Study of Correlation between Serum Amylase and Serum Lipase level with Percentage of Necrosis on CECT in Acute Necrotising Pancreatitis
Shifa A Kalokhe*, Shrutik Devdikar, Lisha Suraj
Department of General Surgery, MGM Medical College, Navi Mumbai, MGM Institute of Health Sciences, India
*Corresponding Author: Shifa A Kalokhe, Department of General Surgery, MGM Medical College, Navi Mumbai, MGM Institute of Health Sciences, India
Received: 19 June 2022; Accepted: 27 June 2022; Published: 13 July 2022
Article Information
Citation: Shifa A Kalokhe, Lisha Suraj, Shrutik Devdikar. Study of Correlation between Serum Amylase and Serum Lipase level with Percentage of Necrosis on CECT in Acute Necrotising Pancreatitis. Journal of Surgery and Research 5 (2022): 441-444
View / Download Pdf Share at FacebookAbstract
Background
Acute pancreatitis (AP) is a common inflammatory disease of pancreas, mainly characterized by local inflammation of the pancreas due to activation of pancreatic enzymes and increase in serum amylase and lipase levels. As studies suggests 20% of patients with acute pancreatitis develop necrotizing pancreatitis. The aim of our study was to determine whether patients with necrotizing pancreatitis had any significant correlation with Serum Amylase and Lipase Level and if it helps in Early predictability of percentage of Necrosis.
Aim
Methods
To determine correlation between Serum Amylase and Serum Lipase Level with Percentage of necrosis on CECT in patients with Acute Necrotising Pancreatitis. We will be assessing all patients presenting to Institution and diagnosed as a case of Acute Necrotizing Pancreatitis. All Routine Investigation along with Amylase and Lipase done for the Patient, CECT of the Patients were done after 72 hrs of onset of attack. Comparison was done between the relation of Serum Amylase-Lipase level and the percentage of Pancreatic Necrosis mentioned on CECT.
Results
In this retrospective study done from January 2021 to January 2022, 40 cases of Acute Necrotising Pancreatitis were evaluated, it was found that there was no significant correlation between Serum Amylase and Lipase level and the percentage of Necrosis on CECT abdomen.
Conclusion
It was found that level of serum amylase and serum lipase on admission is not a good predictor to assess the percentage of necrosis of pancreas on CECT abdomen. The level of serum amylase and lipas
Keywords
Serum amylase, Serum lipase, Acute necrotizing pancreatitis, Necrosis percentage
Serum amylase articles, Serum lipase articles, Acute necrotizing pancreatitis articles, necrosis percentage articles.
Serum amylase articles Serum amylase Research articles Serum amylase review articles Serum amylase PubMed articles Serum amylase PubMed Central articles Serum amylase 2023 articles Serum amylase 2024 articles Serum amylase Scopus articles Serum amylase impact factor journals Serum amylase Scopus journals Serum amylase PubMed journals Serum amylase medical journals Serum amylase free journals Serum amylase best journals Serum amylase top journals Serum amylase free medical journals Serum amylase famous journals Serum amylase Google Scholar indexed journals Serum lipase articles Serum lipase Research articles Serum lipase review articles Serum lipase PubMed articles Serum lipase PubMed Central articles Serum lipase 2023 articles Serum lipase 2024 articles Serum lipase Scopus articles Serum lipase impact factor journals Serum lipase Scopus journals Serum lipase PubMed journals Serum lipase medical journals Serum lipase free journals Serum lipase best journals Serum lipase top journals Serum lipase free medical journals Serum lipase famous journals Serum lipase Google Scholar indexed journals Acute necrotizing pancreatitis articles Acute necrotizing pancreatitis Research articles Acute necrotizing pancreatitis review articles Acute necrotizing pancreatitis PubMed articles Acute necrotizing pancreatitis PubMed Central articles Acute necrotizing pancreatitis 2023 articles Acute necrotizing pancreatitis 2024 articles Acute necrotizing pancreatitis Scopus articles Acute necrotizing pancreatitis impact factor journals Acute necrotizing pancreatitis Scopus journals Acute necrotizing pancreatitis PubMed journals Acute necrotizing pancreatitis medical journals Acute necrotizing pancreatitis free journals Acute necrotizing pancreatitis best journals Acute necrotizing pancreatitis top journals Acute necrotizing pancreatitis free medical journals Acute necrotizing pancreatitis famous journals Acute necrotizing pancreatitis Google Scholar indexed journals Necrosis percentage articles Necrosis percentage Research articles Necrosis percentage review articles Necrosis percentage PubMed articles Necrosis percentage PubMed Central articles Necrosis percentage 2023 articles Necrosis percentage 2024 articles Necrosis percentage Scopus articles Necrosis percentage impact factor journals Necrosis percentage Scopus journals Necrosis percentage PubMed journals Necrosis percentage medical journals Necrosis percentage free journals Necrosis percentage best journals Necrosis percentage top journals Necrosis percentage free medical journals Necrosis percentage famous journals Necrosis percentage Google Scholar indexed journals reduce morbidity articles reduce morbidity Research articles reduce morbidity review articles reduce morbidity PubMed articles reduce morbidity PubMed Central articles reduce morbidity 2023 articles reduce morbidity 2024 articles reduce morbidity Scopus articles reduce morbidity impact factor journals reduce morbidity Scopus journals reduce morbidity PubMed journals reduce morbidity medical journals reduce morbidity free journals reduce morbidity best journals reduce morbidity top journals reduce morbidity free medical journals reduce morbidity famous journals reduce morbidity Google Scholar indexed journals retro peritoneal fat necrosis articles retro peritoneal fat necrosis Research articles retro peritoneal fat necrosis review articles retro peritoneal fat necrosis PubMed articles retro peritoneal fat necrosis PubMed Central articles retro peritoneal fat necrosis 2023 articles retro peritoneal fat necrosis 2024 articles retro peritoneal fat necrosis Scopus articles retro peritoneal fat necrosis impact factor journals retro peritoneal fat necrosis Scopus journals retro peritoneal fat necrosis PubMed journals retro peritoneal fat necrosis medical journals retro peritoneal fat necrosis free journals retro peritoneal fat necrosis best journals retro peritoneal fat necrosis top journals retro peritoneal fat necrosis free medical journals retro peritoneal fat necrosis famous journals retro peritoneal fat necrosis Google Scholar indexed journals hypertriglyceridemia articles hypertriglyceridemia Research articles hypertriglyceridemia review articles hypertriglyceridemia PubMed articles hypertriglyceridemia PubMed Central articles hypertriglyceridemia 2023 articles hypertriglyceridemia 2024 articles hypertriglyceridemia Scopus articles hypertriglyceridemia impact factor journals hypertriglyceridemia Scopus journals hypertriglyceridemia PubMed journals hypertriglyceridemia medical journals hypertriglyceridemia free journals hypertriglyceridemia best journals hypertriglyceridemia top journals hypertriglyceridemia free medical journals hypertriglyceridemia famous journals hypertriglyceridemia Google Scholar indexed journals hypercalcemia articles hypercalcemia Research articles hypercalcemia review articles hypercalcemia PubMed articles hypercalcemia PubMed Central articles hypercalcemia 2023 articles hypercalcemia 2024 articles hypercalcemia Scopus articles hypercalcemia impact factor journals hypercalcemia Scopus journals hypercalcemia PubMed journals hypercalcemia medical journals hypercalcemia free journals hypercalcemia best journals hypercalcemia top journals hypercalcemia free medical journals hypercalcemia famous journals hypercalcemia Google Scholar indexed journals
Article Details
1. Introduction
Acute pancreatitis (AP) is a common inflammatory disease of pancreas which can be mild and self-limiting without complications or severe with prolonged hospitalization, high morbidity, and high mortality. Acute pancreatitis (AP), mainly characterized by local inflammation of the pancreas due to activation of pancreatic enzymes, accompanied or not by the involvement of proximal tissues and distal organs [1]. It is a common acute abdomen seen in clinical practice and its incidence is increasing [2,3]. Worldwide, the incidence of acute pancreatitis ranges between 5 and 80 per 100,000 population, with the highest incidence recorded in the United States and Finland. Prevalence rate for Pancreatitis in India is 7.9 per 100,000. Prevalence rate for men and women 8.6 and 8.0 per 100,000 respectively in India. According to the The revised Atlanta classification system, introduced in 2012, the clinical course of acute pancreatitis is subdivided into early (1 week) phases relative to disease onset, and the late phase may persist for weeks to months. AP can be subcategorised into interstitial oedematous pancreatitis (IEP) and Necrotising pancreatitis (NP) which can be classified into three types according to the necrotic area involved: pancreatic parenchymal necrosis with peripancreatic necrosis, pancreatic parenchymal necrosis alone, or peripancreatic necrosis alone. As studies and literature suggests 20% of patients with acute pancreatitis develop necrotizing pancreatitis, with a mortality of 8% to 30%. Activated pancreatic enzymes, microcirculatory impairment, and the release of inflammatory mediators lead to rapid worsening of pancreatic damage and necrosis of the gland causing acute necrotising pancreatitis. Necrotizing pancreatitis has a more severe prognosis and a higher mortality rate than interstitial pancreatitis. CECT is the gold standard of investigation. The aim of our study was to determine whether patients with necrotizing pancreatitis had any significant correlation with serum Amylase and Serum Lipase Level and if Level of Serum Amylase-Lipase level helps in Early predictability of percentage of Necrosis.
2. Aim and Objective
To determine correlation between Serum Amylase and Serum Lipase Level with Percentage of necrosis on CECT in patients with Acute Necrotising Pancreatitis.
3. Material and Methods
- All patients who were admitted at the institution under Department of Surgery, MGM hospital, Navi Mumbai, and diagnosed as necrotizing pancreatitis were included in the study.
- Study Design: Retrospective study
- Study Location: Tertiary care teaching hospital-based study done in Department of General Surgery, MGM hospital, Navi Mumbai.
- Study Duration: 1 year January 2021 – January 2022
- Sample size: 40 patients.
- Sample size calculation: The sample size was estimated based on a single proportion design.
- Selection method: The study population was drawn from surgical patients who presented to Mahatma Gandhi Mission Hospital and diagnosed as a case of necrotizing pancreatitis admitted from January 2021 – January 2022
Inclusion criteria
1.Patients diagnosed as case of Acute Necrotising Pancreatitis.
2.Either Sex - Male, Female.
3.Age - Above 18 years.
Exclusion criteria
1.Patient with interstitial oedematous pancreatitis.
2.Under 18 years of age.
3.All patients above the age of 18 years with severe debilitating diseases.
4. Methodology
- All Patients presenting to Institution and diagnosed as a case of Acute Necrotising Pancreatitis were included in the study. All Routine Investigation along with Amylase And Lipase done for the Patient, CECT of the Patients were done after 72 hrs of onset of attack and the CT images were analyzed.
- As per the Atlanta classification, Pancreatic necrosis was defined as area of non-enhancement of pancreatic parenchyma after intravenous administration of contrast media. EPN includes peripancreatic and contiguous retro peritoneal fat necrosis; defined by fat infiltration, collection of fluid/solid components and with increased attenuation (more than 20–30 HU) with heterogeneous appearance [4,5].
- Comparison was done between the relation of Serum Amylase-Lipase level and the percentage of Pancreatic Necrosis mentioned on CECT.
5. Discussion
Acute pancreatitis is a common inflammatory disease of the pancreas with increasing incidence in the western world. It is a complex process in which pancreatic enzyme activation causes local pancreatic damage, resulting in an acute inflammatory response. Acute pancreatitis remains a disease of unpredictable outcome, with a mortality rate of between 10% and 15%. The most common causes of acute pancreatitis are biliary tract stones and alcohol abuse. Other Causes of Pancreatitis include Idiopathic, Iatrogenic, Anatomical obstruction, Drug induced (sulfonamides, metronidazole, erythromycin, tetracyclines, thiazides, furosemide, HMG-CoA reductase inhibitors (statins), azathioprine, 6-mercaptopurine, 5-aminosalicylic acid, sulfasalazine, valproic acid, andacetaminophen), Metabolic (hypertriglyceridemia, hypercalcemia), Miscellaneous (Blunt, penetrating abdominal trauma).
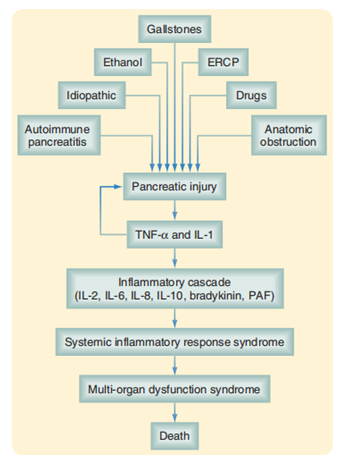
Figure 1: Pathophysiology of Severe Acute Pancreatitis
The cardinal symptom of AP is epigastric or periumbilical pain that radiates to the back. Upto 90% of patients have nausea or vomiting that typically does not relieve the pain. The nature of the pain is constant; therefore, if the pain disappears or decreases, another diagnosis should be considered [6]. Abdomen may be normal or reveal only mild epigastric tenderness. Significant abdominal distention, associated with generalized rebound and abdominal rigidity, is present in severe pancreatitis [6]. According to the The revised Atlanta classification system, introduced in 2012, AP can be subcategorised into interstitial oedematous pancreatitis (IEP) and Necrotising pancreatitis (NP). Pancreatic necrosis is the presence of nonviable pancreatic parenchyma or peripancreatic fat; it can be manifested as a focal area or diffuse involvement of the gland. The acute inflammatory injury that occurs during the first 48 to 72 hours causes mucosal ischemia and reperfusion injury. Both effects favor bacterial overgrowth because they alter local immunity. Mucosal ischemia also produces an increase in the permeability of intestinal cells, which is initiated 72 hours after the acute episode but typically peaks 1 week later. These transient episodes of bacteremia are associated with pancreatic necrosis infection. Less frequently, distant sources of infection, such as pneumonia and vascular or urinary tract infection associated with central lines and catheters, are associated with bacteremia and pancreatic necrosis. Finally, local contamination after surgery or interventional procedures such as ERCP is responsible for necrosis infection. Contrast-enhanced CT is the most reliable technique to diagnose pancreatic necrosis. In acute pancreatitis, serum amylase activity is increased within 2-12 hours of the onset of disease with maximal levels in 12-72 hours which return to normal by the 3rd-4th days [7]. In acute pancreatitis, increased lipase activity in blood is seen after 4-8 h of an attack, peaks at about 24h, and comes back to the normal level by 8-14 days [7]. Serum lipase measurement is a highly specific marker of pancreatic disease than amylase, its activity remains increased for longer than that of serum amylase, and there are no other sources of lipase to reach the blood. Sensitivity for serum amylase is 63.6% and for serum lipase it is 99.5%, whereas specificity for serum amylase 99.4 % and for lipase 99.2% [8].
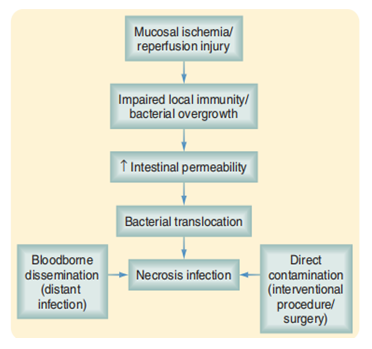
Figure 2: Pathophysiology of Pancreatic Necrosis Infection
As per the Atlanta classification, Pancreatic necrosis was defined as area of non-enhancement of pancreatic parenchyma after intravenous administration of contrast media. EPN includes peripancreatic and contiguous retro peritoneal fat necrosis; defined by fat infiltration, collection of fluid/solid components and with increased attenuation (more than 20-30 HU) with heterogeneous appearance [4,5]. The study is based on level of Serum Amylase and Serum Lipase in Early predictability of percentage of Necrosis which can guide towards early and aggressive management of the patients to reduce morbidity and mortality.
6. Results
- In this Retrospective Study done from January 2021 to January 2022, 40 cases of Acute Necrotising Pancreatitis were evaluated.
- Out of the 40 patients analysed who had Acute Necrotizing Pancreatitis, it was found that there was no significant correlation between Serum Amylase and Serum Lipase level and the percentage of Necrosis on CECT abdomen.
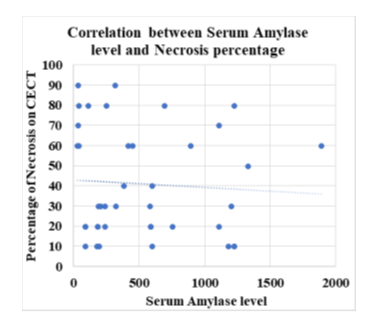
Figure 3: Correlation between serum Amylase level and Necrosis percentage
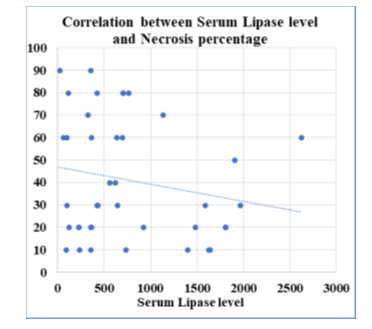
Figure 4: Correlation between serum Lipase level and Necrosis percentage
7. Conclusion
- In this Retrospective Study done from January 2021 to January 2022, 40 cases of Acute Necrotising Pancreatitis were evaluated.
- It was found that level of serum amylase and serum lipase on admission is not a good predictor to assess the percentage of necrosis of pancreas on CECT abdomen.
- The level of serum amylase and lipase depend on the time of onset of symptoms but the patient's presentation to hospital is variable which can be a cause for error.
References
- Delrue LJ, De Waele JJ, Duyck PO. Acute pancreatitis: radiologic scores in predicting severity and outcome. Abdom Imaging 35 (2010): 349-361.
- Bhatia M, Wong FL, Cao Y et al. Pathophysiology of acute pancreatitis. Pancreatology 5 (2005): 132-144.
- Szentesi A, Tóth E, Bálint E et al. Analysis of research activity in gastroenterology: pancreatitis is in real danger (2016).
- Shyu JY, Sainani NI, Sahni VA. et al. Necrotizing pancreatitis: diagnosis, imaging, and intervention. Radiographics 34 (2014): 1218-1239.
- Meyrignac O, Lagarde S, Bournet B, et al. Acute Pancreatitis: Extrapancreatic Necrosis Volume as Early Predictor of Severity. Radiology 276 (2015): 119-128.
- Sabiston Textbook of Surgery- The Biological Basis of Modern Surgical Practice, (21st edtn), pp: 1553-1554
- Treacy J, Williams A, Bais R, et al. Evaluation of amylase and lipase in the diagnosis of acute pancreatitis. ANZ J Surg 71 (2001): 577-582.
- Chang JWY, Chung CH. Diagnosing acute pancreatitis: amylase or lipase Hong kong J Emerg Med 18 (2011): 20-24.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 