The Comparison of Scintigraphic and Ultrasonographic Evaluation Criteria of Thyroid Nodules with Histopathologic Findings
Seracettin Egin*
Department of General Surgery, University of Health Sciences, Okmeydani Education and Research Hospital, Istanbul, Turkey
*Corresponding Author: Dr. Seracettin Egin, Department of General Surgery, University of Health Sciences, Okmeydani Education and Research Hospital, Istanbul, Turkey
Received: 03 June 2018; Accepted: 18 June 2018; Published: 22 June 2018
Article Information
Citation: Seracettin Eğin. The Comparison of Scintigraphic and Ultrasonographic Evaluation Criteria of Thyroid Nodules with Histopathologic Findings. Journal of Surgery and Research 1 (2018): 42-52.
View / Download Pdf Share at FacebookAbstract
The aim of the study is to prospectively investigate the common malignancy criteria of nodules with the inclusion of malignancy potential in palpable thyroid nodules by imaging scintigraphically and sonographically. The study was conducted on 55 patients with palpable thyroid nodules including the suspicions of malignancy. The evidences of the scintigraphic and ultrasonographic images were evaluated prospectively. The evidences were compared with histopathologic results after surgical intervention. The sensitivity and specificity of cold nodules to malignancy were found as100% and 82% respectively. In ultrasonography (USG), a comparison was performed between two groups of patients according to the dominant nodule diameter of each patient, and the diameter was significantly larger in the malignant group. The sensitivity to determine malignancy for the solid and complex structure of the nodule was 60% and 40% respectively. The specificity to determine malignancy was 26% for solid nodule and was 82% for the complex nodule. The patients with only one malignancy findings at USG were compared according to groups and a significant difference was not found. However, the patients with two or three malignancy findings at USG were compared according to groups and significant differences were found . The sensitivity and specificity for the patients with two malignancy findings at USG were found as 100% and 72% respectively. The combination of two or more of these USG findings may suggest an increased risk of thyroid cancer and fine needle aspiration biopsy is still the most important diagnostic method in the diagnosis of thyroid malignancies.
Keywords
Thyroid nodule, Thyroid scintigraphy, Thyroid ultrasonography, Thyroid histopathology
Thyroid nodule articles Thyroid nodule Research articles Thyroid nodule review articles Thyroid nodule PubMed articles Thyroid nodule PubMed Central articles Thyroid nodule 2023 articles Thyroid nodule 2024 articles Thyroid nodule Scopus articles Thyroid nodule impact factor journals Thyroid nodule Scopus journals Thyroid nodule PubMed journals Thyroid nodule medical journals Thyroid nodule free journals Thyroid nodule best journals Thyroid nodule top journals Thyroid nodule free medical journals Thyroid nodule famous journals Thyroid nodule Google Scholar indexed journals Thyroid scintigraphy articles Thyroid scintigraphy Research articles Thyroid scintigraphy review articles Thyroid scintigraphy PubMed articles Thyroid scintigraphy PubMed Central articles Thyroid scintigraphy 2023 articles Thyroid scintigraphy 2024 articles Thyroid scintigraphy Scopus articles Thyroid scintigraphy impact factor journals Thyroid scintigraphy Scopus journals Thyroid scintigraphy PubMed journals Thyroid scintigraphy medical journals Thyroid scintigraphy free journals Thyroid scintigraphy best journals Thyroid scintigraphy top journals Thyroid scintigraphy free medical journals Thyroid scintigraphy famous journals Thyroid scintigraphy Google Scholar indexed journals Thyroid ultrasonography articles Thyroid ultrasonography Research articles Thyroid ultrasonography review articles Thyroid ultrasonography PubMed articles Thyroid ultrasonography PubMed Central articles Thyroid ultrasonography 2023 articles Thyroid ultrasonography 2024 articles Thyroid ultrasonography Scopus articles Thyroid ultrasonography impact factor journals Thyroid ultrasonography Scopus journals Thyroid ultrasonography PubMed journals Thyroid ultrasonography medical journals Thyroid ultrasonography free journals Thyroid ultrasonography best journals Thyroid ultrasonography top journals Thyroid ultrasonography free medical journals Thyroid ultrasonography famous journals Thyroid ultrasonography Google Scholar indexed journals Thyroid histopathology articles Thyroid histopathology Research articles Thyroid histopathology review articles Thyroid histopathology PubMed articles Thyroid histopathology PubMed Central articles Thyroid histopathology 2023 articles Thyroid histopathology 2024 articles Thyroid histopathology Scopus articles Thyroid histopathology impact factor journals Thyroid histopathology Scopus journals Thyroid histopathology PubMed journals Thyroid histopathology medical journals Thyroid histopathology free journals Thyroid histopathology best journals Thyroid histopathology top journals Thyroid histopathology free medical journals Thyroid histopathology famous journals Thyroid histopathology Google Scholar indexed journals clinically palpable nodules articles clinically palpable nodules Research articles clinically palpable nodules review articles clinically palpable nodules PubMed articles clinically palpable nodules PubMed Central articles clinically palpable nodules 2023 articles clinically palpable nodules 2024 articles clinically palpable nodules Scopus articles clinically palpable nodules impact factor journals clinically palpable nodules Scopus journals clinically palpable nodules PubMed journals clinically palpable nodules medical journals clinically palpable nodules free journals clinically palpable nodules best journals clinically palpable nodules top journals clinically palpable nodules free medical journals clinically palpable nodules famous journals clinically palpable nodules Google Scholar indexed journals Thyroid diseases articles Thyroid diseases Research articles Thyroid diseases review articles Thyroid diseases PubMed articles Thyroid diseases PubMed Central articles Thyroid diseases 2023 articles Thyroid diseases 2024 articles Thyroid diseases Scopus articles Thyroid diseases impact factor journals Thyroid diseases Scopus journals Thyroid diseases PubMed journals Thyroid diseases medical journals Thyroid diseases free journals Thyroid diseases best journals Thyroid diseases top journals Thyroid diseases free medical journals Thyroid diseases famous journals Thyroid diseases Google Scholar indexed journals malignant nodules articles malignant nodules Research articles malignant nodules review articles malignant nodules PubMed articles malignant nodules PubMed Central articles malignant nodules 2023 articles malignant nodules 2024 articles malignant nodules Scopus articles malignant nodules impact factor journals malignant nodules Scopus journals malignant nodules PubMed journals malignant nodules medical journals malignant nodules free journals malignant nodules best journals malignant nodules top journals malignant nodules free medical journals malignant nodules famous journals malignant nodules Google Scholar indexed journals ultrasonographic findings articles ultrasonographic findings Research articles ultrasonographic findings review articles ultrasonographic findings PubMed articles ultrasonographic findings PubMed Central articles ultrasonographic findings 2023 articles ultrasonographic findings 2024 articles ultrasonographic findings Scopus articles ultrasonographic findings impact factor journals ultrasonographic findings Scopus journals ultrasonographic findings PubMed journals ultrasonographic findings medical journals ultrasonographic findings free journals ultrasonographic findings best journals ultrasonographic findings top journals ultrasonographic findings free medical journals ultrasonographic findings famous journals ultrasonographic findings Google Scholar indexed journals Multinodular colloid adenomatous hyperplasia articles Multinodular colloid adenomatous hyperplasia Research articles Multinodular colloid adenomatous hyperplasia review articles Multinodular colloid adenomatous hyperplasia PubMed articles Multinodular colloid adenomatous hyperplasia PubMed Central articles Multinodular colloid adenomatous hyperplasia 2023 articles Multinodular colloid adenomatous hyperplasia 2024 articles Multinodular colloid adenomatous hyperplasia Scopus articles Multinodular colloid adenomatous hyperplasia impact factor journals Multinodular colloid adenomatous hyperplasia Scopus journals Multinodular colloid adenomatous hyperplasia PubMed journals Multinodular colloid adenomatous hyperplasia medical journals Multinodular colloid adenomatous hyperplasia free journals Multinodular colloid adenomatous hyperplasia best journals Multinodular colloid adenomatous hyperplasia top journals Multinodular colloid adenomatous hyperplasia free medical journals Multinodular colloid adenomatous hyperplasia famous journals Multinodular colloid adenomatous hyperplasia Google Scholar indexed journals Papillary carcinoma articles Papillary carcinoma Research articles Papillary carcinoma review articles Papillary carcinoma PubMed articles Papillary carcinoma PubMed Central articles Papillary carcinoma 2023 articles Papillary carcinoma 2024 articles Papillary carcinoma Scopus articles Papillary carcinoma impact factor journals Papillary carcinoma Scopus journals Papillary carcinoma PubMed journals Papillary carcinoma medical journals Papillary carcinoma free journals Papillary carcinoma best journals Papillary carcinoma top journals Papillary carcinoma free medical journals Papillary carcinoma famous journals Papillary carcinoma Google Scholar indexed journals
Article Details
Abbreviations for guidelines:
American Thyroid Association (ATA); American Association of Clinical Endocrinologists (AACE); American College of Endocrinology (ACE); Associazione Medici Endocrinologi Medical (AME)
1. Introduction
Thyroid diseases are fairly common. Most of these are clinically palpable nodules. It is reported that 4% of the American population has clinically a palpable thyroid nodule. Autopsy studies showed that 8% of the population had thyroid nodules. It has been reported that 15% of women over 50 years old have a single or multiple nodules in their thyroid [1]. Due to increased availability and sophisticated imaging techniques, increasing numbers of thyroid nodules are determined incidentally. There are palpable thyroid nodules in 1% of men and 5% of women, moreover, there are ultrasonically detectable thyroid nodules in 19% to 67% of unselected patients [2]. In general, 5-15% of these nodules are thyroid cancers although most of the thyroid nodules are benign [3].
Cold thyroid nodules are a major problem because the rate of malignity in solitary cold thyroid nodules is 15-25% and in multiple cold thyroid nodules is 1-6% [4, 5]. Thyroid function tests should be evaluated. Malignancy rate is 1% if thyroid stimulating hormone (TSH) is low. If thyroid nodules are detected, scintigraphy is no indication in the first step. Scintigraphic imaging should be performed if the dominant thyroid nodule in the patient with low TSH (<0.4 mU/L) is ?1 cm. Malignancy rate is 15-20% in cold nodules and <5% in hot nodules [6]. Ultrasonographic evidences associated with thyroid cancer are microcalcification, hypoechogenicity, irregular margin, the absence of halo, intranodular vascularity, round appearance [6]. The detachment of malignant nodules from benign thyroid nodules and early diagnosis of malignant potential nodules are very important in terms of prognosis. If the palpable nodule is detected on the thyroid gland clinically, scintigraphy and ultrasonography (USG) should be performed in addition to thyroid function tests in order to determine the probability of malignancy of the nodule. The main clinical problem in thyroid nodules is to exclude malignancies in these nodules. Most patients with thyroid nodules are asymptomatic, but the absence of symptoms does not exclude malignancy. In the United States, while the annual incidence of thyroid malignancies was 4.9 per 100.000 in 1975, it increased to 14.3 in 2009 [7]. Thyroid cancer rate is 40 cases for one million population every year. Mortality due to thyroid cancer is 6 cases for one million population every year [1]. I aimed to prospectively investigate the common malignancy criteria of nodules with the inclusion of malignancy potential in palpable thyroid nodules by imaging scintigraphically and sonographically.
2. Materials and Methods
The study was conducted on fifty-five patients with palpable thyroid nodules including the suspicions of malignancy admitted to Department of General Surgery in Haydarpa?a Numune Hospital from August 1989 to January 1991. The criterion used in the selection of patients was all patients with the suspicions of thyroid malignancy admitted at this time period. The ages of fifty females and five males patients ranged from 12 to 78 years old with a mean age of 26.8 years. Scintigraphic and ultrasonographic examinations were performed after thyroid function tests such as TSH of these patients were analyzed. The evidences of the scintigraphic and ultrasonographic images were evaluated prospectively. All of these patients underwent surgical intervention and histopathologic results were obtained. The evidences of the scintigraphic and ultrasonographic images were compared with histopathologic results.
Thyroid scintigraphy was performed 30-60 minutes after the administration of Technetium-99m-pertechnetate (Tc-99m) intravenously 1 millicurie (mCi). The results were recorded on a film, photographic paper or plain paper by a gamma camera by using a pinhole collimator while the patient was in the supine position and the neck was hyperextension. Nodules were classified as cold, hot, and normoactive. 4 MHz linear prop, 5 and 6 MHz convex electronic props were used in the ultrasonographic examination. The examination was performed as longitudinal and transverse. The images were detected with a mono printer or multiformat camera. Localizations, sizes, and numbers of nodules were determined. Nodules were defined as solid, complex or cystic. Solid nodules were evaluated as hypoechoic, isoechoic, hyperechoic according to normal thyroid tissue. Whether the nodule boundaries were regular or not was investigated. Whether the nodules had contained the halo or had not was examined. The presence or absence of calcification of nodules and the characteristics of calcification were investigated. Cancer-related ultrasonographic findings such as microcalcification, hypoechogenicity, irregular margins, and absence of halo were separately recorded for each patient.
Histopathologically, the generally accepted classification was used (4):
1. Adenoma 2. Multinodular colloid adenomatous hyperplasia 3. Papillary carcinoma 4. Follicular carcinoma 5. Medullary carcinoma 6. Anaplastic carcinoma
3. Statistical Analysis
The Kolmogorov-Smirnov test was used for normal distributions. Mann-Whitney U and chi-square tests were performed to compare the results. Sensitivity and specificity were calculated. Differences were considered statistically significant at a value of p?0.05. The statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) for Windows Version 15.0.
4. Results
Histopathologically, malignancy was detected in five of fifty-five patients after surgery. For this reason, the patients were divided into two groups as benign and malignant. A statistically significant difference between benign and malignant groups was not found according to gender and age (Table 1). All the patients in the malignant group were female. After the patients had been evaluated according to their histopathological results, papillary carcinoma was found in four patients and papillary-follicular carcinoma was in one patient. Follicular adenoma was detected in seven patients. Other patients were reported as multinodular colloidal adenomatous hyperplasia.
In scintigraphic examinations, a total of ninety-three nodules were found in fifty-five patients. Twenty-six patients had solitary nodules and twenty -nine patients had multiple nodules. Of the ninety-three nodules sixty-one were cold, twelve were warm, and twenty were normoactive. Forty-six patients had the cold nodule. The rate of malignancy in patients with cold nodule was 10.8%. A scintigraphic image of the cold nodule of a patient with a benign histopathologic result is shown in Figure 1. A statistically significant difference between benign and malignant groups was not found according to the presence of malignancy in patients with cold nodule (Table 1). There was no hot nodule in the malignant group. The cold nodules were determined in eighteen patients after the radioactive characteristics of the nodules were evaluated in twenty-six patients who had a solitary nodule in scintigraphic images. Three of these patients were malignant and the rate was 16.6%. The cold nodules were determined in twenty-eight patients after the radioactive characteristics of the nodules were evaluated in twenty-nine patients who had multiple nodules in scintigraphic images. Two of these patients were malignant and the rate was 7%. Accordingly, the sensitivity and specificity of cold nodules to malignancy were found as 100% and 82%, respectively (Table 1).
|
|
Benign |
Malign |
p |
||
|
Sex |
Male |
5 |
0 |
0.458 |
|
|
Female |
45 |
5 |
|||
|
Age (years) |
27.3 ± 9.96* |
21.4 ± 2.96* |
0.076 |
||
|
Diameter of dominant nodules at USG (mm) |
42.4 ± 8.39* |
53.8 ± 6.87* |
0.007 |
||
|
Cold nodules** |
Yes |
41 |
5 |
0.3 |
|
|
No |
9 |
0 |
|||
* Mean ± Standard derivation; ** sensitivity: 100% specificity: 82%
Table 1: Evaluation of the groups in terms of age, sex, diameters of nodules and cold nodules.
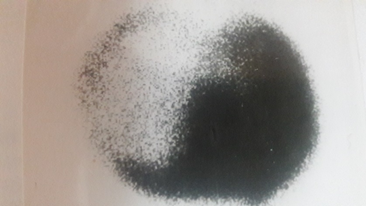
Figure 1: Scintigraphy: Cold nodule in thyroid right lobe (Result of histopathology: Benign).
In sonographic examinations, a total of one hundred and sixteen nodules were found in fifty-five patients. The smallest of these nodules was 4.3 mm and the largest was 65 mm. The mean nodule diameter was 33 mm. A comparison was performed between two groups of patients according to the dominant nodule diameter of each patient, and the diameter was significantly larger in the malignant group (p=0.007) (Table 1). The malignancy was found in three of the sixteen patients with solitary nodule and in two of the thirty-nine patients with multiple nodules. More than one nodule was determined in ten patients after sonographic examination had been performed in twenty-six patients who had a solitary nodule in scintigraphic images and the rate was 38.4%.
One hundred and sixteen nodules were evaluated according to their sonographic characteristics and it was seen that there were eighty-eight solid, twenty-five complex, and three cystic characters. The malignancy was identified in three of the solid nodules and was in two of the complex nodules. The malignancy was not found in cystic nodules. The sensitivity to determine malignancy was 100% while the solid and complex structure of the nodule was evaluated together, but it was 60% and 40% respectively while assessed separately. The specificity to determine malignancy of the solid and complex structure of the nodule was 8% while the solid and complex structure of the nodule was evaluated together. The specificity to determine malignancy was 26% for solid nodule and was 82% for the complex nodule.
Eighty-eight solid nodules were evaluated according to their sonographic echogenicity and it was seen that there were fifty-six hypoechogenic, twenty isoechogenic, and twelve hyperechogenic. Three cases of malignancy were hypoechogenic too. The microcalcifications were found in six patients. One of these patients was malignant. The contours of the nodules were assessed sonographically and irregular margins were found in ten patients who had seventeen nodules. All of five malignancy patients were also found to have an irregular margin. The forty-one nodules with no halo were found in twenty-two patients. Four of the five malignant patients had no halo.
The patients with only one malignancy findings at USG were compared according to groups and a significant difference was not found (Table 2). However, the patients with two or three malignancy findings at USG were compared according to groups and significant differences were found (p=0.001) (Table 2). The sensitivity and specificity for the patients with two malignancy findings at USG were found as 100% and 72%, respectively. Moreover, the sensitivity and specificity for the patients with three malignancy findings at USG were found as 60% and 96%, respectively (Table 2). The sensitivity and specificity of USG findings suggesting malignancy in thyroid nodules were separately calculated (Table 3).
|
Malignancy findings at USG |
Benign (n) |
Malign (n) |
p |
|
|
One finding |
Yes |
37 |
5 |
0.192 |
|
|
No |
13 |
0 |
|
|
Two findings |
Yes |
14 |
5 |
0.001* |
|
|
No |
36 |
0 |
|
|
Three findings |
Yes |
2 |
3 |
0.001** |
|
|
No |
48 |
2 |
|
* sensitivity: 100% specificity: 72%; ** sensitivity: 60 % specificity: 96%
Table 2: Malignancy findings at USG according to groups.
|
USG findings |
Sensitivity (%) |
Specificity (%) |
|
Hypoechogenicity |
60 |
50 |
|
Microcalcification |
20 |
90 |
|
Irregular margins |
100 |
90 |
|
Absence of halo |
80 |
66 |
Table 3: suggesting malignancy in thyroid nodules.
5. Discussion
Thyroid nodules were generally evaluated as primer via scintigraphy in previous periods. Solitary cold nodules, in other words, solitary hypoactive nodules were considered to have the malignant probability of 15-25%. The malignancy probability of cold nodule cases detected in a multinodular gland was between 1% and 6% [4, 5]. In this study, the likelihood of malignancy in solitary cold nodules was found as16.6% and was consistent with the literature. In addition, the malignancy probability of cold nodule cases detected in a multinodular gland was found as 7% and was a little higher than in the literature. In the investigations carried out, approximately 10-25% of the nodules detected as scintigraphic cold nodule was found as carcinoma [8]. In this study, the malignancy probability of the nodules detected as scintigraphic cold nodule was found as 10.8% and was consistent with the literature as well. Rojeski reported this rate as 16% [9]. Although the sensitivity and specificity of cold nodules to malignancy were found as 100% and 82%, respectively, a statistically significant difference between benign and malignant groups was not found according to the presence of malignancy in patients with the cold nodule. The reason for this may be due to the low number of patients. Nowadays, scintigraphy is recommended to be performed in patients with TSH suppression [4, 10].
Nowadays, the basis of thyroid nodule management is high resolution ultrasound (US), sensitive TSH, fine needle aspiration biopsy (FNAB) and clinical findings. Clinical and US risk factors for malignant diseases should always be observed. All patients with palpable thyroid nodules or clinical risk factors should undergo US evaluation. In ATA guidelines, it has been stated that thyroid USG evaluating of cervical lymph nodes should be performed in all patients with known or suspected thyroid nodules (strong recommendation, high level evidence). The USG can assess the size, characterization, presence of a nodular structure in the thyroid gland and whether there is a cervical lymphadenopathy associated with the nodule. Thyroid USG is widely used to evaluate the risk of malignancy in thyroid nodules and to decide whether or not the FNAB is indicated. It helps to distinguish non-palpable nodules up to a size of 0.3 mm. The malignancy rate was found as 27% in those with solitary nodule and multinodular goiter and those with the dominant nodule diameter was 40 mm or more [11]. In this study, the size of the nodule diameter was found to be significant in terms of malignancy (Table 1). The cancer risk is similar in those with solitary thyroid nodules and those with multinodular goitre (Evidence Level 3, according to the AACE / ACE / AME guidelines evidence levels) [12-16]. The cancer risk was not similar in those with solitary thyroid nodules and those with multinodular goitre in this study due to the low number of patients. It has been suggested that about 70% of solitary cases in scintigraphy and physical examination were sonographically multiple [17]. In this study, this rate was found as 38.4% due to the low number of patients.
The majority of thyroid cancers, 82-91% are solid tumors [18-22]. In a study carried out in Mayo clinic, 88% solid or minimal cystic were determined in 360 consecutive cases operated due to malignancy, 9% were less than 50% cystic and only 3% were more than 50% cystic [23]. In this study, the malignancy was identified in three of the solid nodules and was in two of the complex nodules. The sensitivity to determine malignancy was calculated as100% for the solid and complex structure together. However, it was calculated as 60% and 40% respectively for separate assessment. Therefore, the decision of FNAB for partially cystic thyroid nodules should be performed by taking into account the different US findings. These findings include the eccentric placement of the solid component, sudden angulations in the components, and microcalcifications.
Most of the thyroid nodules are hypoechoic, similarly, most of the thyroid cancers are hypoechoic according to normal thyroid tissue. The risk of malignancy in isoechoic nodules is moderate and is low in hyperechoic nodules [4]. In this study, the malignancy was detected in three of eighty-eight solid nodules and three patients had hypoechoic nodules too. Rago and colleagues suggested the sensitivity and specificity for malignancy of hypoechoic nodule as 66.6% and 45.6%, respectively. Moreover, Papini and colleagues suggested these values as 87.1% and 43.4%, respectively [12, 24]. In this study, the values of 60% sensitivity and 50% specificity were close to the study of Rago and colleagues (Table 3).
Microcalcifications are seen as hyperechogenic points of the nodule in the USG. It is usually multiple and the dimensions are smaller than 2 mm [25]. Calcification is present in 10-15% of all thyroid nodules. Location and pattern are important to distinguish malignant-benign nodules [4]. Peripheral calcification in the form of the eggshell is found in benign nodules. In the same way, large and coarse calcifications are the sign of benignity. Fine and punctate calcifications suggest the risk of malignancy. Thin calcifications can be the psammoma bodies and these bodies are seen in papillary carcinoma. Microcalcifications may also occur in medullary carcinoma. In the literature, it is stated that the most reliable sonographic finding in the benign-malign nodule differentiation is microcalcification [17]. In spite of low sensitivity (36%), the highest specificity (93%) was found among the sonographic criteria [26]. The appearance of microcalcification in the form of a snowstorm has 100% specificity. FNAB should be performed for nodules containing microcalcification having this appearance [27]. Similarly, in this study, sensitivity and specificity were found as 20% and 90%, respectively (Table 3).
Irregular margin, excessive microlobulation on the borders of the nodules are accepted to be malignancy finding [28]. Benign nodules tend to be well-defined, sharp contours, while malign nodules tend to be irregular limited, weak contoured. In this study, the sensitivity and specificity of detection of malignancy in nodules with irregular margins were calculated as 100% and 90%, respectively. Papini and colleagues found these values as 77.5% and 80%, while Kim and colleagues found 55.1% and 83% respectively [12, 28].
Halo is sonographically hypoechoic, a sonolucent ring seen around the nodule. It is usually considered to be a benign finding. In the benign nodules, It is regular, thinner than 2 mm, surrounding the nodule continuously [29]. The halo capsule, which separates the nodule from the thyroid tissue, may be due to compression tissue, inflammation, and edema. Increased vascularity can be demonstrated in this region with doppler technique [30]. An ultrasonographic image of the halo of a patient with a benign histopathologic result is shown in Figure 2. In the study performed by Rago and colleagues, the sensitivity of demonstration the malignancy of the absence of halo was found to be 66.6% and specificity 77% [31]. In this study, the sensitivity of detecting malignancy of halo absence was 80% and specificity was 66% (Table 3).

Figure 2: Ultrasonography: The nodule with 65 mm in diameter, showing hyperechogenicity, halo and cystic degeneration in the thyroid right lobe (Ultrasonography pertains to the patient in Figure 1).
In the USG study, although the sensitivity is low for a single feature, the features with the highest specificity (median> 90%) for thyroid cancer are microcalcifications, irregular margins, and tall shape. Several studies performed have reported that various of USG features is associated with thyroid cancer and the majority are papillary thyroid cancer. These features include microcalcifications, nodule hypoechogenicity, irregular margins, and tall nodule (Evidence Level 2, according to the AACE / ACE / AME guidelines evidence levels) [12, 14, 18-21, 32-34]. It is not appropriate to estimate the malignancy with only USG characteristics because these features described in USG have a low predictive sensitivity to cancer. The combination of two or more of these features may suggest an increased risk of thyroid cancer. In this study, there was no significant difference when patients with only one malignancy finding at USG compared according to groups (Table 2). Moreover, these features such as hypoechogenicity, microcalcification, and absence of halo described in USG had a low predictive sensitivity to cancer (Table 3). However, significant differences between the groups were indicated after the patients with two or three malignancy findings at USG had been compared (Table 2). In addition, the sensitivity for the patients with two malignancy findings at USG was found as 100% (Table 2). These results are the most striking findings of the study. The limitation of this study is a low number of patients. Comparing prospectively assessed imaging findings with definitive pathology results is the strong side of the study.
6. Conclusion
Considering the scintigraphic features, the hypoactive appearance of the nodule at scintigraphy is a reliable finding with a low grade in the detection of malignancy, furthermore, the risk of malignancy is not high when this finding is detected. The solid, cystic or complex sonographic structure of the nodule is not a reliable finding in the screening of malignancy. Similarly, the solitary sonographic structure of the nodule is also not a reliable finding in the screening of malignancy. In the presence of these findings, the risk of malignancy is not high. Considering the ultrasonographic features, the most sensitive features of malignant differentiation are nodule with irregular margin, nodule without halo its around, and a hypoechoic appearance of the nodule. The highest specificity is nodule with microcalcification and irregular margin. According to these findings, microcalcification is not a reliable finding in the screening of malignancy, but the risk of malignancy is high when microcalcification is detected. The hypoechoic appearance of the nodule and the absence of halo around the nodule are reliable in the detection of malignancy, but the risk of malignancy is low because of low specificity when these features are detected. However, since irregular margin sonographic sensitivity and specificity are high, it is safe for malignancy screening and the risk of malignancy is high when this finding is detected. Furthermore, because the sensitivity for the patients with two malignancy findings at USG is high, it is safe for malignancy screening when two findings are detected for the same patient. In summary, the combination of two or more of these USG findings may suggest an increased risk of thyroid cancer and FNAB is still the most important diagnostic method in the diagnosis of thyroid malignancies.
Acknowledgment
I have not any sources of funding for my research.
Conflicts of Interest
I have not any financial and personal relationships with other people or organizations.
References
- Sadler GP, Clark OH. Schwartz’s Principles of Surgery. 4th edition (1984): 1545-1566.
- Smith PW, Salomone LJ, Hanks JB. Sabiston textbook of surgery: The biological basis of modern surgical practice. 19th edition (2012): 899.
- Cooper DS, Doherty GM, Haugen BR, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19(2019): 1167-1214.
- Solbiati L, Volterrani L, Rizzatto G, et al. The thyroid gland with low uptake lesions: evaluation by ultrasound. Radiology 155 (1985): 187-191.
- McGahan JP. Controversies in Ultrasound: Clinics in Diagnostic Ultrasound Series 20 (1987): 179-220.
- Smith PW, Hanks LB, Salomone LJ, et al. Sabiston textbook of surgery(): The biological basis of modern surgical practice. 20th edition (2017): 889-900.
- Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg 140 (2014): 317-322.
- Chen H, Zeiger NA, Clark DP, et al. Papillary carcinoma of thyroid: Can operative management be based safely on fine needle aspiration?. J Am Coll Surg 184 (1997): 605.
- Rojeski TM, Gharrib H. Nodular thyroid disease: Medical progress. N Eng J Med 313 (1984): 428-434.
- Cooper DS, Doherty GM, Haugen BR, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16 (2006): 109-142.
- Ravetto C, Colombo L, Dottorini ME. Usefulness of fine-needle aspiration in the diagnosis of thyroid carcinoma: A retrospective study in 37,895 patients. Cancer 90 (2000): 325-329.
- Papini E, Guglielmi R, Bianchini A, et al. Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab 87 (2002): 1941-1946.
- Horvath E, Majlis S, Rossi R, et al. An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management. J Clin Endocrinol Metab 94 (2009): 1748-1751.
- Moon WJ, Jung SL, Lee JH, et al. Benign and malignant thyroid nodules: US differentiation multicenter retrospective study. Radiology 247 (2008): 762-770.
- Kim EK, Park CS, Chung WY, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol 178 (2002): 687-691.
- Corrias A, Einaudi S, Chiorboli E, et al. Accuracy of fine needle aspiration biopsy of thyroid nodules in detecting malignancy in childhood: comparison with conventional clinical, laboratory, and imaging approaches. J Clin Endocrinol Metab 86 (2001): 4644-4648.
- Rumack CM, Wilson SR, Charboneau JW. Diagnostic Ultrasound. Cv Mosby (1998): 715-716.
- Kwak JY, Han KH, Yoon JH, et al. Thyroid imaging reporting and data system for US features of nodules(): a step in establishing better stratification of cancer risk. Radiology 260 (2011): 892-899.
- Salmaslioglu A, Erbil Y, Dural C, et al. Predictive value of sonographic features in the preoperative evaluation of malignant thyroid nodules in a multinodular goiter. World J Surg 32 (2008): 1948-1954.
- Gul K, Ersoy R, Dirikoc A, et al. Ultrasonographic evaluation of thyroid nodules: comparison of ultrasonographic, cytological, and histopathological findings. Endocrine 36 (2009): 464-472.
- Frates MC, Benson CB, Doubilet PM, et al. Prevalence and distribution of carcinoma in patients with solitary and multiple thyroid nodules on sonography. J Clin Endocrinol Metab 91 (2006): 3411-3417.
- Nam-Goong IS, Kim HY, Gong G, et al. Ultrasonography-guided fine needle aspiration of thyroid incidentaloma: correlation with pathological findings. Clin Endocrinol 60 (2004): 21-28.
- Henrichsen TL, Reading CC, Charboneau JW, et al. Cystic change in thyroid carcinoma: prevalence and estimated volume in 360 carcinomas. J Clin Ultrasound 38 (2010): 361-366.
- Rago T, Vitti P, Chiovato L, et al. Role of conventional ultrasonography and color flow-doppler sonography in predicting malignancy in 'cold' thyroid nodules. Eur J Endocrinol 138 (1998): 41-46.
- Varverakis E, Neonakis E. Contribution of high-resolution ultrasonography in the differential diagnosis of benign from malignant thyroid nodules. Hormones 1 (2002): 51-56.
- Takashima S, Fukuda H, Nomura N, et al. Thyroid nodules: re-evaluation with ultrasound. J Clin Ultrasound 23 (1995): 179-184.
- Iannuccilli JD, Cronan JJ, Monchik JM. Risk for malignancy of thyroid nodules as assessed by sonographic criteria: the need for biopsy. J Ultrasound Med 23 (2004): 1455-1464.
- Kim EK, Park CS, Chung WY, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol 178 (2002): 687-691.
- Solbiati L, Cioffi V, Ballarati E. Ultrasonography of the neck. Radiol Clin North Am 30 (1992): 941-954.
- Propper RA, Skolnick ML, Weinstein BJ, et al. The nonspesifity of halo sign. J Clin Ultrasound 8 (1980): 129-132.
- Rago T, Vitti P, Chiovato L, et al. Role of conventional ultrasonography and color flow-doppler sonography in predicting malignancy in 'cold' thyroid nodules. Eur J Endocrinol 138 (1998): 41-46.
- Moon HJ, Kwak JY, Kim MJ, et al. Can vascularity at power Doppler US help predict thyroid malignancy? Radiology 255 (2010): 260-269.
- Cappelli C, Pirola I, Cumetti D, et al. Is the anteroposterior and transverse diameter ratio of nonpalpable thyroid nodules a sonographic criteria for recommending fine-needle aspiration cytology? Clin Endocrinol 63 (2005): 689-693.
- Campanella P, Ianni F, Rota CA, et al. Quantification of cancer risk of each clinical and ultrasonographic suspicious feature of thyroid nodules: a systematic review and meta-analysis. Eur J Endocrinol 170 (2014): 203-211.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 