Systematic Review of Flow Diversion for Giant and Paraophthalmic Aneurysms: Are Additional Coils Necessary
Hang Yu1, Khunsa Faiz1, Sudharsana Rao Ande1, Janice Linton2, Zul Kaderali3, Timo Krings4, Jai Shankar1*
1Department of Radiology, University of Manitoba, Winnipeg, Canada.
2Indigenous Health Librarian. Neil John Maclean Health Sciences Library, University of Manitoba, Winnipeg, Canada.
3Division of Neurosurgery, University of Manitoba, Winnipeg, Canada
4Department of Radiology, University of Toronto, Toronto, Canada
*Corresponding Author: Jai Jai Shiva Shankar, Department of Radiology, University of Toronto, Toronto, Canada
Received: 24 January 2023; Accepted: 09 February 2023; Published: 04 March 2024
Article Information
Citation: Hang Yu, Khunsa Faiz, Sudharsana Rao Ande, Janice Linton, Zul Kaderali, Timo Krings, Jai Shankar. Systematic Review of Flow Diversion for Giant and Paraophthalmic Aneurysms: Are Additional Coils Necessary. Journal of Surgery and Research. 7 (2024): 96-106.
View / Download Pdf Share at FacebookAbstract
Background: There is limited data regarding the use of flow diversion in treating giant or paraophthalmic aneurysms. It is also unclear whether coiling in combination with flow diversion improves outcomes.
Purpose: To evaluate the efficacy of using flow diverters (FD) with and without coiling for the treatment of intracranial aneurysms, especially in giant and paraophthalmic aneurysms.
Data Sources: Ovid Embase and Ovid Medline
Study Selection: Nine studies with 318 patients and 318 aneurysms were used. All were observational studies with five retrospective and four prospective.
Data Analysis: Studies were analyzed for patient and aneurysm characteristics, procedural details including success rate and complications, and follow-up imaging and clinical outcomes.
Data Synthesis: Procedure-related mortality rate was 3.5% (11/318). 6 months occlusion rate was 79.7% (149/187), 83.3% (5/6) for giant aneurysms, and 100% (8/8) for paraophthalmic aneurysms. There was no significant difference in occlusion rate in FD alone vs. FD with coils (p = 0.90). There did not seem to be a difference in morbidity, mortality, or clinical outcomes between FD alone and FD with coils.
Limitations: Small amounts of studies, heterogeneous study populations and types of aneurysm treated. All the included studies were observational with none having been randomized or including control groups. Significant heterogeneity in reporting outcomes and follow-up data.
Conclusions: Flow diverters alone are an effective way to treat giant and paraophthalmic aneurysms. The use of FD with coils was not shown to be superior to the use of FD alone.
Keywords
Intracranial aneurysms, Paraophthalmic aneurysms, Intracranial hemorrhage
Article Details
Abbreviations
AComA: Anterior communicating artery
eCLIP: endovascular clip system
FD: Flow diverter
FRED: Flow Re-Direction Endoluminal Device
ICH: Intracranial hemorrhage
mRRC: Modified Raymond-Roy Classification
mRS: modified Rankin Scale
OKM: O’Kelly-Marotta Grading scale
PComA: Posterior communicating artery
PED: Pipeline embolization device
RROC: Raymond-Roy Occlusion Classification
SILK: Silk Flow Diverter
SURPASS: Surpass Flow Diverter
Introduction
Intracranial aneurysms are primarily treated using either endovascular coiling or microsurgical clipping. Since the late 2000s, endoluminal flow diversion was introduced as an alternative treatment option [1]. Instead of intervening on the aneurysm sac with coiling and clipping, flow diversion targets the parent artery. The technique employs flow diverters (FD), endovascular mesh-like devices that are deployed within the parent artery overlying the artery/aneurysm interface. The FD, as its name suggests, diverts blood flow from the aneurysm sac resulting in intra-aneurysm flow stasis. This phenomenon simultaneously reduces sheer stress on the aneurysm wall and promotes intra-aneurysm thrombosis. Additionally, the mesh acts as a scaffold and promotes the propagation and development of endothelial and neointimal cells across the aneurysm neck allowing for reconstruction of the parent artery [2-5]. Flow diversion has comparable rates of aneurysm occlusion, no increase in morbidity or mortality, and similar clinical outcomes compared to coiling [6-11]. Flow diversion is still being more commonly used for aneurysms that are deemed difficult to treat with other endovascular techniques or may be deemed to have higher chances of recurrence [12-19]. While flow diversion is viewed as an alternative to coiling, adjunctive coiling is frequently used during endovascular flow diversion therapy [20-24]. Several FDs are currently available such as the PipelineTM embolization device (PED; Medtronic, Irvine, California), the Silk flow diverter (SILK; Balt Extrusion, Montmorency, France), the Flow Re-Direction Endoluminal Device (FRED; Microvention; Tustin, California) and the Surpass flow diverter (SURPASS; Fremont, CA). While flow diversion is becoming more commonplace, there is some evidence that flow diversion has higher efficacy for treatment of large or giant aneurysm in paraophthalmic location [25-29]. While flow diversion is becoming more commonplace, some studies have suggested the use of adjunctive coils to increase efficacy of flow diversion. It is unclear when to use coils in conjunction with flow diversion and when coils are used, how many coils should be used [28]. Our systematic review aims to answer whether the use of flow diverters alone, without the use of adjunctive coiling, are effective in treating intracranial aneurysms, with a focus on giant and paraophthalmic aneurysms.
Methods
Preliminary searching was done in the Cochrane Library and Scopus databases to identify existing systematic reviews specific to this question, but none were found. To identify relevant studies for inclusion in the analysis, comprehensive searches of the Medline and Embase databases were carried out in June 2019 using the OVID platform. A combination of keyword and MeSH or EMTREE subject headings was used (see online appendix for search strategies). We limited the search to articles published in English before June 2019 with the following inclusion criteria: 1) contained giant intercranial aneurysms (defined as ≥25 mm in diameter) or contained aneurysms of any size within the paraophthalmic region of the ICA, 2) treated with flow diverters with or without additional coils, and 3) had a sample of ≥5 patients.
Two independent screeners extracted the following information using a predetermined data abstraction form: study characteristics, patient demographics, aneurysm characteristics including size, location, and symptoms, flow diverter characteristics, endovascular procedure materials and details, complications of the endovascular procedure, follow-up and imaging, and clinical outcome and degree of aneurysmal occlusion. When available, complete occlusion rates for paraophthalmic aneurysms and giant aneurysm were tabulated separately.
Statistics
Descriptive statistics were performed to calculate mean and proportions. The complete occlusion rate for aneurysms treated with FD alone vs. FD with coils was compared using 2-way ANOVA with an alpha of 0.05. The principle summary measure was the risk ratio and study heterogeneity were measured by I2.
Results
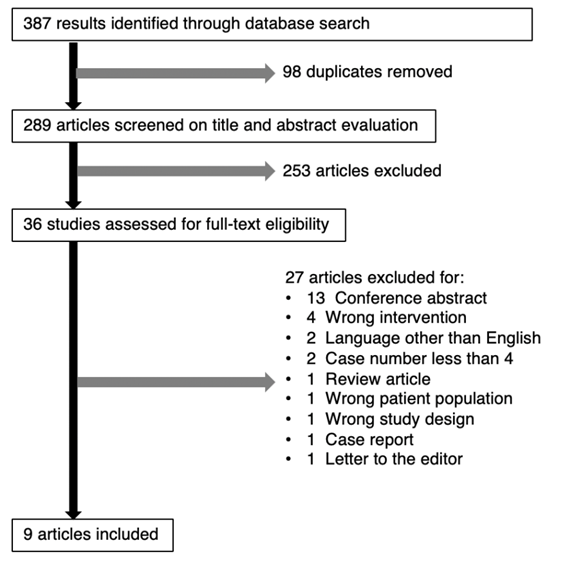
The results are summarized in figure 1. The initial search yielded 387 results, and 289 unique articles after duplicates were removed. Of the original 289 articles, only nine studies were eligible for inclusion within our systematic review [13-21]. A summary of the articles included can be found in table 1.
|
Title |
Author |
Year |
Journal |
Study Design |
Number of Patients |
Number of aneurysms |
|
Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the pipeline embolization device. |
Szikora et al. |
2010 |
American Journal of Neuroradiology |
Prospective |
18 |
19 |
|
Early postmarket results after treatment of intracranial aneurysms with the pipeline embolization device: A US multicenter experience |
Kan et al. |
2012 |
Neurosurgery |
Prospective |
56 |
58 |
|
Volume changes of extremely large and giant intracranial aneurysms after treatment with flow diverter stents |
Carneiro et al. |
2014 |
Neuroradiology |
Retrospective |
8 |
8 |
|
A novel flow-diverting device (Tubridge) for the treatment of 28 large or giant intracranial aneurysms: A single-center experience |
Zhou et al. |
2014 |
American Journal of Neuroradiology |
Prospective |
28 |
28 |
|
Endovascular treatment of unruptured aneurysms of cavernous and ophthalmic segment of internal carotid artery with flow diverter device Pipeline |
Jevsek et al. |
2016 |
Radiology and Oncology |
Retrospective |
15 |
15 |
|
Pipeline for uncoilable or failed aneurysms: 3-year follow-up result |
Becske et al. |
2017 |
Journal of Neurosurgery |
Prospective |
108 enrolled (107 treated) |
109 |
|
Usefulness of the pipeline embolic device for large and giant carotid cavernous aneurysms |
Miyachi et al. |
2017 |
Neurointervention |
Retrospective |
24 |
24 |
|
The second-generation eCLIPs Endovascular Clip System: initial experience |
Chiu et al. |
2018 |
Journal of Neurosurgery |
Retrospective |
33 |
25* |
|
Short-term efficacy of pipeline embolization device for treating complex intracranial aneurysms |
ReXiaTi et al. |
2018 |
Bio-Medical Materials and Engineering |
Retrospective |
29 |
32 |
*Chiu et al had fewer aneurysms than patients because the authors only characterized the 25 successfully treated patients who had 25 aneurysms.
Table 1: Studies included in the systematic review.
Four studies were prospective and five were retrospective. The nine studies yielded a total of 318 patients with 318 intracranial aneurysms. Patient and aneurysm details are shown in table 2. The sample size ranged from eight to 107 patients, and the number of aneurysms varied between 8 and 109.
|
Patients |
318 |
|
Female |
228/267 (85.4%) |
|
Mean Age |
57.7 (267*) |
|
Total number of aneurysms |
318 |
|
Giant (≥25 mm max. diameter) |
58/310 (18.7%) |
|
Paraophthalmic |
51/299 (17.1%) |
|
Anterior circulation |
283/318 (89.0%) |
|
Vertebrobasilar circulation |
35/318 (11.0%) |
|
Saccular |
128/141 (90.8%) |
|
Fusiform |
11/141 (7.8%) |
|
Wide-necked (≥4mm or dome:neck ratio ≤1) |
168/171 (98.2%) |
|
Unruptured |
306/318 (95.0%) |
|
Ruptured |
12/318 (7 acute, 5 prior; 3.8%) |
|
Clinical presentation |
|
|
Asymptomatic |
99/285 (34.7%) |
|
Symptomatic |
186/285 (65.3%) |
*Of the 267 patients that had their ages known.
Table 2: Patient and aneurysm characteristics
Patient characteristics such as age and sex, and aneurysm characteristics including location, size, and type were not available in all studies. While Becske et al. did not characterize their patient population or aneurysm characteristics, the study was a follow-up to their 2013 study which indicated 96 female patients, 35 paraophthalmic aneurysms and 22 giant aneurysms. Carneiro et al. did not provide maximum diameters for the 8 aneurysms they treated but stated that they were either “extremely large” (≥20 mm) or giant (≥25 mm) [4,15]. For aneurysms where maximum diameter and location were known, 58 of 310 (18.7%) were giant aneurysms and 51 of 299 (17.1%) were paraophthalmic aneurysms.
Two hundred eighty-three (89.0%) and 35 (11.0%) of the aneurysms originated from the anterior and vertebrobasilar circulations respectively. Individual aneurysm characteristics were not known for all aneurysms included. Out of 141 aneurysms whose shape were known, 128 (90.8%) were saccular and 11 (7.8%) were fusiform. Out of 171 aneurysms whose neck widths were known, 168 (98.2%) were wide-necked defined as ≥4 mm neck width or dome:neck ratio ≤1. There were 25 (7.9%) bifurcation aneurysms, all of which were from Chiu et al. Both ruptured and unruptured aneurysms were studied; there were 306 (96.2%) unruptured aneurysms and 12 (3.8%) ruptured ones, with seven (2.2%) being acute ruptures and five (1.6%) being previous ruptures.
The 186 (65.3%) symptomatic patients presented with headache, visual disturbances, ocular motor palsies, seizures, hemiparesis, and SAH. Two studies, Becske et al. and Miyachi et al. used the modified Rankin Scale (mRS) for neurological disability to categorize symptoms [18,19].
A variety of FDs were used by the authors and their details are listed in table 3. Overall, 262 (82.4%) aneurysms were treated with PED, 3 (0.9%) with SILK, 28 (8.8%) with Tubridge, and 25 (7.9%) with eCLIP. No aneurysm was treated with two different FDs.
|
Type of flow diverter |
PED: 7 studies. 82.4% (262/318) |
|
SILK: 1 study. 0.94% (3/318) |
|
|
Tubridge: 1 study. 8.8% (28/318) |
|
|
eCLIP: 1 study. 7.9% (25/318) |
|
|
Flow diverters alone |
74.5% (213/286) |
|
Flow diverters with coils |
25.2% (72/286) |
|
Flow diverters with additional treatment other than coils |
Prior WEB: 0.35% (1/286)* |
|
Prior surgical clip: 0.35% (1/286) |
|
|
Number of flow diverters deployed |
281 for 184 aneurysms |
|
Successful deployment/treatment |
(FDs deployed): 96.9% (220/227) |
|
(Patients treated): 83.3% (180/216) |
|
|
Post-balloon reconstruction |
|
|
(FDs deployed): 99.6% (226/227) |
|
|
(Patients treated): 86.1% (183/216) |
|
|
Side branches covered |
104 FDs covered 89 side branches |
|
·Ophthalmic: 59 |
|
|
· AComA: 1 |
|
|
· PComA: 16 |
|
|
·Anterior choroidal: 4 |
|
|
· PICA: 5 |
|
|
·AICA: 1 |
|
|
·Meningohypophyseal: 2 |
|
|
·Frontal: 1 |
*WEB: Woven EndoBridge Aneurysm Embolization system
Table 3: Flow diverter and endovascular procedure characteristics
Treatment characteristics can also be found on table 3. There were 286 aneurysms that had data on whether they were treated with FD alone or with FD in combination with coils. Of the 286, 213 (74.5%) were treated with FD alone and 72 (25.2%) were treated with FD with coils, including aneurysms previously coiled. One out of 286 was treated with FD alone with prior microsurgical clipping. ReXiaTi et al. treated 31 of their 32 aneurysms with 30 PEDs, but it was unclear how many aneurysms were treated with PED alone versus PED with coils as the authors only state that 12 patients were treated with PED alone and 17 were treated with PED with coils [21]. From the available data, 281 FDs were deployed to treat 184 aneurysms giving a ratio of around 1.5 FDs per aneurysm. The range for number of FDs deployed per aneurysm was 1/3 to 15. In one case, 3 aneurysms were treated with a single PED.
Initial success was documented as either number of patients treated successfully, or number of FDs deployed successfully depending on the study. Initial technical success occurred in 220 of 227 (96.9%) attempted FD deployments. The number was 226 (99.6%) after adjunctive balloon angioplasty for complete opening of the FD. Treatment success occurred in 180 of 216 (83.3%) patients initially and was 183 (84.7%) post balloon assistance.
Three studies provided data regarding side branches occluded by deployment of the FD. Overall, 104 FDs covered 89 side branches and details are available in table 3. Occlusion of side branches were not associated with any neurological deficits or ischemic events.
There were 96 (30.2%) patients who had complications (Table 4). 14 (4.4%) had hemorrhagic and 20 had (6.3%) ischemic complications. Other complications included worsening headaches, worsening cranial neuropathies, bleeding, vision changes, seizures, new aneurysm formation (not a recurrence), and infection. Aneurysm recurrences were not reported in any study. The procedure-related mortality rate is 3.5% (11/318).
|
Complications (including death) |
Total: 30.2% (96/318) |
|
Ischemic and hemorrhagic complications: 10.7% (34/318): 4.4% (14/318) hemorrhagic and 6.3% (20/318) ischemic |
|
|
· 9/34 fatal. |
|
|
· 5/34 permanent deficits |
|
|
· 20/34 no permanent deficits |
|
|
Mortality |
Total: 14/318. Procedure-related 3.5% (11/318) |
|
· ICH due to rupture of target aneurysm: 8 |
|
|
· ICH unrelated to rupture of target aneurysm: 1 |
|
|
· Mass effect by target aneurysm: 1 |
|
|
· Rapid neurological deterioration post-treatment: 1 |
|
|
· Non-procedure related: 3 |
|
|
Perioperative: 7/14 |
|
|
Delayed: 7/14 |
|
|
Perioperative (≤30 days post-procedure) deaths and hemorrhagic/ischemic complications |
Deaths: 7 (6 aneurysm rupture, 1 ICH unrelated to rupture) |
|
Hemorrhagic complications: 12 |
|
|
· Aneurysm rupture: 7 (6 fatal; 1 full recovery) |
|
|
· ICH (unrelated to rupture): 5 (1 fatal; 2 full recovery; 2 permanent deficits) |
|
|
Ischemic complications: 18 |
|
|
· TIA: 11 |
|
|
· Ischemic stroke: 5 (2 permanent deficits) |
|
|
· Retinal artery occlusion: 1 (permanent visual field deficits) |
|
|
· In-stent thrombosis: 1 (transient hemiparesis) |
|
|
Delayed (>30 days post-procedure) deaths and hemorrhagic/ischemic complications |
Deaths: 7 (2 aneurysm rupture, 1 worsening mass effect, 1 rapid neurological deterioration, 3 unrelated) |
|
Hemorrhagic complications: 2 |
|
|
· Aneurysm rupture: 2 (2 fatal) |
|
|
Ischemic complications: 2 |
|
|
· In-stent thrombosis: 2 (no permanent deficits) |
Table 4: Complications from flow diverter treatment
All studies included imaging and clinical follow-up, although there was significant heterogeneity in follow-up duration and documenting. Follow-up times ranged from 3 months to 48 months at various intervals at the discretion of the clinician. Five studies included scheduled follow-ups while the other studies only reported on the last follow-up each patient had. For the purpose of this review, follow-up scheduling initially expressed in days or years were all converted to months (e.g. a follow-up time of 180 days, ½ a year, and 6 months were treated the same).
Follow-up imaging included MRA, CTA, and DSA. Occlusion was measured using the Raymond-Roy occlusion criteria (RROC) in two studies, the modified Raymond-Roy occlusion criteria (mRRC) for one study, and the O’Kelly-Marotta Grading scale (OKM) for one study. Clinical outcomes were measured using the modified Rankin Scale (mRS) in two studies while the others used descriptors such as “no deficit/cured,” “improved,” “unchanged” or “worsened.” Follow-up data is summarized in table 5. When available, separate data was given for FD alone vs. FD with coils, and for giant and paraophthalmic aneurysms.
|
Follow-up |
|
|
Immediate post-procedure |
Imaging (93 aneurysms) |
|
Complete occlusion: 8/93 (8.6%) |
|
|
Incomplete occlusion: 82/93 (88.2%) |
|
|
·Neck remnant/RROC Class II/mRRC Class II: 10 |
|
|
·Residual aneurysm/RROC Class III/mRRC Class IIIa and IIIb: 58 |
|
|
·Incomplete unspecified: 14 |
|
|
No change: 3/92 (3.2%) |
|
|
FD alone (34 aneurysms): |
|
|
·Complete occlusion: 1/34 (2.9%) |
|
|
·Incomplete occlusion: 30/34 (88.2%) |
|
|
·No change: 3/34 (8.8%) |
|
|
FD with coils (18 aneurysms): |
|
|
·Complete occlusion: 0/18 (0%) |
|
|
·Incomplete occlusion: 18/18 (100%) |
|
|
3 months |
Imaging (20 aneurysms): |
|
Complete occlusion: 13/20 (65%) |
|
|
Incomplete occlusion: 7/20 (35%) |
|
|
·Neck remnant/RROC Class II/mRRC Class II: 5 |
|
|
·Residual aneurysm/RROC Class III/mRRC Class IIIa and IIIb: 2 |
|
|
6 months |
Imaging (187 aneurysms): |
|
Complete occlusion: 149/187 (79.7%) |
|
|
Incomplete occlusion: 35/187 (18.7%) |
|
|
·Incomplete unspecified: 10 |
|
|
·Neck remnant/RROC Class II/mRRC Class II: 18 |
|
|
·Residual aneurysm/RROC Class III/mRRC Class IIIa and IIIb: 7 |
|
|
Cannot determine: 3/187 (1.6%) |
|
|
Clinical (185 patients): |
|
|
mRS (available 125 patients) |
|
|
·mRS ≤1: 118/125 (94.4%) |
|
|
No deficits: 12/84 (14.3%) |
|
|
Improved: 41/84 (48.8%) |
|
|
Unchanged: 18/84 (21.4%) |
|
|
Worsened: 13/84 (15.5%) |
|
|
FD alone (152 aneurysms) |
|
|
·Complete occlusion: 117/152 (77.0%) |
|
|
FD with coils (10 aneurysms) |
|
|
·Complete occlusion: 10/10 (100%) |
|
|
Giant (6; all treated with FD alone) |
|
|
·Complete occlusion: 5/6 (83.3%) |
|
|
Paraophthalmic (8 aneurysms) |
|
|
·Complete occlusion: 8/8 (100%) |
|
|
12 months |
Imaging (91 aneurysms): |
|
Complete occlusion: 79/91 (86.8%) |
|
|
Incomplete occlusion: 12/91 (13.2%) |
|
|
·Incomplete unspecified: 2 |
|
|
·Neck remnant/RROC Class II/mRRC Class II: 5 |
|
|
·Residual aneurysm/RROC Class III/mRRC Class IIIa and IIIb: 5 |
|
|
FD alone (91 aneurysms) |
|
|
·Complete occlusion: 79/91 (86.8%) |
|
|
14 months |
Imaging (15 aneurysms): |
|
Complete occlusion: 15/15 (100%) |
|
|
Clinical (15 patients): |
|
|
No deficits: 15/15 (100%) |
|
|
FD alone (13 aneurysms; 13 patients) |
|
|
·Complete occlusion: 13/13 (100%) |
|
|
·No deficits: 13/13 (100%) |
|
|
FD with coils (1 aneurysm; 1 patient) |
|
|
·Complete occlusion: 1/1 (100%) |
|
|
·No deficits: 1/1 (100%) |
|
|
Paraophthalmic (8 aneurysms; 8 patients) |
|
|
·Complete occlusion: 8/8 (100%) |
|
|
·No deficits: 8/8 (100%) |
|
|
36 months |
Imaging (76 aneurysms): |
|
Complete occlusion: 71/76 (93.4%) |
|
|
Incomplete occlusion: 4/76 (5.3%) |
|
|
·Neck remnant/RROC Class II/mRRC Class II: 2 |
|
|
·Residual aneurysm/RROC Class III/mRRC Class IIIa and IIIb: 2 |
|
|
Cannot determine: 1/76 (1.3%) |
|
|
Clinical (89 patients): |
|
|
mRS ≤1: 80/89 (89.9%) |
|
|
·mRS 0: 60/89 (67.4%) |
|
|
·mRS 1: 20/89 (22.5%) |
|
|
mRS 2: 2/89 (2.2%) |
|
|
mRS 3: 1/89 (1.1%) |
|
|
mRS 4: 2/89 (2.2%) |
|
|
mRS 6: 4/89 (4.5%) |
|
|
FD alone (76 aneurysms) |
|
|
·Complete occlusion: 71/76 (93.4%) |
|
|
Latest (Range: 3 to 48 months) |
Imaging (69 aneurysms; mean 10.7 months): |
|
Complete occlusion: 26/69 (37.7%) |
|
|
Incomplete occlusion: 43/69 (62.3%) |
|
|
·Incomplete unspecified: 16 |
|
|
·Neck remnant/RROC Class II/mRRC Class II: 16 |
|
|
·Residual aneurysm/RROC Class III/mRRC Class IIIa and IIIb: 6 |
|
|
Unchanged: 3/69 (4.3%) |
|
|
Increased: 2/69 (2.9%) |
|
|
Clinical (28 patients; mean 19.0 months): |
|
|
No deficits: 13/28 (46.4%) |
|
|
Improved: 6/28 (21.4%) |
|
|
Unchanged: 9/28 (32.1%; 5 transient worsening) |
|
|
FD alone (10 aneurysms) |
|
|
·Complete occlusion: 7/10 (70%) |
|
|
FD with coils (23 aneurysms) |
|
|
·Complete occlusion: 12/23 (52.2%) |
Table 5: Follow-up imaging and clinical findings
Immediately post-procedure, aneurysms treated with FD alone had a complete occlusion rate of 2.9% (1/34) versus 0% (0/18) for those treated with FD and coils. Reported complete occlusion rate for FD alone was 77.0% (117/152) at 6 months, 86.8% (79/91) at 12 months, 100% (13/13) at 14 months, and 93.4% (71/76) at 36 months. Complete occlusion rate for FD with coils was 100% (10/10) at 6 months and remained 100% at 14 months (1/1). There was no significant difference in occlusion rate between FD with coils vs FD and alone at 6 months (RR: 0.99; 95% CI: 0.82-1.19; I2: 0%; p = 0.90). The 13 patients treated with FD alone at 14 months follow-up were all symptom-free. One patient treated with FD and coils at 14 months follow-up was symptom free.
At 6 months, the complete occlusion rate for giant aneurysms was 83.3% (5/6) and was 100% (8/8) for paraophthalmic aneurysms. All the giant aneurysms were treated with FD alone. At 14 months follow-up, 100% (8/8) of patients with known paraophthalmic aneurysms were reported to be symptom-free.
A cohort of 69 aneurysms that only had their latest imaging follow-up reported had a mean follow-up time of 10.7 months. The complete occlusion rate was 37.7% (26/69). Treatment with FD alone had a complete occlusion rate of 70% (7/10) and treatment with FD and coils had a complete occlusion rate of 52.2% (12/23). There was no significant difference between FD with coils and FD alone (RR: 1.69; 95% CI: 0.30 - 9.57; I2: 46%; p = 0.55). There were 28 patients that only had their latest clinical follow-up reported; they had a mean follow-up time of 19.0 months. Of this cohort, 46.4% (13/28) had no deficits, 21.4% (6/28) had improved, and 32.1% (9/28) were unchanged, though 55.6% (5/9) of unchanged patients did experience transient worsening.
Discussion
Our review reported the results of nine studies with a total of 318 patients with 318 aneurysms. The results from this review corroborate previous research regarding the efficacy of FDs in treating intracranial aneurysms. A meta-analysis by Brinjikji et al. which included 1451 patients with 1654 intracranial aneurysms treated with flow-diverter devices found a 6-month occlusion rate of 76%, including a 6-month occlusion rate of 76% for treated giant aneurysms [1]. Procedure-related permanent morbidity was 5% and mortality was 4% [1]. We found a 6-month occlusion rate of 79.7% and a procedure-related mortality rate of 3.5%. Giant aneurysms had a 6-month occlusion rate of 83.3% and paraophthalmic aneurysms had a 6-month occlusion rate of 100%. There was no aneurysm recurrence mentioned in any of the included studies.
Few studies have looked at the use of FDs alone versus FDs with adjunctive coiling. There have been observations of faster occlusion, lower morbidity, and lower incidence of aneurysm rupture with adjunctive coiling [24,25]. We were able to compare the complete occlusion rates for aneurysms treated by FD alone and FD with coils at 6 months (p = 0.90) and 10.7 months (p = 0.55) and found no significant difference. There did not seem to be a difference in morbidity or mortality in the two groups, and clinical outcomes were also similar.
The rate of ischemic and hemorrhagic complications post-procedure was 10.7%, with 6.3% ischemic and 4.4% hemorrhagic. This is similar to other studies which have found ischemic and hemorrhagic complication rates of 5-8% and 2-5% respectively [1,26,27]. 90.9% of all procedure-related deaths were hemorrhagic complications, and 1.6% of patients had permanent deficits from ischemic or hemorrhagic complications post-procedure. Our review also corroborated several other known complications of flow diverters such as side branch and perforator occlusion, perianeurysmal edema, and in-stent thrombosis [2]. Occlusion of perforators and side branches was seen but was clinically silent in all cases. The transient worsening of headaches, cranial neuropathies, and mass effect was attributed in some of our included studies to perianeurysmal edema. Finally, in-stent thrombosis was observed in three patients all presenting with ischemic symptoms such as hemiparesis. None of the three had permanent deficits.
Limitations
There are several limitations to our systematic review. First, all the included studies were observational with the majority of them being retrospective. There were no randomized studies or any with control groups. Selection bias could have been introduced to the sample as the majority of the included studies had small sample sizes, with an average sample size of 35 and with only two studies having a sample size of over 50. Several of the studies also only provided experiences at a single centre.
There was a strong gender bias as 85.4% of the patients were female, although female sex is a risk factor associated with intracranial aneurysms. Additionally, some of the included articles such as Becske et al. and Chiu et al. studied populations with complex and clinically challenging aneurysms, such as bifurcation aneurysms, wide-necked aneurysms, and uncoilable aneurysms [18,20]. As such, the results from those studies may not be generalizable to all patient populations. The complex patient population could explain why Chiu et al. only achieved a treatment success rate of 75.8% whereas all other studies had >90% [20].
Another limitation was that not all of the studies provided all relevant data regarding patient and aneurysm characteristics, parent vessel characteristics, procedure details, and follow-up details. When available, there was no consistent method for data presentation and statistics which made it difficult to compile the data. There were also large amounts of heterogeneity when it came to procedure and follow-up documentation. This was problematic when assessing follow-up data as the studies all had varied follow-up intervals. The follow-up outcome measures also differed widely between studies. Some had aneurysm-centric outcome measures (e.g. number of aneurysms successfully treated) while some had patient-centric measures (e.g. number of patients successfully treated). Overall, the heterogeneity of the included studies made it difficult to compile and compare data.
Conclusion
Flow diverters alone are an effective way to treat intracranial aneurysms, including giant intracranial aneurysms and paraophthalmic aneurysms. The use of coiling in addition to flow diverter for the treatment of intracranial aneurysms has not been shown to be superior to the use of flow diverters alone.
References
- Brinjikji W, Murad MH, Lanzino G, et al. Endovascular treatment of intracranial aneurysms with flow diverters: a meta-analysis. Stroke 44 (2013): 442-447.
- Alderazi YJ, Shastri D, Kass-Hout T, et al. Flow Diverters for Intracranial Aneurysms. Stroke Res Treat (2014).
- Molyneux AJ, Kerr RSC, Yu LM, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 366 (2005): 809-817.
- Becske T, Kallmes DF, Saatci I, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology 267 (2013): 858-868.
- Pierot L. Flow diverter stents in the treatment of intracranial aneurysms: Where are we? J Neuroradiol 38 (2011): 40-46.
- Vlak MH, Algra A, Brandenburg R, et al. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol 10 (2011): 626-636.
- Moret J, Cognard C, Weill A, et al. The “Remodelling Technique” in the Treatment of Wide Neck Intracranial Aneurysms. Angiographic Results and Clinical Follow-up in 56 Cases. Interv Neuroradiol 3 (1997): 21-35.
- Chalouhi N, Jabbour P, Singhal S, et al. Stent-Assisted Coiling of Intracranial Aneurysms. Stroke 44 (2013): 1348-1353.
- Awad AJ, Mascitelli JR, Haroun RR, et al. Endovascular management of fusiform aneurysms in the posterior circulation: the era of flow diversion. Neurosurgical Focus 42 (2017): E14.
- Rinkel Gabriel JE, Djibuti M, Algra A, et al. Prevalence and Risk of Rupture of Intracranial Aneurysms. Stroke 29 (1998): 251-256.
- Brown RD, Broderick JP. Unruptured intracranial aneurysms: epidemiology, natural history, management options, and familial screening. The Lancet Neurology 13 (2014): 393-404.
- Thompson B, Gregory, Brown RD, et al. Guidelines for the management of patients with unruptured Intracranial Aneurysms. Stroke 46 (2015): 2368-400.
- Szikora I, Berentei Z, Kulcsar Z, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the pipeline embolization device. AJNR Am J Neuroradiol 31 (2010): 1139-1147.
- Kan P, Siddiqui AH, Veznedaroglu E, et al. Early postmarket results after treatment of intracranial aneurysms with the pipeline embolization device: a U.S. multicenter experience. Neurosurgery 71 (2012): 1087-1088.
- Carneiro A, Rane N, Küker W, et al. Volume changes of extremely large and giant intracranial aneurysms after treatment with flow diverter stents. Neuroradiology 56 (2014): 51-58.
- Zhou Y, Yang PF, Fang YB, et al. A novel flow-diverting device (Tubridge) for the treatment of 28 large or giant intracranial aneurysms: a single-center experience. AJNR Am J Neuroradiol 35 (2014): 2326-2333.
- Jevsek M, Mounayer C, Seruga T. Endovascular treatment of unruptured aneurysms of cavernous and ophthalmic segment of internal carotid artery with flow diverter device Pipeline. Radiol Oncol 50 (2016): 378-384.
- Becske T, Potts MB, Shapiro M, et al. Pipeline for uncoilable or failed aneurysms: 3-year follow-up results. J Neurosurg 127 (2017): 81-88.
- Miyachi S, Hiramatsu R, Ohnishi H, et al. Usefulness of the Pipeline Embolic Device for Large and Giant Carotid Cavernous Aneurysms. Neurointervention 12 (2017): 83-90.
- Chiu AH, De Vries J, O’Kelly CJ, et al. The second-generation eCLIPs Endovascular Clip System: initial experience. J Neurosurg 128 (2018): 482-489.
- ReXiaTi N, AiKeReMu R, KaDeEr K, et al. Short-term efficacy of pipeline embolization device for treating complex intracranial aneurysms. Biomed Mater Eng 29 (2018): 137-146.
- Bender MT, Jiang B, Campos JK, et al. Single-stage flow diversion with adjunctive coiling for cerebral aneurysm: outcomes and technical considerations in 72 cases. Journal of NeuroInterventional Surgery 10 (2018): 843-850.
- Chalouhi N, Tjoumakaris S, Starke RM, et al. Comparison of Flow Diversion and Coiling in Large Unruptured Intracranial Saccular Aneurysms. Stroke 44 (2013): 2150-2154.
- Park MS, Kilburg C, Taussky P, et al. Pipeline Embolization Device with or without Adjunctive Coil Embolization: Analysis of Complications from the IntrePED Registry. AJNR Am J Neuroradiol 37 (2016): 1127-1131.
- Yang C, Vadasz A, Szikora I. Treatment of ruptured blood blister aneurysms using primary flow-diverter stenting with considerations for adjunctive coiling: A single-centre experience and literature review. Interv Neuroradiol 23 (2017): 465-476.
- Zhou G, Su M, Yin YL, et al. Complications associated with the use of flow-diverting devices for cerebral aneurysms: a systematic review and meta-analysis. Neurosurg Focus 42 (2017): E17.
- Pierot L, Spelle L, Berge J, et al. Feasibility, complications, morbidity, and mortality results at 6 months for aneurysm treatment with the Flow Re-Direction Endoluminal Device: report of SAFE study. Journal of NeuroInterventional Surgery 10 (2018): 765-770.
- Shankar JJS, Vandorpe R, Pickett G, et al. SILK flow diverter for treatment of intracranial aneurysms: initial experience and cost analysis. J Neurointerv Surg 5 (2013): 11-15.
- Shankar JJS, Tampieri D, Iancu D, et al. SILK flow diverter for complex intracranial aneurysms: a Canadian registry. Journal of NeuroInterventional Surgery 8 (2016): 273-278.
Appendix
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily <1946 to June 26, 2019>
Search Strategy:
--------------------------------------------------------------------------------
1 (Giant adj5 aneurysm*).mp. (4575)
2 Intracranial Aneurysm/ (26585)
3 giant.mp. (84277)
4 (Eye* or paraophthalm* or ophthalm* or periocular or ocular or extraocular or orbital or vision* or blind* or optic*).mp. (1373920)
5 (Flow* or diver* or coil*).mp. (1506506)
6 *Embolization, Therapeutic/ (21561)
7 (hydrocoil* or guglielmi*).mp. (858)
8 2 and 3 (1997)
9 1 or 8 (4704)
10 5 or 6 or 7 (1520648)
11 4 and 9 and 10 (135)
***************************
Database: Embase <1974 to 2019 Week 25>
Search Strategy:
--------------------------------------------------------------------------------
1 (Giant adj5 aneurysm*).mp. (5783)
2 exp intracranial aneurysm/ (31663)
3 giant.mp. (95137)
4 (Eye* or paraophthalm* or ophthalm* or periocular or ocular or extraocular or orbital or vision* or blind* or optic*).mp. (1582413)
5 (Flow* or diver* or coil*).mp. (2005521)
6 coil embolization/ (11588)
7 (hydrocoil* or guglielmi*).mp. (1381)
8 2 and 3 (2215)
9 1 or 8 (5999)
10 5 or 6 or 7 (2005575)
11 4 and 9 and 10 (252)
***************************


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 