Spontaneous Pneumothorax in Post COVID-19 Patients - A Case Series
Gaurav Wadhawan, Konark Thakkar*, Ravdeep Singh
Department of Surgery, Pacific Medical College and Hospital, Udaipur, Rajasthan, India
*Corresponding Author: Konark Thakkar, Department of Surgery, Pacific Medical College and Hospital, Udaipur, Rajasthan, India
Received: 11 January 2022; Accepted: 18 January 2022; Published: 24 January 2022
Article Information
Citation: Gaurav Wadhawan, Konark Thakkar, Ravdeep Singh. Spontaneous Pneumothorax in Post Covid-19 Patients - A Case Series. Journal of Surgery and Research 5 (2022): 46-50.
View / Download Pdf Share at FacebookAbstract
Covid- 19 is that the acute respiratory communicable disease caused by novel coronavirus later named as Severe Acute Respiratory Syndrome CoronaVirus 2 (SARS- CoV- 2).Clinical findings of coronavirus outbreak revealed majority of patients as asymptomatic or mild to moderate symptoms while a number of the cases present with severity of disease. New case with complication associated with disease emerges because the number of covid-19 cases raised. We present the case series of 10 patients of spontaneous pneumothorax in post covid-19 patient. Although the precise mechanism remains not known but our observation emphasis on thereon NIV or IV may well be one in all the adding factors to develop post covid pneumothorax.
Keywords
<p>Covid 19, Pneumothorax, NIV, Intercostal tube drainage</p>
Article Details
1. Materials and Methodology
In our study we have included all those patients admitted in Pacific Medical College and Hospital with the complain of covid-19 and post covid pneumothorax during the period of January 2021 to December 2021. All those patients who were admitted with Pneumothorax and did not have the history of covid-19 were not included in our study.
2. Observation
The main conclusive findings in our study during this pandemic was not good, in fact it was the after effect of a big disaster adding on to mortalities. Post covid pneumothorax was reported in 10 of our hospitalised patients, most of them were of age group 61-70 (30%). Male to female ratio was 7:3 and right sided pneumothorax was observed predominantly (70%), only one case presented with bilateral pneumothorax. Post covid pneumothorax was seen more commonly in non smokers (40%) than smokers. There was equal distribution of cases that were on mechanical ventilation and CPAP/NIV and only 2 patients developed spontaneous pneumothorax. Majority of patients did not have any respiratory co-morbidity. Pneumothorax was seen in patients of Diabetes mellitus (47%) and hypertension (35%) who were affected by covid. Clinical change in breathing pattern was the major mode of diagnosis in our case study.
Management:For all the patients an intercostal drainage tube was inserted on the affected side of the patient according to the British Thoracic Society.
3. Discussion
To our knowledge, no relationship between SARS-CoV-2 infection and pneumothorax has been described before. A few cases of pneumothorax after COVID-19 are reported in Pacific Medical Collage and Hospital, Bedla, Udaipur. The latter reports a case of 10 patients with COVID-19 having co-morbidities like hypertension, diabetes type-2, hyperlipidaemia and COPD. Among these patients, 2 patients were re-admitted to hospital for pneumothorax which occurred after admission for COVID-19 [1-5]. A subsequent CT-scan and X-ray revealed extensive bulla formation where first ground-glass opacities had been observed. A pneumothorax is defined as air within the pleural space and may be classified as spontaneous (primary or secondary) or traumatic. Traumatic pneumothorax results from trauma including iatrogenic cases caused during procedures like pacemaker insertions, while secondary spontaneous pneumothorax (SSP) occurs secondary to an underlying lung disease [6,7]. Primary spontaneous pneumothorax (PSP) however, by definition, occurs in patients with no associated lung disease. Indeed, a finding of abnormal pleura however is incredibly common even in PSP patients if hunted for carefully, and include blebs and bullae, which are otherwise referred to as emphysema-like changes [8]. The possible mechanism of COVID-related pneumothorax is attributed to pulmonary parenchymal injury, alveolar membrane damage, and bulla formation, which when subjected to high intra-alveolar pressure during acts like coughing or high positive end-expiratory pressure ventilation leads to pneumothorax [9]. Pneumothorax and/or pneumomediastinum are more frequent in individuals with COVID-19 following tracheal intubation for invasive ventilation. This may be secondary to tracheobronchial injury together with the utilization of larger bore tracheal tubes and better ventilation pressures. The precise mechanism of spontaneous pneumothorax and/or pneumomediastinum in COVID-19 is unknown [10]. According to Begum Oktem, Tarik Yagci1, Fatih Uzer (Departments of Emergency Medical speciality, Thoracic Surgery and couple of Respiratory Disorder, Kastamonu State Hospital, Kastamonu, Turkey) the patients who developed pneumothorax after covid-19 are less likely to be related to lung abnormality, while they’re more related to underlying co-morbidities like DM, Hypertension etc; here in our series too there are only 3 patients who were having lung abnormality remainder of the patients are related to other co-morbidities, among them majority of the patients had Diabetes Mellitus and hypertension and other co-morbidities furthermore. According to S. Zayet, T. Klopfenstein (Infectious Diseases Department, ICU Department, Nord Franche-Comté Hospital, Trevenans, France) patients who are on mechanical ventilation had more chances of developing pneumothorax as a result of pressure imbalance, here we had almost 80% patients who were intubated and kept on mechanical ventilation and they developed pneumothorax. In management part, we managed all the patients with intercostal drainage tube insertion in keeping with guidelines of management of pneumothorax based on the British thoracic society’s (BTS) consensus guidelines, requires that this be undertaken in Level 1 PPE (surgical mask, visor, gown and gloves). BTS further recommends that bubbling chest drains should be considered for strategies to minimise droplet exposure via the chest drain circuit this could be achieved by connecting the chest drain to wall suction (even in cases where suction is not normally indicated but set at a really low level like 5cmH2O) thereby creating a closed system or by installing a viral filter onto the suction port of a Rocket chest drain bottle. Digital drain circuits are an alternate method of reducing risk of droplet spread [11]. In patients with COVID-19 who are on non invasive ventilatory support and ventilatory support are at danger of producing pneumothorax of any side of the lungs, as other studies shows there are risk of developing bilateral pneumothorax, but here in our case report 2/10 patient suffered from bilateral pneumothorax and 8/10 developed unilateral pneumothorax (Figure 1).
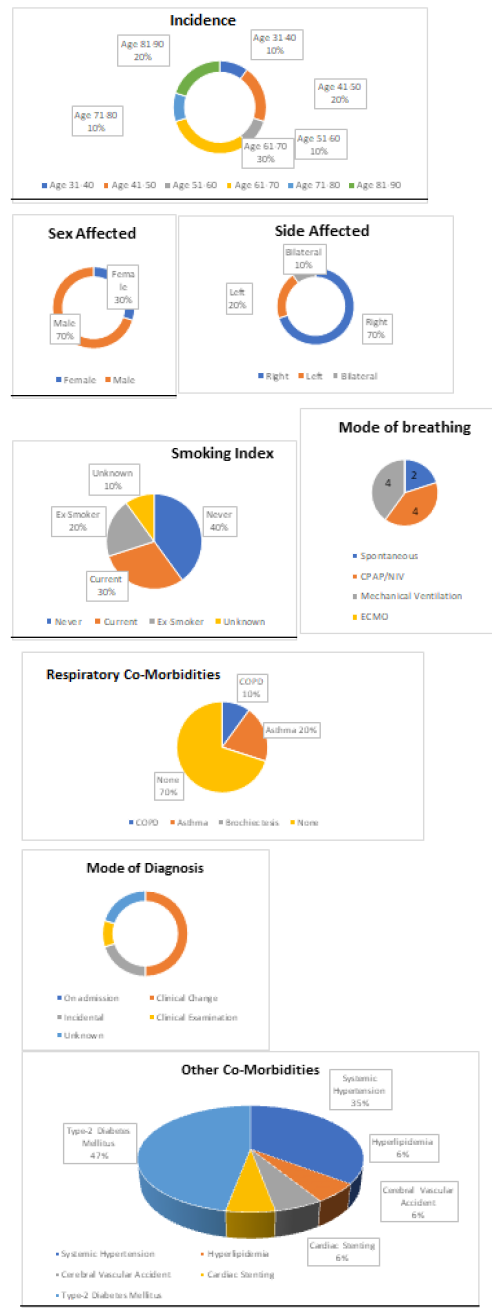
Plate 2: a) inoculated sheath blight Petri dish b) inoculated rice blast Petri dish.
4. Conclusions
Pneumothorax, defined by the presence of air within the pleural cavity with or without collapse of the lung, is usually a life threatening complication and a medical emergency. During the COVID-19 pandemic a rise in pneumothorax incidence, especially among mechanically ventilated patients with COVID-19 infection, has been observed. The mechanical ventilation has deleterious effects on the lung, and pneumothorax could be a known complication of lung ventilation. Although spontaneous pneumothorax has been reported with infections, including COVID-19, the probability of pneumothorax increases from the mixture of parenchymal injury from underlying infection and inflammatory response with additional positive pressure ventilation, further research is required for the clearance of the controversies.
References
- Li Q, Guan X, Wu P, et al. Early transmission dynamics in wuhan, China, of novel coronavirus-infected pneumonia, N Engl J Med 382 (2020): 1199-1207.
- Nikita W and Gaurav W. Presumedly dietary and lifestyle changes during Covid-19 and the subsequent lockdowns among Indian Elderly population. International journal for modern trends in science and technology 7 (2021): 112-116.
- Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome, Lancet Respir Med 8 (2020): 420-422.
- Zheng Y, Yun Z, Yi W. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. European Radiology (2020).
- Quincho-Lopez, Quincho-Lopez DL, HurtadoMedina FD. Case report: pneumothorax and pneumomediastinum as uncommon complications of COVID-19 pneumonialiterature review. The American Journal of Tropical Medicine and Hygiene 103 (2020): 1170-1176.
- Alhakeem, Khan MM, Al Soub H, et al. Case report: COVID-19-associated bilateral spontaneous pneumothorax-a literature review. The American Journal of Tropical Medicine and Hygiene 103 (2020): 1162-1165.
- Jenkinson SG. Pneumothorax. Clinics in Chest Medicine 6 (1985): 153-161.
- Grundy S, Bentley A, Tschopp JM. Primary spontaneous pneumothorax: a diffuse disease of the pleura, Respiration 83 (2012): 185-189.
- Borczuk AC, Salvatore SP, Seshan SV, et al. COVID-19 pulmonary pathology: a multi-institutional autopsy cohort from Italy and New York City. Mod Pathol 33 (2020): 2156-2168.
- Noppen M. Spontaneous pneumothorax: epidemiology, pathophysiology and cause. Eur Respir Rev Off J Eur Respir Soc 19 (2010): 217-219.
- British Thoracic Society Uk, Pleural Services during the COVID-19 Pandemic (2020).


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 