Admission and Discharge Unit: Erie Shores Health Care Experience
Kristin Kennedy1, Katelyn Dryden1, Neelu Sehgal1, Rashoo Brar1, Matt Bessey, Holly Kettle1, Patti Fields1, & Munira Sultana*,1,2
1Erie Shores HealthCare, 194 Talbot St. W. Leamington, Ontario N8H 1N9
2WE SPARK HEALTH Institute, 401 Sunset Ave, Windsor, ON N9B 3P4
*Corresponding author: Munira Sultana, Erie Shores HealthCare, 194 Talbot St. W. Leamington, Ontario N8H 1N9, Canada.
Received: 14 June 2025; Accepted: 23 June 2025; Published: 10 July 2025
Article Information
Citation: Kristin Kennedy, Katelyn Dryden, Neelu Sehgal, Rashoo Brar, Matt Bessey, Holly Kettle, Patti Fields, & Munira Sultana. Admission and Discharge Unit: Erie Shores HealthCare Experience. Fortune Journal of Health Sciences. 8 (2025): 649-657.
View / Download Pdf Share at FacebookAbstract
Erie Shores HealthCare (ESHC) has effectively addressed key challenges in Canadian Emergency Departments, including overcrowding and long treatment times that impact patient care and staff morale. To combat these issues, ESHC launched an innovative Admission Discharge Unit (ADU) pilot project in December 2023. This initiative aimed to create a scalable model that reduces dependence on traditional funded-bed approaches while upholding high-quality standards and enhancing access. The ADU model alleviated emergency congestion by minimizing bottlenecks and optimizing resource allocation, leading to improved hospital efficiency and a shorter idle time for beds. As a result, the pilot project facilitated quicker admissions, boosted patient satisfaction, and reduced the hospital's overall cost of care. This strategic move not only improved patient outcomes but also helped mitigate burnout among healthcare providers, addressing the pressing needs of the post-pandemic healthcare environment.
Keywords
Emergency Department wait-time, Admission, Discharge, Care model
Article Details
Background
Emergency departments (ED) are among the most challenging areas of the healthcare system when it comes to patient delays. Patients can arrive at the emergency department through various channels, including walk-ins and ambulances. Depending on the nature of the emergency, patients may be directed to either an ambulatory or non-ambulatory section of the department. Upon arrival, the patient or a companion checks in with a receptionist to provide background information and then meets with a nurse for triage. Patients are treated by physicians and nurses in designated treatment rooms, which may specialize in specific injuries (such as orthopedics) or categorized by the level of urgency. Before treatment can begin, various tests such as lab work, X-rays, CT scans, or MRIs may be required. Sometimes, patients need to be moved to an operating room for surgery. Once emergency treatment is complete, the patient may need to be admitted to the hospital, where they may face additional processes and delays. Finally, after the patient has been treated and is ready for discharge, the discharge process occurs, and the bed must be prepared for the next patient. According to Hall [1], the service demand can be so high that the ED rarely has a break from waiting patients, especially in community hospitals. This situation arises either from the ED not having enough capacity or the hospital wards being unable to accommodate the influx of patients. Several factors are responsible for higher demand for services, such as higher patient acuity, prolonged ED evaluations, inadequate inpatient bed capacity, nursing shortage, problems with access to on-call specialists and the use of ED by those with no other alternative to medical care, such as the uninsured [2]. Unlike conventional queueing models, the rate at which patients arrive at the system often exceeds its capacity to serve them over extended periods, leading to a dysfunctional situation where the queues do not grow indefinitely solely because some patients leave without being seen when the wait becomes intolerable [1]. Some patients may return later, possibly in worse condition, while others may never receive treatment [1]. Conversely, fewer patients leave when waiting times decrease, which can cause the wait to build up gradually [1].
EDs across Ontario face persistent challenges, including overcrowding, long wait times, and strained resources, compromising patient care and outcomes (Registered Nurses' Association of Ontario [3,4]. Due to the lack of space or the funds to expand or add staff, more and more hospitals are motivated to look at improving their flow of patients by studying bottlenecks and limitations in their process that artificially add to the problem. Our hospital, Erie Shores HealthCare (ESHC), is no exception. The 72-bed hospital serves 468,019 people across Greater Windsor-Essex County, and the region's population has increased by 17.3% from 2016 to 2024 [5]. Moreover, ESHC expanded its catchment area by 75000 to reduce regional EMS code blacks in 2018 [6] and the EMS volume increased by 50% from 2018 to 2025. The region is also experiencing a rise in the senior population, which accounts for over 70% of hospital inpatient days, further straining healthcare services [7]. As the population expands, so does the demand for the ED, resulting in more visits and potential overcrowding. Respiratory season adds extra strain to the ED as more people seek care for respiratory illnesses. The influx of temporary foreign workers creates an additional seasonal surge of approximately 14,000 in healthcare demand at ESHC, with these workers relying on ED for acute care [5]. Therefore, innovative, practical ways to reduce ED wait times and an additional burden on our hospital resources were warranted. We aimed to create an innovative care model to streamline patient transitions within the hospital, reduce bottlenecks, and improve overall efficiency in patient care.
Literature published since 2000 discusses various care models that hospitals can implement to improve patient care and throughput in EDs [1,8-13]. Key care model components are summarized below:
A. Infrastructure/real estate modification:
- ED fast track: A dedicated area to treat lower acuity patients quickly, aiming for a 60-minute throughput time. Efficient tools like checkbox clinical records and point-of-care testing can help manage non-urgent cases, potentially handling 40-50% of ED volume, which enhances patient satisfaction and increases capacity for higher acuity cases.
- Establishing a Clinical Decision Unit: A separate 8-12 bed unit for patients needing more care but not necessarily a full hospital bed can substantially reduce admissions by up to 30% and shorten patient stay durations from 24-48 hours in traditional beds to 10-14 hours, thereby freeing up inpatient beds.
- Establishing a Rapid Admission Unit/Zone (RAZ): This area can assist patients awaiting hospital admission when beds are not available.
- Discharge lounge: A space for patients waiting to be discharged, providing a comfortable environment to complete logistical tasks like prescription fulfillment and transportation arrangements. This can expedite discharge times and make beds available for incoming patients.
B. Realtime data analysis for resource management
- Analyze staffing data: Collect historical data on hospital admissions to identify patterns over time, which helps in understanding demand and capacity ratios.
- Adjust staffing to demand: After identifying demand patterns, healthcare facilities can optimize staffing during peak times, balancing technical and nursing staff to meet service needs.
- Prepare contingency plans: Establish a backup system for unexpected demand, including on-call staff or plans for reallocating personnel from other departments to manage sudden surges effectively.
- Ensure resources for management team: Managers need access to precise data and robust information systems to create effective demand management strategies and adjust staffing accordingly.
- Reduce unnecessary utilization: The healthcare providers need to identify and reduce confirmatory tests that do not contribute to patient diagnosis or treatment but are performed for risk management purposes. Ongoing monitoring on test utilization and variations among physicians can minimize unnecessary testing.
C. Synchronize care delivery
- Focus on getting the patient to the provider: Most patients want to see the physician, so processes that interfere with that should be reexamined.
- Evaluate, delete, or retime processes that do not enhance turnaround time: This includes streamlining triage when there is a delay due to a lack of beds, reducing assessment exams, and reducing duplicate questions between the registration/admitting staff and the physician nurse team (e.g., “why are you here today?”).
- Establish protocols for top diagnoses: Protocols can greatly reduce delays by streamlining the transition of patients from one step in the treatment process to another.
- Based on protocols, initiate action: Once a protocol has been agreed upon, a patient who arrives in the ED with a condition for which a protocol is in place can be moved immediately through the steps, eliminating the delays that often occur in ordering appropriate tests.
- Reconnect services within the hospital: This is not uncommon for hospitals, as each department traditionally operates with its own “silo” accountable for the individual performance and service delivery standards. Many of the flow issues facing most EDs can be resolved with a synergistic process involving different departments (e.g. pharmacy, lab, housekeeping).
D. Active engagement of hospital physicians
To improve ED and inpatient throughput, hospitals need active involvement from physicians, as nurses and managers can only do so much. Important strategies for collaboration include recognizing shared benefits and leveraging data. To enhance capacity and flow, hospitals can implement strategies such as a) creating a hospitalist program, b) developing care maps for common admissions, c) hiring nurse practitioners and physician assistants to assist with discharges, d) utilizing clinically-based case managers for efficiency, e) enforcing admission and discharge policies, d) analyzing length-of-stay and discharge timing to identify outliers, e) appointing a "bed czar" to manage bed utilization, f) adjusting scheduling for ancillary tests to support timely discharges, and g) conducting staff surveys to identify improvement opportunities.
E. A transition unit
- Establishing a centralized command center with real-time bed tracking to manage admissions and discharges more effectively, thereby preventing bottlenecks.
- Ensuring discharges from inpatient units occur before peak ED admission times to minimize waiting for beds and improve throughput.
- Implementing proactive strategies to anticipate demand from the ED, helping receiving units prepare for incoming patients and maintain smoother transitions.
- Creating refined bed control protocols to address temporary surges, especially during high-demand periods like flu season.
- Holding regular meetings with defined goals and participation from key staff to manage bed resources effectively.
- Establishing clear roles within each department to monitor the workload and develop action plans for temporary surges. This involves reallocating resources based on immediate needs, such as prioritizing bed cleaning teams over routine housekeeping.
- Revitalization of the house supervisor’s role responsible for bed management should be refocused to prioritize capacity management.
- To reduce delays in patient discharges, hospitals can streamline access to nursing homes, rehabilitation centers, and outpatient resources.
Although several strategies outlined in the article have already been implemented to streamline patient flow, we continue to face significant challenges in transitioning patients from the ED to the inpatient unit. Despite these efforts including improved communication protocols, early bed assignment processes, and interdisciplinary huddles—bottlenecks persist due to factors such as limited bed availability, delays in discharge from inpatient units. These ongoing issues highlight the complexity of patient flow and underscore the need for more robust, system-wide solutions to ensure timely and efficient transfers from the ED.
Methods
The project used a mixed-method research approach, allowing the team to collect and analyze both quantitative and qualitative data within the same project [14]. Mixed method research allowed us to draw on the potential strengths of qualitative and quantitative methods [15], exploring diverse perspectives and uncovering relationships between the intricate layers of our multifaceted care model. As providers and policymakers strive to ensure quality and safety for patients and families, mixed methods helped us to explore contemporary healthcare trends and practices across increasingly diverse practice settings. The following steps were adopted:
- An environmental scan was conducted to identify possible bottlenecks affecting ED patient flow at ESHC, along with a review of organizational reports. The aim was to create an innovative care model utilizing the available resources catered to the hospital’s needs.
- A pilot project (a case series evaluated with before-after intervention) was implemented to test the impact of the innovative care model. The population of interest was patients attending the ED, the intervention was a separate admission and discharge unit (ADU), and the control was the historical data points. The outcomes of interest were a) reduced ED wait time, b) reduced bed idle time, c) bed capacity improvement, and d) overall cost reduction. The timeline for data analysis was one year. The data collected as part of routine hospital administration was used to descriptively analyze the feasibility and impact of the pilot project on the outcomes of interest.
- During the pilot project implementation, a qualitative study using a series of semi-structured interviews and a post-discharge survey based on the constructivism paradigm position [16] using an interpretive description approach [17] was conducted. Thematic analysis for the interview data and descriptive analysis for the survey data was used for data inference.
Results
Environmental Scan
An environmental scan originated in a business context as a tool for retrieving and organizing data for decision-making [18]. Environmental scans have been mainly used to investigate external factors interpreted as keys to success and affect an organization's future [19, 20]. In healthcare, an environmental scan aims to help design a care model that is geared toward and incorporates the needs of specific communities [21]. The hospital's data [22] highlight significant challenges, such as EMS calls to ESHC surged by 32% compared to 2023, and ED admissions to the hospital have increased by 34%. Moreover, the number of individuals without a family physician in Windsor-Essex has increased by 22% from 2022 to 2023 [23], leading to a higher volume of ED patients and limited infrastructure to support efficient patient transitions. It is also worth mentioning that ESHC ranked the 6th highest (123%) overall of hospitals in Ontario for occupancy rates in 2024-25 (22, 24).
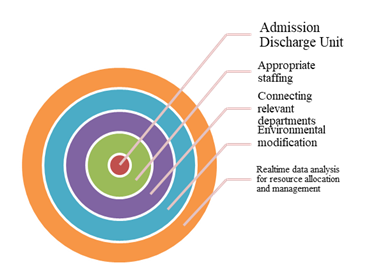
From the environmental scan, we learned that the current staffing model can potentially delay discharge processes for not having a dedicated team streamlining the process. A bed czar could also expedite ESHC's discharge times and make beds available for incoming patients. Establishing clear admission and discharge protocols and synchronizing care delivery across departments were also warranted to help streamline patient transitions and mitigate delays caused by departmental silos. Implementing adjustable staffing based on demand patterns and preparing contingency plans can further enhance the response to unexpected surges in ED visits. By ensuring that management teams can access precise data, ESHC can develop robust demand management strategies, ultimately improving patient care and resource utilization. Post-discharge care that includes thorough medication reconciliation offers significant benefits for hospitals by enhancing patient safety, reducing readmission rates, and improving overall care quality. Ensuring that patients leave the hospital with a clear, accurate, and up-to-date medication list along with post discharge follow up appointment with their family care providers or specialists also reduces the likelihood of costly readmissions. We realized our ED is not built to track lower acuity patients quickly. We also did not have a discharge lounge or space for patients waiting to be discharged, which provided a comfortable environment for completing logistical tasks like prescription fulfillment and transportation arrangements. After a series of discussions among the senior leadership team and relevant departments, we decided to implement an innovative model (intervention) that was tailored to ESHC's needs and the population we serve. This intervention was an Admission and Discharge Unit (ADU) (Figure 1).
The admission and discharge Unit, a relatively new concept [25], is a key administrative service that manages the admission and discharge of patients in healthcare facilities. Typically operating 24/7 for all admissions and discharges qualifying the hospital’s eligibility criteria, it also accommodates emergency admissions through 24-hour units. The process begins with patients receiving a confirmation letter and pre-admission forms, followed by a clinical assessment [25]. Upon arrival, administrative tasks are verified, clinical assessments and consent forms are reviewed, and financial matters are settled (national health insurance, OHIP, in Canada) before the patient is transferred for treatment [23]. In some specialized cases, planned admissions may bypass the Admission Unit, while unplanned admissions are handled by emergency staff [11]. The unit also manages patient data through electronic and paper records [10]. A Discharge Lounge may also be available for patients awaiting discharge or transfer, streamlining the discharge process by the facility's operational policies [4]. Our adopted ADU model is explained in detail in Table 1.
Table 1: Structure of ESHC ADU
*RN=Registered Nurse, RPN= Registered Practical Nurse, FT= Full Time, PT=Part Time, ADU=Admission Discharge Unit, ED=Emergency Department, RAZ= Rapid Assessment Zone, IP=In-patient
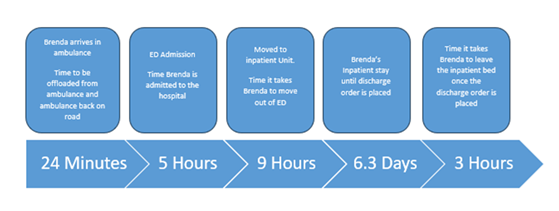
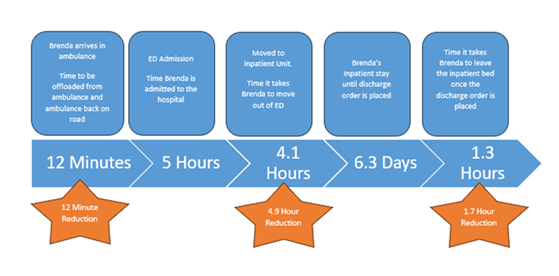
Pilot project
Despite being a small rural hospital, ESHC established ADU in November 2023, informed by an environmental scan of the hospital’s ED experience to break the vicious cycle of system-wide demand, dysfunction, and delay. The process was iterative and catered to the ESHC service delivery model. The evaluation of the before-after intervention on the outcomes of interest revealed that patients spent an average of 5.4 hours less in ED and acute beds (Table 2). For example, in 2022-23, it would have taken 24 minutes to offload a patient from the ambulance to ED, five hours to admit the patient at ED, nine hours to move the patient from ED to the in-patient unit, 6.3 days from in-patient stay to discharge order in place, and three hours to leave the in-patient bed once the discharge order is placed (Figure 2). After the introduction of ADU, it took 12 minutes to offload a patient from ambulance to ED (a 50% reduction), five hours to admit the patient at ED, 4.1 hours to move the patient from ED to in-patient unit (a 50% reduction), 6.3 days from in-patient stay to discharge order in place, and 1.3 hours to leave the in-patient bed once the discharge order was placed (a 43% reduction) in 2024-25(Figure 3). We also noticed an improved bed efficiency (4,480 hours were gained for emergency bed availability and 1,523 hours for inpatient bed availability).
Table 2: Admission Discharge Unit’s hospital wide impact
|
Emergency Department |
IP* bed |
|||
|
ED* visits |
ED bed Idle Time |
Admits |
IP bed idle time |
|
|
No ADU* |
7,247 |
9 hours |
787 |
3 hours |
|
ADU fully implemented |
8,326 |
4.1 hours |
896 |
1.3 hours |
|
*ADU=Admission Discharge Unit, ED=Emergency Department, IP=In-patient |
||||
The hospital’s administrative data from ED performance also revealed that ESHC decreased Admit No Beds (ANB) at 8 am by 2.4 beds (from 3.9 in 2023-24 to 1.5 in 2024-25), decreased admitted Length of Stay (LOS) by 8.7 hours (from 31.7 hours in 2023-24 to 23 hours in 2024-25), and decreased Time to Inpatient Bed (TIB) by 11.2 hours (from 25.3 hours in 2023-24 to 14.1 hours in 2024-25) while maintaining an Ambulance Offload Time (AOT) of less than 25 minutes ranking as number one in Ontario for 14 consecutive months. Regarding cost and care comparison, ADU implementation has increased ED visit capacity by 15% compared to pre-implementation levels, allowing us to effectively manage patient volumes exceeding 160% capacity during surge season and 150% during regular off-peak times we are experiencing. This enhanced capacity has also provided additional Emergency Medical Services (EMS) diversion space. This increase in diversion space has assisted Windsor Essex in reducing EMS code blacks. Operating nine inpatient beds under the traditional funding model costs $4.6 million annually. In contrast, the ADU model, featuring nine ADU beds and eight discharge recliners, costs significantly more than the ADU model-which includes nine ADU beds and eight discharge recliners-reduces annual costs by approximately 39%. Additionally, the recliners offer the equivalent capacity of about four inpatient beds. Furthermore, ADU beds offer critical surge overflow capacity during peak periods, ensuring additional inpatient support when needed.
Qualitative study
An interpretive description approach [17] was used to understand observers' perspectives on the performance of ADU at ESHC. The methodology allowed us to develop a deep understanding of subjective experiences and the practical importance of ADU. The informants (N=11) included patients and their family members using ADU services and ADU staff. A 30-minute, in-person and over-the-phone semi-structured interview was conducted. The interview transcripts were analyzed thematically. Three themes emerged from the informants' subjective accounts: 1) welcoming space, 2) Patients clearly understood their next steps after discharge, and 3) supportive work environment.
Welcoming space: An overwhelming response (8 out of 11 respondents) to ADU was that they felt valued and welcomed while waiting at ADU. A quote from a respondent speaks volumes about their feelings:
"Whoever came up with the idea of a separate unit for admitted and discharged patients is a genius. On my previous visit to this hospital, I was one of those waiting on the stretcher in the hallway. Now, I can wait in a welcoming space with my family and friends."
Patients clearly understood their next steps after discharge: To ensure seamless care delivery, ADU added a follow-up phone call service. All patients and their family members (N=9) appreciated the follow-up calls. They reported being better supported with medication counselling and navigating the pathways related to their care after their discharge through phone calls. "The whole process was professional. He did not take the pain medication during discharge as he thought he didn't need any. Thank you for calling. I think he needs his pain medication."
Supportive work environment: The management noticed that the nurses are more interested in working with admitted and discharged patients. For example, a manager commented, "South nurses requested to have shifts at ADU. This is amazing."
The patient satisfaction survey also revealed an overall satisfaction with discharges was 90% when ADU was added compared to overall satisfaction with discharges being 78% when ADU was absent.
Discussion
ED admissions and patient discharges significantly contribute to overall health expenditures, with the decision to admit or discharge patients being complex and influenced by both clinical and non-clinical factors. When bed availability is limited, patients often experience delays in receiving appropriate care, including prolonged stays in the emergency department. The cumulative impact of these pressures creates a cycle of stress and inefficiency that undermines the hospital's ability to deliver optimal care. The post-pandemic landscape of health has changed, and at ESHC, we are seeing increased volume and higher acuity. When hospitals are unable to admit patients from the ED due to a lack of available beds, it leads to prolonged waiting times, delayed diagnoses, and treatment interruptions. This bottleneck not only increases the risk of adverse health outcomes but also places immense stress on healthcare providers. For healthcare staff, the constant strain of managing high patient volumes without adequate resources contributed to burnout, emotional exhaustion, and job dissatisfaction. These challenges also lead to a reduction in the hospital's ability to deliver timely and attentive care. However, by identifying and implementing effective solutions, we can mitigate these negative impacts and improve hospital efficiency. We understand that healthcare delivery models are unique and cannot be approached with a one-size-fits-all mindset. Emphasizing a community-centered approach to ESHC's ADU model allowed us to treat our patients as individuals rather than just numbers on a bell curve. Our care was tailored to meet their specific needs. To achieve this, we relied on three key principles grounded in the science of change and evolution [26]:
- Variation: We explored different approaches to discover what works best for the community we served, recognizing the individuality of each patient’s healthcare journey.
- Selection: Based on our experiences, we choose strategies that aligned with the needs of our patient population and staff.
- Retention: We encouraged our staff to stick with the effective strategies while remaining open to adjustments as we grew and evolved.
By applying these principles, we ensured that our innovative care model (ADU) is both personalized and adaptable, reflecting the ever-changing nature of the emergency department environment. A related study conducted by Cheng and colleagues [12] at Sunnybrook Hospital supports our approach. The study identified that the factors influencing the failure to meet target wait times for high-acuity discharges and admissions were mainly under the hospital's control. They recommended that hospitals tailor their strategies for reducing emergency department length of stay (ED LOS) by analyzing their specific patient population and resource requirements [12]. Similar to our experiences with ADU, a recent doctoral thesis [27] showed that optimizing admission decisions, reducing unnecessary hospitalizations, and adjusting the timing of decisions can be beneficial. However, the study [27] reported that delaying admissions could allow for further diagnostics, which helped providers make more informed choices. For instance, increasing diagnosing time from 1 hour to 2 hours in ED significantly lowered admission rates from 41.6% (95% CI: [40.6, 42.7]) to 32.7% (95% CI: [32.2, 33.2]) for patients with abdominal pain [27]. The longer ED wait time allowed providers to identify patients better to discharge. Therefore, reducing waiting time alone is not a sole indicator of better patient care outcomes.
Warren [28] reported that patients experiencing a delay in transferring from ED to inpatient bed often felt uncertainty, frustration, disappointment, and concern because they perceived that their functional recovery was compromised because of delayed access to inpatient care. The phenomenological causes for such emotional experiences are rooted in a sense of no or little control over the process. Our qualitative enquiry echoed this finding with our patients’ overwhelmingly positive response about ADU despite having comparatively longer wait times.
A key enhancement to this model was the integration of a pharmacy technician into the discharge lounge. This addition resulted in a marked reduction in post-discharge clarification calls from external pharmacy partners regarding exit prescriptions. By addressing potential prescription errors at the point of discharge, the need for follow-up involving clerks, pharmacy technicians, and physicians was minimized. This not only streamlined the discharge process but also reduced the workload on clinical and administrative staff, contributing to a more seamless and efficient patient transition from hospital to home, echoing Dautzenberg’s [29] work. An equally impactful advancement of the ADU model following Hall’s [1] principles was the optimization of nursing resources on inpatient units for both admissions and discharges. By centralizing these processes within the ADU, bedside nurses were relieved of the time-intensive tasks associated with admission reviews and discharge coordination. This allowed them to dedicate more time to direct patient care and clinical priorities. Standardized operating procedures within the ADU ensured consistent, high-quality transitions for all patient populations. On average, this model returned approximately two hours per admission or discharge to unit-based nurses, enhancing their capacity to address ongoing care needs or to immediately focus on newly admitted patients. For discharges, this efficiency also translated into improved patient flow and faster bed turnover, directly supporting hospital-wide capacity management. This approach reflected a practice model that not only improved workflow efficiency but also elevated the overall quality, safety, and continuity of care at ESHC. To further support safe transitions and reduce ED revisits, the ADU team conducted follow-up phone calls with patients discharged through the lounge. These calls, made within 24 hours post-discharge, aiming to identify any gaps in care, clarify discharge instructions, and connect patients with additional resources as needed. This proactive outreach aligned with the relevant works [1, 29].
Conclusion
ED overcrowding is a complex issue as the process of admission and discharge is often non-linear and involves both clinical and non-clinical factors. A rigorous improvement science approach can identify various factors and solutions to promote both top-down and bottom-up strategies for addressing overcrowding, including system design, accountability measures, and continuous quality improvements. However, relying solely on small efficiency gains to alleviate ED access block without addressing capacity challenges will be insufficient. Given that the risk of deteriorating health conditions and death for ED patients is associated with increasing ED LOS, the time gains associated with our ADU project could improve patient outcomes. In a rural Canadian setting, the strategic optimization of resources is not just beneficial—it is essential for transforming healthcare delivery and dramatically improving patient outcomes. By harnessing limited resources effectively, healthcare facilities can enhance access and operational efficiency, ensuring that every patient receives timely and high-quality care. This proactive approach not only amplifies the impact of available services but also cultivates a robust and sustainable healthcare model that directly addresses the unique challenges faced by rural communities. Therefore, we believe our innovative ADU care model can be potentially replicated and scaled in similar settings. The ADU model is our commitment to best resource utilization, serving as a powerful catalyst for meaningful change in rural healthcare, propelling us toward a healthier future.
References
- Hall R. Patient Flow: Reducing Delay in Healthcare Delivery (2nd Ed). Springer New York Heidelberg Dordrecht London (2013).
- American College of Emergency Physicians, ACEP. Responding to emergency department crowding: A guidebook for chapters. American College of Emergency Physicians, ACEP Dallas, TX (2002).
- Registered Nurses’ Association of Ontario. Admissions and discharge guidelines: Health strategy implementation project (2003).
- Registered Nurses’ Association of Ontario. Care transitions (2014).
- Erie Shores HealthCare. Strategic plan: 2021-2023 (2024).
- CBC News. Windsor-Essex ambulance offload delays down by 7K hours with new protocol and tech. (2019).
- Windsor Regional Hospital. Quality improvement plan (QIP) narrative for health care organizations in Ontario (2017).
- Bahari A, Asadi F. A simulation optimization approach for resource allocation in an emergency department healthcare unit. Global Heart 15 (2020): 14.
- Matukaitis J, Stillman P, Wykpisz E, Ewen E. Appropriate admissions to the appropriate unit: a decision tree approach. Am J Med Qual 20 (2005): 90-97.
- Bahalkeh E, Hasan I, Yih Y. The relationship between Intensive Care Unit Length of Stay information and its operational performance. Healthcare Analytics (2022).
- Cheng I, Lee J, Mittmann N, et al. Implementing wait-time reductions under Ontario government benchmarks (Pay-for-Results): a Cluster Randomized Trial of the Effect of a Physician-Nurse Supplementary Triage Assistance team (MDRNSTAT) on emergency department patient wait times. BMC Emerg Med 13 (2013): 17.
- Cheng I, Zwarenstein M, Kiss A, Castren M, et al. Factors associated with failure of emergency wait-time targets for high acuity discharges and intensive care unit admissions. CJEM 20 (2018): 112-124.
- Ngo H, Forero R, Mountain D, et al. Impact of the Four-Hour Rule in Western Australian hospitals: Trend analysis of a large record linkage study 2002-2013. PLoS One 13 (2018): e0193902.
- Shorten A, Smith J. Mixed methods research: expanding the evidence base. Evid Based Nurs 20 (2017): 74-75.
- Greene JC, Caracelli VJ, Graham WF. Toward a conceptual framework for mixed method evaluation designs. Educ Eval Policy Anal 11 (1989): 255–74.
- Lincoln Y, Guba E. The constructivist credo. Y. S. Lincoln, E. G. Guba. (Eds.). Walnut Creek, CA: Left Coast Press, Inc (2013).
- Thorne S. Interpretive description: Qualitative research for applied practice (2nd ed) (2016).
- Aguilar FJ. Scanning the business environment. New York, NY: The Macmillan Company (1967).
- Muralidharan R. Environmental scanning and strategic decisions in multinational corporations. Multinat Bus Rev 11 (2003): 67–87
- Albright KS. Environmental scanning: radar for success. Inf Man J 38 (2004): 38–45
- Graham P, Evitts T, Thomas-MacLean R. Environmental scans: How useful are they for primary care research? Can Fam Physician 54 (2008): 1022-1023
- Maru S. CTV News: How Leamington hospital is trying to manage persistent overcapacity as patient volumes rise. 2025. Retrieved from https://www.ontariohealthcoalition.ca/index.php/how-leamington-hospital-is-trying-to-manage-persistent-overcapacity-as-patient-volumes-rise/
- Maru S. CTV News: Surge in Windsor-Essex residents without family doctor reinforces calls for health teams. 2023. Retrieved from https://www.ctvnews.ca/windsor/article/surge-in-windsor-essex-residents-without-family-doctor-reinforces-calls-for-health-teams/
- Ontario Health. Operational direction: Rehabilitation and complex continuing care capacity and flow. 2025. Retrieved from https://www.ontariohealth.ca/news/operational-direction-rehab-ccc-capacity
- Nates JL, Nunnally M, Kleinpell R, et al. ICU admission, discharge, and triage guidelines: A framework to enhance clinical operations, development of institutional policies, and further research. Critical Care Medicine 44 (2016): 1553-1602.
- Gelder LV. Embracing your unique health journey: Why one size doesn’t fit all (2024).
- Avendano SAA. Counterfactual analysis in service systems (2023).
- Warren N, Walford K, Susilo A, et al. Emotional consequences of delays in spinal rehabilitation unit admission or discharge: A qualitative study on the importance of communication. Top Spinal Cord Inj Rehabil 24 (2018): 54-62.
- Dautzenberg L, Bretagne L, Koek HL, et al. Medication review interventions to reduce hospital readmissions in older people. J Am Geriatr Soc 69 (2021): 1646-1658.
Article Views: 521
Journal Statistics




Discover More: Recent Articles
Grant Support Articles
- Explicating the Role of miR-638 in the Pathogenesis of Exfoliation Syndrome and Exfoliation Glaucoma
- Contributing Factors to The Awareness of Health Risks of Geophagy Among Pregnant Women in Lubumbashi
- Support of Patients Admitted with COVID-19 at Public Hospitals in South Africa by the Family Members
- View More
© 2016-2026, Copyrights Fortune Journals. All Rights Reserved!