152908.
- Sakano Y, Noda T, Kobayashi S, et al. A case report of hepatocellular carcinoma derived from Rastelli procedure-related congestive liver disease. Clin J Gastroenterol 14 (2021): 1525-1529.
- Lim YP, Lin CL, Lin YN, et al. Antiarrhythmic agents and the risk of malignant neoplasm of liver and intrahepatic bile ducts. PLoS One 10 (2015): e0116960.
- Fares WH. Amiodarone and the risk of cancer: a nationwide population-based study. Cancer 119 (2013): 40-51.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 