The Role of Prenatal and Postnatal Counseling in the Management on Disorders of Sex Development: A Review
Igor Gualberto1, Iana Gualberto2, Gil Guerra-Junior3, Rodrigo Ruano4, Raphael Liberatore Junior5 and Lourenço Sbragia*,5
1Universidade de São Paulo, Faculdade de Medicina, São Paulo, SP, Brasil.
2Universidade de Pernambuco, Faculdade de Ciências Médicas, Recife, PE, Brasil.
3Universidade Estadual de Campinas, Faculdade de Ciências Médicas, Campinas, SP, Brasil.
4University of Miami, Leonard Miller School of Medicine, Miami, FL, USA.
5Universidade de São Paulo, Faculdade de Medicina de Ribeirão Preto, Ribeirão Preto, SP, Brasil.
*Corresponding Author: Lourenço Sbragia, M.D.- Ph.D. Division of Pediatric Surgery Department of Surgery and Anatomy University of São Paulo, Ribeirão Preto School of Medicine Av. Bandeirantes 3900, Monte Alegre, 14049-900 Ribeirão Preto, SP, Brazil.
Received: 22 July 2025; Accepted: 30 July 2025; Published: 04 October 2025
Article Information
Citation: Igor Gualberto, Iana Gualberto, Gil Guerra-Junior, Rodrigo Ruano, Raphael Liberatore Junior and Lourenço Sbragia. The Role of Prenatal and Postnatal Counseling in the Management on Disorders of Sex Development: A Review. Fortune Journal of Health Sciences. 8 (2025): 917-925.
View / Download Pdf Share at FacebookAbstract
This study aims to review the literature and to investigate how prenatal and postnatal counseling interfere in subjects with Disorders of Sex Development (DSD). The articles were obtained through search on bibliographic databases: Web of Science, Scopus, Scielo, MEDLINE, and LILACS and selected using the guideline following the Joanna Briggs Institute scoping review protocol and answering. The search identified 181 articles. After the methodological screening, 7 studies were eligible for this narrative review. 16 cases of different types of DSD were evaluated in the studies. In this case, different types of prenatal and postnatal counseling were carried out to address the diagnosis. In most cases, prenatal counseling was based on a genetic point of view and postnatal was based on psychological and educational follow-up of the family. There are different manners to conduct prenatal and postnatal counseling in cases of DSD. However, the data shows that there is a lack of specific protocols for adequate counseling of patients and families in the context of DSD. In addition, previous studies have only described this aspect in superficial forms. Therefore, further investigations are necessary to establish a scientific protocol for this matter.
Keywords
Disorder of sexual differentiation; counseling; prenatal diagnosis; neonate
Disorder of sexual differentiation articles; counseling articles; prenatal diagnosis articles; neonate articles
Article Details
Background
The sex determination is a very complex event that involves not only genetic but also embryological and hormonal steps beginning around the 5th week of life from primordial germ cell (1). When defects occur in this development, it results in a disorder/difference of sex development (DSD), whose incidence is 1 in 4500 births (2). At the moment of discovering DSD, appropriate care should include interdisciplinary teams with effective communication structures and joint efforts regarding goals and settings to counseling parents facing the new challenge they need to face (3,4). The prenatal diagnosis of sex can be suspected by prenatal ultrasonography since the 70s with significant improvement in the last 2 decades (5). Non-invasive prenatal testing for sex diagnosis has been used since the end of the 90s and the determination of cell free DNA can be done beyond 10 weeks of gestation (6). Because of that, there is a current gap in the literature addressing how to offer a consistent evaluation of discordant prenatal findings (7). Even thought, the sex diagnosis during gestation using only ultrasound or both methods, can be discordant not only between the methods but also be discordant after birth (7-9). The routine use of prenatal ultrasound in pregnancy monitoring has allowed the early detection of a wide spectrum of congenital defects and has contributed to our understanding of their prenatal natural history (11,12). Ultrasound and magnetic resonance imaging have been used to improve prenatal diagnosis. Still, there may be the possibility of misdiagnosis resulting in errors in the medical approach, family anxiety, and economic damages. Therefore, the diagnosis must be correct, and the counseling must be given cautiously (13). The frequency of anomalies associated with a diagnosis of genital anomaly is unknown. It is estimated that 30% of hypospadias and 41% of ambiguous genitalia have an associated anomaly including fetal growth restriction (14,15). Prenatal genetic testing and counseling following the finding of atypical genitalia on prenatal ultrasound can help better identify the final diagnosis of the defect (16). In addition, these patients and their family need psychosocial support to encourage self- acceptance, process trauma, accept the experienced otherness and improve sexual satisfaction, as well as overall psychosocial well-being. This is particularly important when the diagnosis of DSD is made, pre or postnatal, so this study lists these measures and comment the evidence for them (17). For those reasons, this study aims to perform a scoping review on the role of prenatal and postnatal counseling in the management on DSD, to show how these behaviors can be better understood and promote a better quality of life for patients living with DSD and their families.
Materials and Methods
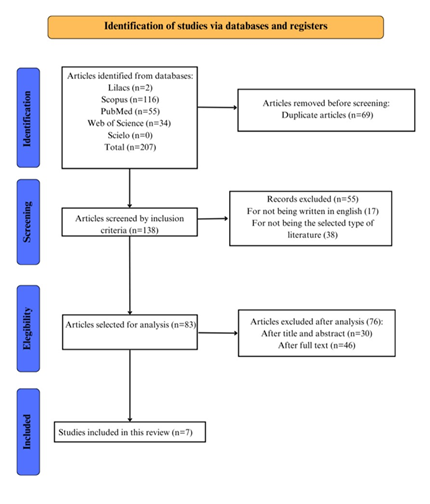
The present study is a scoping literature review, which allows a broad and comprehensive view of records on a respective topic and enables the synthesis of relevant evidence that addresses and informs clinical practice and identifies existing gaps in knowledge. This study follows the proposal of the Joanna Briggs Institute (18). The Population, Concept, and Context (PCC) strategy was used to formulate the guiding research question and the search strategy. Thus, we defined “P” as DSD subjects; “C” as the prenatal diagnosis and prenatal and postnatal counseling; and the last “C” as the outcome for the DSD patients. Considering this definition, the following guiding question was formulated: “How prenatal and postnatal counseling interfere in subjects with Disorders of Sex Development?”. The included articles had to contain the three elements of the PCC strategy, answer the research question, and be written in English. Articles written in other languages, in different time frames, that did not answer the guiding question, congress abstracts, book chapters, guidelines, roundups, expert opinions, brochures, published in non- indexed sources and reviews were excluded. The search for articles was conducted from November 26th to 27th, 2024 in the following databases: National Library of Medicine (PubMed/MEDLINE), SCOPUS, Web Of Science, SciELO, and Latin American and Caribbean Health Sciences Literature (LILACS/BVS). For the search, health descriptors (Decs/Mesh), keywords, and their alternative terms, and the Boolean operators OR and AND were used in all databases as presented in table 1. Three independent reviewers performed the selection process. Disagreements were resolved through consensus. As our purpose had a scoping nature, the risk of bias assessing eligible studies was not considered mandatory (19). This review followed the PRISMA statement and the checklist is attached as non published material.
Table 1: Databases and search descriptors selected according to PCC strategy.
|
Database |
Search strategies |
|
MEDLINE |
(“Ambiguous Genitalia” OR “Disorders of Sex Development” OR “Sex Development Disorders”) AND (“counseling”) AND (“Prenatal Diagnosis” OR “Fetal Screening” OR “Prenatal Screening” OR “Postnatal diagnosis”) |
|
WEB OF SCIENCE |
(“Ambiguous Genitalia” OR “Disorders of Sex Development” OR “Sex Development Disorders”) AND (“counseling”) AND (“Prenatal Diagnosis” OR “Fetal Screening” OR “Prenatal Screening” OR “Postnatal diagnosis”) |
|
LILACS AND SciELO |
(“Ambiguous Genitalia” OR “Disorders of Sex Development” OR “Sex Development Disorders”) AND (“counseling”) AND (“Prenatal Diagnosis” OR “Fetal Screening” OR “Prenatal Screening” OR “Postnatal diagnosis”) |
|
SCOPUS |
TITLE-ABS-KEY ( ( "Ambiguous Genitalia" OR "Disorders of Sex Development" OR "Sex Development Disorders" ) AND ( "counseling" ) AND ( "Prenatal Diagnosis" OR "Fetal Screening" OR "Prenatal Screening" OR "Postnatal diagnosis" ) ) |
Results
The database search identified 181 potential studies of which 63 studies were repeated. Of the remaining 118, 14 were excluded for not being written in English, 26 were excluded for being reviews, three for being book chapters, two for being letters, and one was excluded for being a brief communication. Twenty-six studies were further excluded after title and abstract analysis. Thirty-nine studies were finally selected, and 7 articles met all the inclusion criteria of the present study (Figure 1). A synthesis of all 7 selected articles is in the following Table 2. The results are presented in the form of tables and discursive reports. The PRISMA extension tool adapted for scoping reviews was applied to comply with the methodology. Of the 7 included studies, each one was written in a different year, which were 1995, 2003, 2012, 2014, 2015, 2017 and 2019, as shown in Table 2. The selected studies were conducted on various sites worldwide, allowing for a variety of patients. Five countries contributed to the results and all studies were conducted in only one country. Most studies took place in the United States (n = 3), followed by United Kingdom, Italy, Taiwan and Australia. Patients and their families differ in terms of ethnicity and culture since the included studies mostly took place in different locations. The populations also included children with Complete Androgen Insensitivity Syndrome (CAIS), True Hermaphrodite, 17Bhsd3 deficiency (46, XY female), Mixed Gonadal Dysgenesis, Cloacal Exstrophy and Smith-Lemli-Opitz syndrome (SLOS). The most commonly used research designs were case reports (n = 4), but there were also case series (n = 2) and retrospective study (n = 1). The characteristics of the selected articles can be seen in Table 2 (which describes the name of the authors, year of publication, country, study design, participants, objectives and prenatal and postnatal conducts). An early detection of several inborn errors, including DSD, can be allowed because of the increasing prenatal investigations methods, including ultrasound and genetic analysis techniques. Most of the studies explored the genotype-phenotype discordance identified in the routine clinical setting in women by ultrasound findings (22, 24-26), while other findings have been suggested through family genetic study (21) and based on an amniocentesis after IVF (23) and a significantly low estriol level on maternal serum screen (27).
Additionally, some studies specify what was considered an Abnormalities of sexual differentiation (22) or Disorder/Difference of sex development (23,26,27), conditions in which the development of chromosomal, gonadal or anatomic sex is atypical, while others just specify the disorder reported (21,24,25). DSD can be classified due to alterations in the number of sex chromosomes (including Turner syndrome and Klinefelter syndrome), 46,XY DSD and 46,XX DSD. Most patients underwent a karyotype confirmation test after ultrasound and genotype- phenotype discordance (23-27), but one patient declined chromosomal testing by amniocentesis (22). This patient returned in two weeks for a follow-up examination and the gender region appeared unchanged from the prior scan. A cesarean section was performed, and the baby underwent a plan to have the following tests as an outpatient: HCG stimulation test, FSH/LH, DHEA, and MIS labs. With the parents’ consent, an exploratory surgery for further evaluation was scheduled. One baby does not have antenatally diagnosis and shortly after birth it was noted that the patient had hypospadias with the urethral tip at the midshaft, some separation of scrotal tissue and undescended right testis with a normal left testicle, in addition to other diseases (24). The patient underwent the right laparoscopic gonadectomy at 15 months, for the undescended right testis, which pathology showed a streak ovary. The biopsy of the left gonad showed infantile testicular tissue. Fluorescent in situ hybridization chromosomal analysis from erythrocytes was performed to investigate mosaic variants and revealed 23 cells 45,X and 7 cells 46,X,psu idic(Y)(q12).
Some studies were concerned with informing that the multidisciplinary team may prepare parents for the complexity of genetic information and about challenges in the development of children with DSD (22-24,26,27). For them, parents should opt-in or opt-out of sex chromosome analysis and the option to terminate the pregnancy or not before counseling needs to be given (23,25,26). Only in one study, three families elected to terminate the pregnancy, two prior to 20 weeks gestation and another at 22+5 weeks gestation (26). Due to uncertain prenatal sex assignment, a clearly outlined management plan may be established (22,23,24), including avoiding pronouns at all points of care until the parents decide on sex assignment after birth (27). Additionally, the management postnatally includes follow-up with a child psychologist, geneticist, endocrinologist and gynecologist to promote the acceptance of clinical condition and gender assignment (22, 24, 27). For interdisciplinary management, studies suggest that early neonatal or childhood intervention with surgical interventions, hormonal interventions and biochemical investigations can help clarify diagnosis, because the evaluation of internal and external anatomy is incomplete in the prenatal setting due to technological limitations (26). Some studies describe surgical procedures and their findings, such as exploratory surgery (22,24), gonadectomy (21-24,26,27) and vaginoplasty (25).
Table 2: Synthesis of papers selected for the review.
Discussion
DSD represents a range of diseases that lead to differences in the development of the urogenital tract and in the clinical phenotypes (17). The characteristics of the disorder can directly impact the sex development and the best therapeutic option, especially when the child has ambiguous genitalia. Also, it is not completely understood the consequences of defects along this process, particularly in the aspects of predicting gender expression and identity (20). Most studies describe cases of patients in which genotype-phenotype discordance was an incidental finding (22-27). For genetic counseling and mainly to direct prenatal diagnosis, the androgen receptor gene (21,23), 7-dehydrocholesterol levels (26,27) and 5a-reductase (23) are useful to classify the DSD. In addition to karyotyping and marker tests, imaging exams are essential to guide the management of patients with suspected DSD. Previous studies have considered prenatal and postnatal ultrasound images and fetal magnetic resonance imaging (MRI) to identify internal reproductive organs (25, 27). When alone, prenatal ultrasound has a DDS detection rate of 15–24% (28). Despite the difficulty identifying these structures, fetal MRI led to early and complete identification of the spectrum of anomalies and facilitated verification of these findings by subsequent evaluations (25).
Having a specific diagnosis at delivery can provide information about gender of rearing assignment, endocrine function, fertility potential and the risk for gonadal malignancy (27). Four studies considered psychological support to patients with DSD and their family an essential conduct to be introduced as soon as possible to follow them to provide assistance in their decisional process and support them properly (22-24,27). Although these measures, factors determining sexual identity and gender change in these subjects are not yet clear at the moment (23). About challenging diagnosis, Radtke et al (24) reviewed 2 cases that illustrate the complexity of antenatal and postnatal management in Turner Syndrome (TS) patients who have 45,X mosaicism 45,X iso-Yp and 46,X,psu idic(Y)(q12). The study concluded that early management would incorporate a multidisciplinary team to help the family navigate the challenges of management and gender assignment. After analyzing the paper, it can be seen that, conceptually, both patients with a mosaicism with 45,X lineage and Y lineage at karyotype and genital ambiguity do not have Turner syndrome, but Mixed Gonadal Dysgenesis, which shows an incongruity in the reported diagnosis (17).
For those reasons, prenatal and postnatal counseling are fundamental for the family and the individual with DSD and ambiguous genitalia, clarifying, and educating about potential events or doubts, and is thus a way of welcoming patients with this type of condition (3,4). In most cases, prenatal counseling was based on a genetic point of view and the postnatal was a psychological and educational follow-up of the family. For prenatal evaluation, most studies suggest genetic counseling analysis on chorionic villi by amniocentesis (22,24,25,27), but Richardson et al (26) shows the possibility that the parents should opt-in or opt-out of sex chromosome analysis and the option to terminate the pregnancy or not before counseling needs to be given (26). In one paper, because of the uncertain sex assignment, a clearly outlined management plan was established, including avoiding pronouns at all points of care (27). The postnatal follow-up was based on gonadectomy, hormone therapy and sometimes reconstructive surgery (21,23,24), but also recommended treatment to repair other anomalies associated to the DSD [25]. Due to diagnostic difficulties, in some cases, it was necessary to use ultrasound after birth associated with genetic tests to prove DSD (23). These studies proposed early interventions such as removal of potentially carcinogenic streak gonads, time- critical hormonal interventions and biochemical investigations (26) joint to long-term follow- up with Genetics, Endocrinology, Gynecology, and Psychology in the DSD clinic (22,27). Although this article excluded literature reviews, book chapters and other forms of literature described in the methodology, an analysis of them was carried out with only one article answering the guiding question of this study (7). This review summarizes suggestions for prenatal counselling, neonatal management and postnatal care of DSD with a focus on common features that families face are addressed with particular emphasis on psychosocial support and a measured shared decision making approach.
Conclusion
In summary, there is a range of ways to conduct prenatal and postnatal counseling for families that live with ambiguous genitalia, but there isn’t a protocol in the literature that specifies general conduct to advise the families that receive this type of diagnosis in the period pre and postnatal. The types of conduct depend generally on the type of etiology in this spectrum and the conduct of the medical group that assists the DSD patients, for this reason, a design of a protocol could be interesting to help the medical care in this situation. Further discussions, consensus, and prospective studies are necessary to establish and propose protocols for managing those babies.
Acknowledgments
Lourenço Sbragia thanks São Paulo State Research Foundation – FAPESP and Igor José Nogueira Gualberto thanks the National Council for Scientific and Technological Development (PIBIC-CNPq).
Conflicts of interest: Authors declare no conflicts of interest.
Funding: Lourenço Sbragia thanks São Paulo State Research Foundation – FAPESP for scholarship # 2022/12021-1. Igor José Nogueira Gualberto thanks the National Council for Scientific and Technological Development (PIBIC-CNPq) scholarship (2021-22).
References
- Z Makiyan. “Studies of gonadal sex differentiation,” Organogenesis 12 (2016): 42-51.
- KT Mehmood and RM Rentea. “Ambiguous Genitalia and Disorders of Sexual Differentiation,” In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing 28 (2024).
- U Lampalzer, P Briken, and K Schweizer. “Psychosocial care and support in the field of intersex/diverse sex development (dsd): counselling experiences, localisation and needed improvements,” International Journal of Impotence Research 33 (2021): 228– 242.
- E Bennecke, K Werner-Rosen, U Thyen, et al. “Subjective need for psychological support (PsySupp) in parents of children and adolescents with disorders of sex development (dsd)” European Journal of Pediatrics 174 (2015): 1287–1297.
- LM Carlson and NL Vora. “Prenatal Diagnosis: Screening and Diagnostic Tools,” Obstetrics and Gynecology Clinics of North America 44 (2017): 245-256.
- L Carbone, F Cariati, L Sarno, et al. “Non-Invasive Prenatal Testing: Current Perspectives and Future Challenges,” Genes (Basel) 12 (2020): 15.
- Weidler, Erica M ab, Ochoa, Briellea, van Leeuwen, Kathleena b. Prenatal and postnatal evaluation of differences of sex development: a user's guide for clinicians and families. Current Opinion in Pediatrics 36 (2024): 547-553.
- S Manzanares, A Benítez, M Naveiro-Fuentes, et al. “Accuracy of fetal sex determination on ultrasound examination in the first trimester of pregnancy,” Journal of Clinical Ultrasound 44 (2015): 272–277.
- M Kearin, K Pollard, and I Garbett. “Accuracy of sonographic fetal gender determination: predictions made by sonographers during routine obstetric ultrasound scans,” Australasian Journal of Ultrasound in Medicine 17 (2014): 125–130.
- F Mackie, K Hemming, S Allen, et al. “The accuracy of cell-free fetal DNA-based non-invasive prenatal testing in singleton pregnancies: a systematic review and bivariate meta-analysis,” British Journal of Obstetrics and Gynecology 124 (2016): 32–46.
- JF Desforges, ME D’Alton, and AH DeCherney. “Prenatal Diagnosis,” New England Journal of Medicine 328 (1993): 114–120.
- SH Garmel and ME D’Alton. “Diagnostic ultrasound in pregnancy: an overview,” Seminars in Perinatology 18 (1994): 117–132.
- TM Crombleholme, MD’Alton, M Cendron, et al. “Prenatal diagnosis and the pediatric surgeon: The impact of prenatal consultation on perinatal management,” Journal of Pediatric Surgery 31 (1996): 156–163.
- M Alimussina, LA Dive, R McGowan, and et al. “Genetic testing of XY newborns with a suspected disorder of sex development,” Current Opinion in Pediatrics 30 (2018): 548–557.
- JM Heeley, AS Hollander, PF Austin, et al. “Risk association of congenital anomalies in patients with ambiguous genitalia: A 22-year single-center experience,” Journal of Pediatric Urology 14 (2018): 153.e1–7.
- Y van Bever, IAL Groenenberg, MFCM Knapen, et al. “Prenatal ultrasound finding of atypical genitalia: Counseling, genetic testing and outcomes. Prenatal Diagnosis 43 (2023): 162-182.
- LA Lee, CP Houk, SF Ahmed, et al. “International Consensus Conference on Intersex organized by the Lawson Wilkins Pediatric Endocrine Society and the European Society for Paediatric Endocrinology. Consensus statement on management of intersex disorders. International Consensus Conference on Intersex,” Pediatrics 118 (2006): e488-500.
- MD Peters, C Marnie, AC Tricco et al. “Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement 19 (2021): 3-10.
- AC Tricco, E Lillie, W Zarin, et al. “PRISMA Extension for Scoping Reviews (PRISMA- ScR): checklist and explanation,” Annals of Internal Medicine 169 (2018): 467-473.
- JA Indyk. “Disorders/differences of sex development (DSDs) for primary care: the approach to the infant with ambiguous genitalia,” Translational Pediatrics 6 (2017): 323–334.
- HR Davles, LA Hughes, and MN Patterson. “Genetic counselling in complete androgen insensitivity syndrome: trinucleotide repeat polymorphisms, single-strand conformation polymorphism and direct detection of two novel mutations in the androgen receptor gene,” Clinical Endocrinology 43 (1995): 69–77.
- P Switalski, M Cozzo, and C Hartfield, “Gender Abnormality: A Prenatal Ultrasound Diagnosis,” Journal of Diagnostic Medical Sonography 19 (2003): 188–191.
- G Russo, A di Lascio, M Ferrario, et al. “46, XY karyotype in a female phenotype fetus: a challenging diagnosis,” Journal of Pediatric and Adolescent Gynecology 25 (2012): e77-9.
- AC Radtke, C Sauder, JL Rehm, and PH McKenna. “Complexity in the diagnosis and management of 45,X Turner Syndrome mosaicism,” Urology 84 (2014): 919- 921.
- CY Chou, YC Tseng, and TH Lai. “Prenatal Diagnosis of Cloacal Exstrophy: A Case Report and Differential Diagnosis with a Simple Omphalocele,” Journal of Medical Ultrasound 23 (2015): 52–55.
- EJ Richardson, FP Scott, and AC McLennan. “Sex discordance identification following non-invasive prenatal testing,” Prenatal Diagnosis 37 (2017): 1298-1304.
- L Mohnach, S Mazzola, D Shumer and et al. “Prenatal diagnosis of 17- hydroxylase/17,20-lyase deficiency (17OHD) in a case of 46, XY sex discordance and low maternal serum estriol,” Case Reports in Perinatal Medicine 8 (2019): 20180009.
- MP Adam, PY Fechner, LA Ramsdell, et al. Ambiguous genitalia: what prenatal genetic testing is practical? Am J Med Genet A 158 (2012): 13371343.


 Impact Factor: * 6.2
Impact Factor: * 6.2 Acceptance Rate: 76.33%
Acceptance Rate: 76.33%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 