Using the lateral thoracic pedicle with nipple-areola complex for Gestational Gigantomastia reduction: A case report
Tran Thiet Son1,2,3, Ta Thi Hong Thuý1,3*, Phan Tuan Nghia1,3, Pham Thi Viet Dung1,3
1Department of Plastic and Reconstructive Surgery, Hanoi Medical University, Hanoi, Vietnam
2Department of Plastic Reconstructive and Aesthetic Surgery, University of Medicine and Pharmacy, Hanoi National University, Vietnam
3Department of Plastic Reconstructive and Aesthetic Surgery, Bach Mai Hospital, Hanoi, Vietnam
*Corresponding Author: Ta Thi Hong Thuý, Department of Plastic and Reconstructive Surgery, Hanoi Medical University, Hanoi, Vietnam
Received: 25 October 2023; Accepted: 06 November 2023; Published: 30 November 2023
Article Information
Citation: Tran Thiet SÆ¡n, Tạ Thi Hong Thuý, Phan Tuan Nghia, Pham Thi Viet Dung. Using the lateral thoracic pedicle with nipple-areola complex for gestational gigantomastia reduction: A case report. Journal of Surgery and Research. 6 (2023): 387-390.
View / Download Pdf Share at FacebookAbstract
Gigantomastia, or breast hypertrophy, is a condition that involves developing extremely large breasts due to excessive growth of breast tissue. Breast reduction surgery is an option that can help patients regain normal breasts. Several surgeons have presented a variety of techniques, but the axial flap bearing the nipple aerolar complex (NAC) remains controversial. We present a particular case of severe gigantomastia with a distance from the sternal notch to the NAC of approximately 48 cm. The surgical method of breast reduction uses a dermoglandular axial pedicle of the lateral thoracic vessels bearing the NAC. As a result, the patient was satisfied, the breast contour was similar to normal breasts, and there were no complications of the NAC. With this case, we wish to restate the safety and reliability of the pedicle bearing the NAC in breast reduction surgery, even when the pedicle of choice is the lateral thoracic vessels.
Keywords
<p>Gestational Gigantomastia, Nipple-areola complex (NAC), Surgery</p>
Article Details
Introduction
Gigantomastia is a rare condition characterized by diffuse and excessive breast growth and associated with juvenile, pregnancy-induced, drug-induced, idiopathic, tumors, obese, and autoimmune disease [1,2]. Gestational gigantomastia (GG) is a type of gigantomastia that appears during the first or second trimester of pregnancy [2-4]. Breast growth that is too rapid can cause abnormal discomfort, stretched overlying skin necrosis, severe mastitis and hemorrhage, and negatively impact long term milk production [5]. Reduction mammoplasty may be an appropriate choice for severe gestational gigantomastia and can use a variety of techniques, such as mastectomy combined with the “free nipple graft” technique or pedicled technique [6,7]. Most surgeons prefer “free nipple grafting” as a choice for gigantomastia, due to the simplicity of the technique, but the disadvantages of this technique are nipple hypopigmentation, graft failure, and decreased breast projection. The pedicled technique is suitable for cases with mild to moderately large breasts. However, the pedicled technique remains controversial in patients with severe gigantomastia, resulting in necrosis to the nipple-areola complex [8]. The latero-thoracic artery (LTA) flap is little-known in gigantomastia reduction. In this article, we present the use of the latero-thoracic pedicle flap bearing the nipple-areola complex (NAC) - for breast reduction in patients with gestational gigantomastia.
Case Presentation
A 30-year-old woman with a history of breast enlargement during her pregnancy, presented with complaints of chest and back pain. There was no other personal or family history for breast disease. Her original breast size was a B cup. During the 24 weeks gestation, bilateral breast growth progressed rapidly and was accompanied by chest and back pain. During pregnancy, management with dicloxacillin and bromocriptine was ineffective. At 39 weeks gestation, she was schedule for a cesarean section and gave birth to a female newborn. She reported swelling, erythema, pain, and continued to have more rapid progressive enlargement in the volume of both breasts during the postpartum period. She went to the plastic surgery department for surgical treatment in 2007, six months after pregnantcy. On examination, she weighed 70 kg, was 165 cm in height, and had a body mass index (BMI) of 25.7 kg/m2. Both of breasts showed significant enlargement and grade III breast ptosis, asymmetry, the left breast being slightly larger than the right. The skin covering the breasts showed marked hyperpigmentation and dilated veins. The NAC enlarged to approximately 14 cm, without bleeding or discharge. The sternal notch to nipple measurements were 47 cm on the right and 49 cm on the left. The nipple to inframammary fold (IMF) measured 34 cm on the right and 33 cm on the left. Breast ultrasonography showed no obvious fluid collections or seroma. Pathological biopsy findings showed chronic dermal inflammation without evidence of malignancy. All laboratory investigations were within normal limits. Gestational gigantomastia was diagnosed, and surgical intervention was proposed, including bilateral mastectomy and reduction mastoplasty with a lateral-thoracic pedicle flap bearing the NAC. Using Doppler helped determine the arteries supplying blood to breasts. Blood vessels that are continous with the areola were marked on the skin surface. Measurements of arterial diameter and vessel depth were performed using color ultrasound. The laterothoracic vessels were chosen as the axis pedicle containing the NAC, because the diameter of the LTAs was larger than the IMA and were the major vessels entering the areola. A Wise pattern skin excision was marked in in supine position.
The new areolar position was determined to be at 17cm from the clavicle to the nipple. The pedicles containing the nipple-areola complex were marked, including a 7x30cm right superior pedicle and a 8x32cm left superolateral pedicle. The skin incisions were made according to plan. The dermoglandular pedicle flap was de-epithelialized. Excess tissue was resected. After rigorous hemostasis and placement of suction drains, closure was continued layer by layer until the skin ended with an inverted “T” closure with non-absorbable sutures. The weights of breast tissue excised from the right and left breasts were 3600 g and 4000 g, respectively. The postoperative course was favorable, with no complications. Follow-up of the patient 4 years after surgery showed no recurrence.
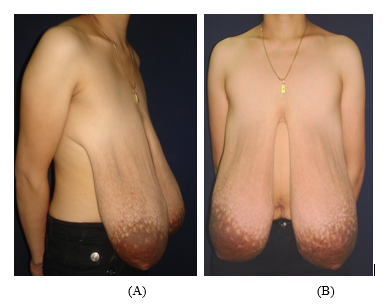
Figure 1: The pre-operation condition of the patient. (A): the right lateral view; (B): The front view
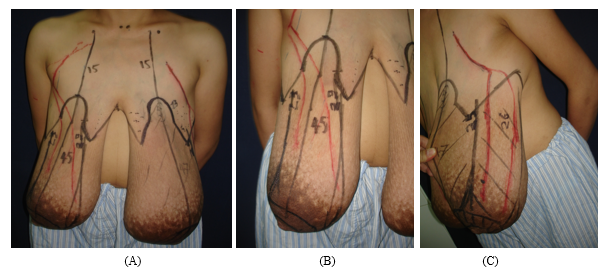
Figure 2: The design marked pre-operation. (A): The front view; (B): The design of superior pedicle bearing NAC in right breast; (C): The design of superio-lateral pedicle bearing NAC in left breast
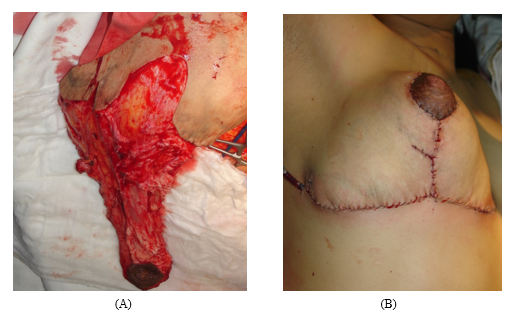
Figure 3: The intra- and post-operative images. (A): The dermoglandular pedicle bearing the NAC; (B): The result after the surgery. The NAC was well vascularized.
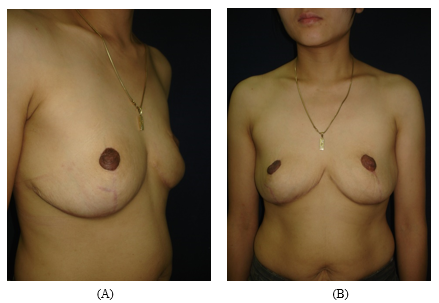
Figure 4: The result after four years of follow-up. (A): The lateral view; (B): the front view.
Discussion
Gigantomastia is a rare condition characterized by diffuse and excessive breast growth associated with adolescence, pregnancy, drug-induced, idiopathic, tumors, obesity, and autoimmune diseases. Breast enlargement is considered gigantomastia, in which excessive tissue exceeds 2-2.5kg [2]. Gestational gigantomastia (GG) is a type of gigantomastia that occurs at the onset of pregnancy or between the 16th and 20th week of gestation. It is estimated to affect roughly 1 in 100,000 pregnancies. This disease can also cause difficulty with movement and breathing as well as emotional, social, and psychological problems [7]. Medical management and surgery are two options, and reduction mammoplasty is considered the gold standard for GG [3]. In breast reduction, depending on the severity of excess tissue, various techniques may be preferred to reduce massive breast size with preservation of NAC and breastfeeding. Procedures with dermoglandular pedicle techniques described for reduction mammoplasty have now been successfully applied for medium and large hypertrophic breasts [8]. However, these techniques cannot preserve the NAC in gigantomastia patients. Breast reduction surgery in patients with gigantomastia proves to be a challenge for plastic surgeons. The high complication rate of NAC necrosis observed in GG reduction is due to lack of blood supply to the NAC. Therefore, most surgeons prefer a free nipple graft reduction mammaplasty for GG. Although this technique remains simple and reliable, it has several disadvantages, such as hyposensitivity, loss of lactation, flat projection, and unmatched pigmentation of the NAC [9-11].
Four arterial sources are mainly responsible for supplying blood to the NAC. These are branches originating from the lateral thoracic artery, internal mammary artery, anterior branches of the intercostal arteries, and branches from the highest thoracic arteries. The first and second sources mentioned above are the dominant arterial supply to this NAC region [12,13]. The LTA arises from the axillary artery and terminates in 2 or 3 branches near the lateral margin of the areola. The LTA was located between the subcutaneous fat tissue and the mammary gland in this course. The vein, a single vena comitans, closely accompanied the artery [14]. In 1978, Harii et al. first used the free LTA flap for defects in the head, neck, and hand [15]. In fact, the LTA flap has been used in local regional reconstruction (axilla, pectoral region, and arm) as an island or propeller flap or as free flap for various defects of the extremities and of the head and neck regions [14,16]. In 2022, Sharp et al. reported a patient in which a free LTA flap from the hypertrophic breast was used for contralateral breast reconstruction [17]. In 2018, Elmelegy et al. introduced a breast reduction technique in 50 patients with hypertrophic breasts. Based on preoperative identification of perforating vessels, whether originating from the internal mammary artery or LTA using a hand-held Doppler, the authors designed a parenchymal medial-lateral bipedicle bearing NAC following reduction mammoplasty that resulted in a meager rate of postoperative ischemia and necrosis of the NAC [18]. Basaran et al. described a breast reduction technique in which the major supply vessels of the NAC were determined by color Doppler ultrasonography, and the pedicles bearing NAC containing these vessels were designed for breast reduction [19].
In our patient, we used a handheld Doppler to locate and estimate the adequate caliber of LTA and internal mammary artery (IMA) branches. As a result, the LTA predominates the IMA branches and eventually reaches the outer circumference of the nipple-areola complex. Therefore, we chose these vessels as the primary blood supply for the NAC. The customized pedicles were made according to the vessel locations with a superior or superolateral-based design. In GG, the hypertrophic breast increases the LTA in both diameter and length to ensure adequate blood supply to the NAC. Using ultrasound, the diameter of the LTA branches is measured to be three times normal. The size of itself also increases with the development of the breast. However, the distribution of the perforator is different in each breast of the same person. Depending on the direction of the LTA vessels and the design of the axial flap that provides vascular supply to the NAC, we can easily create the proper projection of the breast. In our experience, the first thing is to identify which vessels supply for NAC and then decide which ones are the dominant. Each of them will have an impact on the flap design and the pedicle length to carry the NAC without necrosis. We found that resections as extensive as 4000g were well tolerated with nipple viability by customized pedicle reduction. Wound healing issues along the T-junction and reoccurrence have not been observed in this patient. The advantages of using the LTA flap are to create a large tissue flap when the breast is excessively hypertrophic; a long vascular pedicle with arterial external diameter. Possibility of sensory neurovascular flap; a part of the breast tissue can be maintained to ensure breastfeeding; ease of creating breast projection even when a large portion of the breast is removed. This technique can only be applied when LTA branches dominate over the IMS branches.
Conclusion
The customized pedicle constructed with preoperative perforator identification with a Doppler is an alternative technique for gestational gigantomastia reduction that preserves the NAC and breast contour.
References
- Dancey A. Gigantomastia- A classification and review of the literature. J Plast Reconstr Aesthet Surg 61 (2008): 493-502.
- Gerall CD and Jatoi I. Gestational gigantomastia. Surgery 165 (2019): 485.
- Alhindi N. A systematic literature review of the clinical presentation, management, and outcome of gestational gigantomastia in the 21st Aesthetic Plast Surg 47 (2023): 10-29.
- Fletcher M.B. Gestational gigantomastia: A case report and brief review of the literature. JAAD Case Rep 6 (2020): 1159-1161.
- Rezai S. Gestational Gigantomastia Complicating Pregnancy: A case report and review of the literature. Case Rep Obstet Gynecol 15 (2015): 892369.
- Lapid O. Breast reconstruction after mastectomy for gestational gigantomastia. Aesthetic Plast Surg 37 (2013): 388-391.
- Qin F. Management of gestational gigantomastia with breast reconstruction after mastectomy: case report and literature review. J Int Med Res 48 (2020): 300060520920463.
- Wamalwa AO. Surgical anatomy of reduction mammaplasty: a historical perspective and current concepts. S Afr J Surg 55 (2017): 22-28.
- Rooi A. Severe gestational gigantomastia: management challenges. S Afr J Surg 59 (2021): 195a-195c.
- Turkan H. Gestational Gigantomastia. J Breast Health 12 (2016): 86-87.
- Shoma A. Gestational gigantomastia: A review article and case presentation of a new surgical management option. Surg Innov 18 (2011): 94-101.
- Palmer JH and Taylor GI. The vascular territories of the anterior chest wall. Br J Plast Surg 39 (1986): 287-299.
- O'Dey DM, Prescher A, Pallua N, Vascular reliability of nipple-areola complex-bearing pedicles: an anatomical microdissection study. Plast Reconstr Surg 119 (2007): 1167-1177.
- Le-Quang C. Two new free flaps developed from aesthetic surgery I. The lateral mammary flap. Aesthetic Plast Surg 4 (1980): 147-157.
- Harii K, Torii S, and Sekiguchi J. The free lateral thoracic flap. Plast Reconstr Surg 62 (1978): 212-222.
- Kim JT. Lateral thoracic perforator flap: additional perforator flap option from the lateral thoracic region. J Plast Reconstr Aesthet Surg 64 (2011): 1596-1602.
- Sharp OL. Breast augmentation using a free lateral thoracic artery perforator flap from the contralateral breast: A case report. Microsurgery 4 (2022): 176-180.
- Elmelegy NG. Treatment of gigantomastia using a medial-lateral bipedicle reduction mammoplasty: The role of doppler-assisted preoperative perforator identification. Aesthetic Plast Surg 42 (2018): 73-79.
- Basaran K. Ultrasonographically determined pedicled breast reduction in severe gigantomastia. Plast Reconstr Surg 128 (2011): 252e-259e.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 