Supermagnetic Iron Oxide Tracer in Association with Radioisotope, for Sentinel Node Biopsy in Patients with Complete Axillary Response, After Neoadjuvant Chemoterapy: A Single Center, Prospective Study
Burlizzi S1, Giacobbe F1*, Ranieri E1, Stasolla S1, Villanucci A1, D’Amuri A2, Niccoli A3
1Department of Breast Surgery, Antonio Perrino Hospital, Brindisi, Italy
2Department of Pathological Anatomy, Antonio Perrino Hospital, Brindisi, Italy
3Department of Nuclear Medicine, Antonio Perrino Hospital, Brindisi, Italy
*Corresponding author: Giacobbe Felicia, Department of Breast Surgery, Antonio Perrino Hospital, Brindisi, Italy
Received: 21 July 2021; Accepted: 27 July 2021; Published: 03 September 2021
Article Information
Citation: Burlizzi S, Giacobbe F, Ranieri E, Stasolla S, Villanucci A, D’Amuri A, Niccoli A. Supermagnetic Iron Oxide Tracer in Association with Radioisotope, for Sentinel Node Biopsy in Patients with Complete Axillary Response, After Neoadjuvant Chemoterapy: A Single Center, Prospective Study. Journal of Surgery and Research 4 (2021): 465-472.
View / Download Pdf Share at FacebookAbstract
Although NAC has been shown to be very effective in down staging of the axillary cavity and a complete pathological response (pCR) has been observed in 40-70% of cases (above all in triple negative and Her2+ patients), it was assumed that a pathological response of the tumor alter axillary lymphatic rainage for lymphatic canal fibrosis with cellular debris, reducing the probability of sentinel node (SLN) idetification, with a likely increase in the percentage of false negatives rate (FNR), which as shown by SENTINA trial, where it stands at values of 16%, with a detection rate (DR) of 80%. In light of these observations, different surgical strategies have been put in place to reduce the FNR rate, in order to imporve the number of sentinel/parasentinel nodes and the identification rate (IR) during SNLB in c N+ yc N0 patients, such as the use of double tracer (like vital dye or superparamagnetic iron oxide- SPIO, in association with Tc99), the clip placement in nodes involved before NAC and intraoperative ultrasound (IOUS). Here we will report our experience about the detection rate (DR) and the feasibility of the double tracers, SPIO (Magtrace) + Tc99. We enrolled 20 patients with diagnosis of invasive breast cancer with axillary metastasis, undergoing neodjuvant chemiotherapy and in axillary response after this (cN+ycN0). The overall lymph nodes removed were n°64 between sentinel and parasentinel nodes (52 with Magtrace and 29 with technetium, p-value 0.05). In 12/20 patients (60% of cases) the complementary use of Magtrace allowed us to reach a number of identified lymph nodes ≥ 3, avoinding axillary node dissection in 15/20 (75% of all patients). As demonstrated by our experience, still limited in number of cases, Magtrace® is a valid support in finding the SLN post NAC, both in terms of non-inferiority compared to Tc99, and as a complementary means to the latter in the 'to help us find a number ≥ 3 of LS, essential
Keywords
<p>Breast cancer, Chemotherapy, Ironoxide</p>
Article Details
1. Introduction
For many years, among patients c N+ yc N0, undergoing neoadjuvant chemotherapy (NAC), axillary dissection was the gold standard regardless of the clinical status of axilla, because use of sentinel node biopsy (SLNB) after NAC was considered controversial [1,2]. In particular, although NAC has been shown to be very effective in down staging of the axillary cavity and a complete pathological response (pCR) has been observed in 40-70% of cases (above all in triple negative and Her2+ patients), it was assumed that a pathological response of the tumor alter axillary lymphatic drainage for lymphatic canal fibrosis with cellular debris, reducing the probability of sentinel node (SLN) identification, with a likely increase in the percentage of false negatives rate (FNR), which as shown by SENTINA trial, where it stands at values of 16%, with a detection rate (DR) of 80% [3-5]. At the same time, current data also suggest that in the majority of patients the pathologic stage after NAC has more prognostic value, because response to systemic therapy may prove to be a powerful tool for selecting patients with node-positive disease at diagnosis who can avoid radiotherapy [15,16]. In light of these observations, different surgical strategies have been put in place to reduce the FNR rate, in order to imprve the number of sentinel/parasentinel nodes and the identification rate (IR) during SNLB in c N+ yc N0 patients, such as the use of double tracer (like vital dye or superparamagnetic iron oxide- SPIO, in association with Tc99), the clip placement in nodes involved before NAC and intraoperative ultrasound (IOUS). In the ACOSOG Z0171 trial, patients with node-positive disease underwent NAC followed by both sentinel and axillary node dissection. A FNR of 12,6 was seen with the use of standard sentinel. A subgroup of 96 patients had a clip placed in the positive axillary node at the time of ultrasound (US) guided biopsy and documented its excision at the SLN procedure. When the clip containing lymph node was the SLN, the FNR was reduced to 7.4%. The 2015 NCCN guidelines have included the recommendation to place a marker in the positive axillary node and to remove it at the time of surgery to increase the accuracy of SLN after NAC. Various technique for localizing axillary nodes have been reported, including wire localization, radioactive seed and magnetic seed like Magseed. This last one has shown a detection rate of 97% and was approved in 2016 by FDA for axillary node localization. The MD Anderson researchers developed the taget axillay dissection (TAD) which include a placing of I125seed in metastatic node, localized by a clip under US before NAC, 1-5 days prior surgery. In a population of 208 patients the FNR was of 4,2%. Another technique to improve the SNLs identification after NAC, included intraoperative ultrasound (IOUS): features for suspected malignant lymph nodes are defined by size, morphology, and internal echogenicity (including the cortex and medulla of the visualized node), as well as previously published sonographic criteria like presence of eccentric or uneven cortical thickening (which might be associated with outwardly bulging to perinodal fat or inward indentation to the medulla) and/or disproportionate enlargement of a lymph node that forms an abnormal “rounding” shape. The FNR of only 1.39% make it safe in NAC setting. Here we will report our experience about the detection rate (DR) and the feasibility of the double tracers, SPIO (Magtrace) + Tc99.
2. Methods
2.1 Clinical design and patient recruitment
Patients aged between 18 and 75 years, with invasive breast cancer undergoing neoadjuvant chemotherapy, cN+ (clinical, radiological and cytological diagnosis) ycN0 (clinical and radiological evidence), were enrolled. All immunohistochemical types, with tumor size c T1-2-3, were accepted. Before starting chemotherapy, patients were staged using digital mammography, breast and axillary ultrasound, breast MRI, total body CT and bone scan. During and after NAC a further re-evaluation of loco-regional disease was performed by digital mammography, breast and axillary ultrasound and breast MRI. All patients candidates had both conservative surgery and mastectomy. The LNS and parasentinel lymph node (LNpS) removed were >= 3 and sent for definitive histological examination, with an eventually AD, in a second surgical time, in patients with macrometastases, micrometastases and isolated tumors cells (ICT). The inoculation of the radioisotope took place the day before the surgery or the same morning. The injection of the paramagnetic tracer (Magtrace) was performed in the operating room, in the periareolar area, with localization of the LS at least 20 minutes later. The exclusion criteria were as follows: intolerance or hypersensitivity to iron compounds, pregnancy or lactation, having a pacemaker or other ferrous metal-containing devices in the chest wall, breast implant insertion, liver failure, renal failure, prior axillary surgery, metastasis, absence of axillary response or progression disease after NAC.
2.2 Statistical Methods
We calculated the overall detection rate (DR) obtained by the two tracers (SPIO + Tc99) and the concordance rate (CR) between the two single tracers, in finding LNS and LNpS. We also calculated the level of statistical significance of obtained data by means of the chi-square test, accepting as a pvalue significance of <=0,05.
3. Results
Between June 2019-May 2020 we enrolled 20 patients with diagnosis of invasive breast cancer with axillary metastasis, undergoing neoadjuvant chemotherapy and in axillary response after this (cN+ycN0). The middle age was of 51 years (range 29-62 years). N° 3 patients had a BRCA mutation: N°2 BRCA 1, N°1 BRCA 2 (Table 2)
The detection rate (DR) using Tc-99 was successful in 18 patients (90%) and SPIO in 19 patients (95%).
The concordance rate between the two tracers was of 95% (Table 3)
The overall lymph nodes removed were n°64 between sentinel and parasentinel nodes: 52 with Magtrace and 29 with technetium, pvalue 0.05 (Table 3)
In 12/20 patients (60% of cases) the complementary use of Magtrace allowed us to reach a number of identified lymph nodes ≥ 3 (Table 3)
As shown in Table 3, we found 5 micrometastasis in 3 patients (7,8% of all captured nodes, 15% of all cases) and 4 macrometastasis in 2 patients (6,2% of alla nodes, 10% of all cases).So, we avoided ALND in 15/20 patients (75% of all cases).
In one case we have found 2 macrometastatic nodes captured exclusively by Magtrace and not by technetium, while in another case we founded absence of uptake with both the tracers and so we performed axillary lymphadenectomy with subsequent definitive histological examination documenting the presence of two micrometastases. In the other metastatic case both tracers had identified the involved lymph nodes. We did not detect cases with isolated tumor cells (Table 3).
According to identification methods, N° 23 nodes (36% of all nodes) were identified through only SPIO, N° 41 with both tracers (64%), whereas 0 nodes were identified exclusively by tc99 (Figure 1)
4. Discussion
Researchers have investigated different ways to lower the SLN FNR after NAC in those patients with initially clinically positive axillary nodes. It has been accepted that a FNR of 10% is oncologically safe to avoid ALND in clinically node negative patients in the adjuvant setting, so similarly, in the studies after NAC a cut-off value of 10% has also been established to accept the validity of the technique, because we are lacking of long-term follow up on patients with clinically positive axilla and SLN after NAC. Many International studies showed how the use of a second tracer in association the standard techniques (Tc99) imporve the number of captured nodes (> 3) with a consensual reduction of FNR. SENTINA trial is a four arm prospective, multicenter study of the use of SLN in different timing in the neoadjuvant setting. In those patients with clinically node positive after NAC those converted to node negative underwent SLNB (Arm C: 592 patients) and those nodes that remained positives after NAC underwent an ALND (Arm D: 123 patients). FNR in Arm C were dependent on number of SLNs excised, 24.3% for removal of 1 SLN, 18.5% for 2 SLNs and <10% for >3 SLNs, similar to the reported data from ACOSOG Z0171. The authors found that using dual tracer (blue dye+Tc99) FNR were lower than using radiocolloid only (8.6% versus16%). The third study (SN FNAC study) evaluated the feasibility and accuracy of SLN after NAC in 153 patients with cytologically proven node positive breast cancer. The SLN IR was 87.6%, and the FNR was 9.6%. When they considered ypN0(i+) as a positive node, FNR was 8.4%. Similar to the other studies, when 2 or more SLNs were removed, FNR dropped to 4.9%.(Table 1). According to type of tracer used in association of the standard SNLB technique, the use of vital dyes such as blue dye and indocyanine green (ICG) is widespread. ICG is a low molecular weight organic molecule that has been approved by US FDA and EMA for SNLs detection because it fluoresces in the NIR spectrum. A recent single arm prospective studies in 821 patients with clinically node negative disease has seen a 99,8% of IR of SLN for ICG when combined with Tc99radiocollid. This study suggest that ICG optical imaging technique could be a replacement for blue dye in the standar dual mapping method, avoiding its potential drawbacks such as the need of considerable surgical experience with the procedure and occourance of the allergic reaction. Tsuyuki et al. stated that SLNs were detected in all clinically node-negative cases, whereas in clinically node-positive cases the identification rates (IRs) were 93.8%. Regardless of the node metastasis, the sentinel lymphatic pathways were detected without the influence of NAC in all cases. ICG did not reveal any systemic or even local side effects and the method was significantly less expensive than the scintigraphy method. Superparamagnetic iron oxide (SPIO) particles have been shown to be suitable for lymph node mapping using a magnetic probe for nodal detection following local sub-cutaneous injection. Clinical studies and meta-analyses have compared the SPIO technique with the standard mapping technique in breast cancer and have shown non-inferiority to the standard technique of technetiumlabeled colloid with or without blue dye. Magtrace (Endomagnetics Limited, Cambridge, UK), is a blackishbrown suspension of carboxydextran-coated SPIO particles. The particle diameter is designed for lymphatic uptake and filtering out in the sentinel lymph nodes (SLNs) draining from the primary site. In previous studies, Sienna (Endomagnetics Limited), an SPIO tracer requiring dilution with saline prior to injection, was used. To reduce the injected volume of tracer for improved patient comfort, a new formulation of the tracer was developed- Magtrace (formerly known as SiennaXP)- containing the same SPIO particles, but not requiring dilution. These magnetic particles are detected using Sentimag, a handheld magnetic probe analogous to a handheld gamma probe. Similarly to the ICG fluorescence technique, the higher SLN retrieval number and lower FNR for SPIO technique compared with conventional methods in the early breast cancer setting may make it a potentially optimal tracer for SLNB after NAC. However, no SPIO guided SLNB after NAC has been reported so far. To explore the feasibility of SPIO-guided SLNB after NAC in patients with biopsy-proven pretreatment positive ALNs who become clinically negative nodes post chemotherapy, a randomized trial has been initiated (NCT02249208). Enrolled patients are randomly assigned into three groups with different SLN detection methods: radiocolloid + blue dye, radiocolloid + SPIO, and SPIO alone. The primary outcome measure of this study is the FNR of each detection method. This is the first head-tohead randomized trial to compare the FNR between a novel SLN detection method and the currently standard dual detection method.
5. Conclusion
As demonstrated by our experience, still limited in number of cases, Magtrace® is a valid support in finding the LS post NAC, both in terms of non-inferiority compared to Tc99, and as a complementary means to the latter in the 'to help us find a number ≥ 3 of LS, essential for breaking down the FNR, as already widely demonstrated in the literature. Therefore, further prospective studies are needed on large series of cases able to clarify the "safety" of Magtrace®, also in the neoadjuvant setting. in our experience, Magtrace proves promising in finding more LS compared to the standard method, probably thanks to its peculiar molecular composition made of nanoparticles. In addition, in light of the increasingly numerous complete responses at the axillary level after NAC, we will enroll new patients in our protocol, for obtain data on a wider case.
|
Prospective trial |
Overall FNR |
By number of SLNs |
By detection tecniques |
|||
|
1 (%) |
2 (%) |
>3 (%) |
Single tracer |
Dual tracers |
||
|
SENTINA (arm C) |
14,2 (95% CI 9,9-19,4) |
24,3 |
18,5 |
7,3 |
16,0 |
8,6 |
|
ACOSOG Z1071 |
12,6 (95% CI 9,9-16,1) |
31,5 |
21 |
9,1 |
20,3 |
10,8 |
|
SN FNAC |
8,4 (95% CI 2,4-14,4) |
18,2 |
4,9 |
NR |
16,0 |
5,2 |
Table 1: False negative rates (FNR) for SLNB afetr coversation to clinically node-negative disease following NAC
|
N° |
% |
|
|
Pre-meopausal status |
12 |
60 |
|
Post-menopausal staus |
8 |
40 |
|
BRCA 1 mutation |
2 |
10 |
|
BRCA 2 mutation |
1 |
5 |
|
Mastectomy |
12 |
60 |
|
Conservative surgery |
8 |
40 |
|
Luminal A |
2 |
10 |
|
Luminal B |
5 |
25 |
|
Her2+ |
4 |
20 |
|
Triple negative |
4 |
20 |
|
pCR |
5 |
25 |
|
NODE STATUS: yp N0 |
15 |
75 |
|
yp N1mi |
3 |
15 |
|
yp N1 |
2 |
10 |
|
yp N2-N3 |
0 |
0 |
Table 2: Patients characteristics (N°20)
|
N°Cases |
20 |
|
Middle age |
51 (range 29-62 years) |
|
Detection rate Tc99 |
18/20 (90%) |
|
Detection rate Magtrace |
19/20 (95%) |
|
Concordance Rate |
19/20 (95%) |
|
N°LS/LpS Tc99+Magtrace® |
64 |
|
N°LS/LpS Tc99 |
29 |
|
N°LS/LpS Magtrace® |
52 |
|
N°LS/LpS micrometastases |
5 (7,8%) |
|
N°Pz con micrometastases |
3 (15%) |
|
N°LS/LpS macrometastases |
4 (6,2%) |
|
N° Pz macrometastases |
2 (10%) |
|
N°LS/LpS ITC |
0 |
p-value 0.05
Table 3: Results
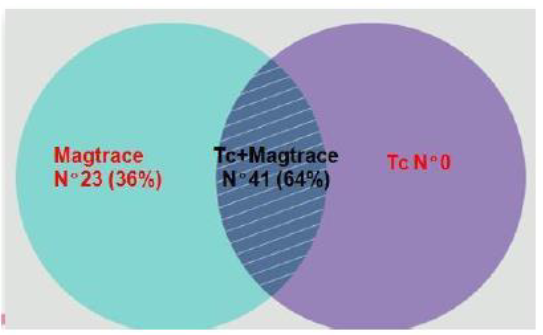
Figure 1: Results according to identification methods
References
- Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial The Lancet 15(2014): 1303-1310.
- Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the Almanac Trial J Natl Cancer Inst 98 (2006): 599-609.
- Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol 14 (2013): 609-618.
- Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with nodepositive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial JAMA 310 (2013): 1455-1461.
- Improved axillary evaluation following neoadjuvant therapy for patients with nodepositive breast cancer using selective evaluation of clipped nodes: Implementation of targeted axillary dissection. J Clin Oncol 34 (2016): 1072-1078.
- Price ER. Initial clinical experience with an inducible magnetic seed system for preoperative breast lesion localization. AJR Am J Roentgenol (2018).
- Sentinel lymph node biopsy after neoadjuvant treatment in breast cancer: Work in progress I.T. Rubio / EJSO 42 (2016): 326-332.
- Rubio IT. The superparamagnetic iron oxide is equivalent to the Tc99 radiotracer method for identifying the sentinel lymph node in breast cancer. Eur J Surg Oncol 41 (2015): 46-51.
- Yu JC. Role of sentinel lymphadenectomy combined with intraoperative ultrasound in the assessment of locally advanced breast cancer after neoadjuvant chemotherapy. Ann Surg Oncol 14 (2007): 174-180.
- Sentinel node biopsy using a magnetic tracer vs. standard technique: The SentiMAG Multicentre Trial. Ann Surg Oncol 21 (2014): 1237-1245.
- The Central-European SentiMag study: Sentinel lymph node biopsy with superparamagnetic iron oxide (SPIO) vs. radioisotope. Breast 23 (2014): 175-179.
- The superparamagnetic iron oxide is equivalent to the Tc99 radiotracer method for identifying the sentinel lymph node in breast cancer. Eur J Surg Oncol 41 (2015): 46-51.
- Piñero-Madrona. Superparamagnetic iron oxide as a tracer for sentinel node biopsy in breast cancer: a comparative non-inferiority study. Eur J Surg Oncol 41 (2015): 991-997.
- Chapman CH, Jagsi R. Postmastectomy radiotherapy after neoadjuvant chemotherapy: a review of the evidence. Oncology (Williston Park) 29 (2015): 657-666.
- Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384 (2014): 164-172.
- Alvarado MD, SentimagIC. A non-inferiority trial comparing superparamagnetic iron oxide versus technetium-99m and blue dye in the detection of axillary sentinel nodes in patients with early-stage breast cancer. Ann Surg Oncol 26 (2019): 3510-3516.
- Evolution in Sentinel lymph node biopsy in breast cancer. Crit Rev Oncol Hematol 123 (2018): 83-94.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 