T-shaped Uterus, Other Studies are Needed But What Can We Do in The Meantime?
Loris Marin1*, Guido Ambrosini1, Simone Antonio Laganà2, Giampiero Capobianco3, Francesco Dessole3, Alessandra Andrisani1
1Department of Women's and Children's Health, University of Padua, Salus Pueri, Padua, Italy.
2Unit of Gynecology Oncology, Department of Health Promotion, Mother and Child Care, Internal Medicine and Medical Specialities (PROMISE), University of Palermo, 90127 Palermo, Italy.
3Department of Surgical, Microsurgical and Medical Sciences, Gynecologic and Obstetric Clinic, University of Sassari, Sassari, Italy.
*Corresponding Author: Loris Marin, Department of Women’s and Children’s Health, University of Padua, Salus Pueri, Padua, Italy
Received: 19 August 2022; Accepted: 26 August 2022; Published: 19 September 2022
Article Information
Citation: Loris Marin, Guido Ambrosini, Simone Antonio Laganà, Giampiero Capobianco, Francesco Dessole, Alessandra Andrisani. T-shaped Uterus, Other Studies are Needed But What Can we Do in The Meantime?. 5 (2022): 526-528.
View / Download Pdf Share at FacebookKeywords
<p>T-shaped Uterus, Malformation</p>
Article Details
Dysmorphic uterus is a condition that can affect fertility differently depending on the type of malformation [1-3]. The underlying etiopathogenetic processes can be vary and they can involve fusion or resorption defects [4,5]. The most common uterine malformation is the septum [1] but other uterine malformations can affect fertility, as t-shaped uterus [4]. This uterine malformation is characterized by a narrowed uterine cavity with lateral indentations and the shape of the endometrial cavity resembles the letter T due to thickened lateral walls. During hysteroscopy the uterine cavity appears tubular and tubal ostia are not visible from the isthmus [4]. T-shaped uterus was first described in 1977 and, until the 1980s, it has been associated to diethylstilbestrol (DES) exposure during intrauterine life. DES is a non-steroidal synthetic estrogen that was widely prescribed between 1940 and 1970 to prevent abortion. However, in utero exposure to DES alone cannot justify the prevalence of this kind of malformation that reaches 13% in infertile women. Exact etiopathogenetic mechanisms are not known but endocrine disruptors, that may mimic or interfere with body's hormones, can have a role and they may act as DES during Mullerian organogenesis [4]. There is no agreement on the diagnosis [2,6,7] and management [5,8] of the t-shaped uterus and also on the effect of this malformation on fertility and obstetric outcomes [3,9,10]. T-shaped uterus can be suspected through different types of examinations as 2D vaginal ultrasound, hysteroscopy, hysterosalpingography, magnetic resonance imaging and the 3D-vaginal ultrasound [4]. This latter allows the visualisation of the coronal view of the uterus, it is a non-invasive examination, it does not require the use of contrast agents and it does not cause discomfort for the patient [6]. Different society tried to classify this kind of malformation, ESHRE/ESGE classification places T-shaped uterus in the category of “dysmorphic uterus” (normal uterine outline but with an abnormal shape of the uterine cavity excluding septa) with the “uterus infantilis” and “others” that include all minor deformities of the uterine cavity [6]. The CUME classification permits a more objective assessment of the T-shape uterus through three criteria that define this uterine malformation. At least two of the following criteria must be present to diagnose a t-shaped uterus: lateral indentation angle ≤ 130°, lateral indentation depth ≥ 7 mm and T-angle ≤ 40° [6]. Studies demonstrate a correlation between T-shaped uterus and unexplained infertility, repeated implantation failures or miscarriages, extrauterine pregnancies and preterm birth, despite only low-quality studies are available [2,5]. Finally, management is also controversial due to the use of non-standardized diagnostic criteria [6,11] and subjectivity in treatment [4,8]. Some authors suggest an expectant management, others recommend surgery as first step, others only for women undergoing assisted reproductive technology (ART) [2,5,9]. The common conclusion of many studies is the need for RCT studies to evaluate the real benefit of surgical treatment for T-shaped uterus [4,5]. But what can we do in the meantime? To answer this question, it is crucial to consider the utility of the diagnosis of T-shaped uterus and the potential risks and potential benefits of its correction. An accurate uterine evaluation is a useful procedure before trying to get pregnant and it is fundamental in an ART process. The diagnosis of a uterine malformation is essential to counsel the patient and to reduce negative obstetric outcomes [5]. Concerns emerged about the risk of overestimating the diagnosis of t-shaped uterus with 3D ultrasound, also in relation to the time of the cycle in which the ultrasound examination was performed or the use of estrogen-progestins [11]. Considering that uterine cavity volume significantly increases during the proliferative phase and remains relatively stable throughout the secretory phase, the best time to perform the 3D ultrasound assessment might be this letter one, when there is a smaller risk of overestimating [11]. Finally, should we correct T-shaped uterus?
Surgical risks are very low after an accurate preoperative evaluation. Several techniques have been proposed, those that do not require cervical dilatation seem to be the best choice to avoid the risk of cervical injuries [4,8]. In our clinical practice we use Bettocchi hysteroscope, a 4.2 mm hysteroscope with operative channel for bipolar electrode (Versapoint Twizzle), and we perform longitudinal incisions from the fundus to the isthmus until tubal ostia are visible from the isthmus. The use of an electrolytic solution as distension medium avoids the risks of severe electrolyte imbalance syndromes. In the literature is it reported a case report of metroplasty for T-shaped uterus with the resection of lateral fibromuscular tissue using a bipolar 15 Fr miniresectoscope [8]. This technique could be particularly interesting in the research field because a histological examination of removed tissue could be obtained and it would be possible to study the composition of the tissue (the proportion of muscle and fibrotic tissue).
The main advantage of metroplasty for T-shaped uterus is the restoration of a normal size cavity. Women with a reduced uterine cavity volume have a higher the risk of early and late miscarriage and preterm labor [2]. Considering the low risks of complications of surgical correction of T-shaped uterus [4,5], women undergoing ART procedures should undergo metroplasty first. Whenever women refuse to undergo surgery, they should be advised that there is an increased risk of multiple pregnancies with ART and they should receive single embryo transfer considering the cavity size.
Moreover, the volunteer endometrial injury performed during the metroplasty can cause an inflammatory response within the endometrium and the following wound healing response could improve the environment of the endometrium according to the endometrial scratching theory [12]. It could be interesting to investigate whether the remodeling of uterine walls can have a protective role on obstetric complication related to myometrial invasion of the trophoblast as preeclampsia.
In conclusion, while waiting for RCT studies on the diagnosis and treatment of this low-prevalent uterine malformation, we believe that its management should be patient-center, in relation to the age of the patient, infertility duration, the ovarian reserve and history of repeated miscarriages or implantation failures. We propose a flow chart as in figure 1.
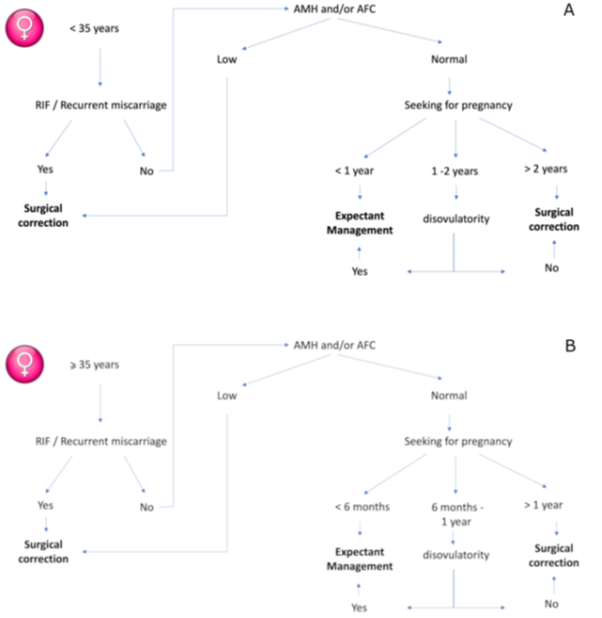
Figure 1: Suggested flowchart for T-shaped uterus management. A. women < 35 years old. B. women ³ 35 years old.
References
- Noventa M, Spagnol G, Marchetti M, et al. Uterine Septum with or without Hysteroscopic Metroplasty: Impact on Fertility and Obstetrical Outcomes-A Systematic Review and Meta-Analysis of Observational Research. Journal of Clinical Medicine 11 (2022): 3290.
- Coelho NMA, Ludwin A, Petraglia F, et al. Definition, prevalence, clinical relevance and treatment of T-shaped uterus: systematic review. Ultrasound in Obstetrics & Gynecology 57 (2021): 366-77.
- Sánchez-Santiuste M, Ríos M, Calles L, et al. Dysmorphic Uteri: Obstetric Results after Hysteroscopic Office Metroplasty in Infertile and Recurrent Pregnancy Loss Patients. A Prospective Observational Study. Journal of Clinical Medicine 9 (2020): 28-57.
- La Marca A, Imbrogno MG, Gaia G, et al. T-shaped uterus: what has been done, what should be done. Minerva Obstetrics and Gynecology 73 (2021): 500-505.
- Garzon S, Laganà AS, Di Spiezio Sardo A, et al. Hysteroscopic Metroplasty for T-Shaped Uterus: A Systematic Review and Meta-analysis of Reproductive Outcomes. Obstetrical & Gynecological Survey 75 (2020): 431-444.
- Seyhan A, Ertas S, Urman B. Prevalence of T-shaped uterus among fertile women based on ESHRE/ESGE and Congenital Uterine Malformation by Experts (CUME) criteria. Reproductive BioMedicine Online 43 (2021): 515-522.
- Alonso PL, Bermejo LC, Carugno J, et al. The rule of 10: a simple 3D ultrasonographic method for the diagnosis of T-shaped uterus. Archives of Gynecology and Obstetrics 304 (2021): 1213-1220.
- Catena U, Campo R, Bolomini G, et al. New approach for T-shaped uterus: Metroplasty with resection of lateral fibromuscular tissue using a 15 Fr miniresectoscope. A step-by-step technique. Facts, Views and Vision in Obstetrics and Gynaecology 13 (2021): 67-71.
- Zhang Y, Zhu Y, Ge B, et al. Reproductive outcome of hysteroscopic metroplasty for women with T-shaped uterus: a retrospective study. Reproductive Health 19 (2022): 78-99.
- Neal SA, Morin SJ, Werner MD, et al. Three-dimensional ultrasound diagnosis of T-shaped uterus is associated with adverse pregnancy outcomes after embryo transfer. Reproductive BioMedicine Online 39 (2019): 777-783.
- Leone FPG, Cammarata S. Oral contraception and overdiagnosis of T-shaped uterus: keep calm and rescan. Ultrasound in Obstetrics & Gynecology 57 (2021): 655-656.
- Vitagliano A, Vitale SG, Cianci A, et al. Endometrial scratching for infertility: The never-ending story. Journal of Gynecology Obstetrics and Human Reproduction 49 (2020): 101743.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 