Assessment of Visual Acuity Following Nd:YAG Laser Posterior Capsulotomy: A Six-Month Prospective Study
Md Golam Faruk Hossain1, Md Miftahul Hossain Chowdhury2, Mazharul Hoque Bhuiyan*,3, Mohammad Mazaharul Islam4, Md Saiful Islam5, Dr. Moinul Hoque6
1Associate Professor, Department of Community Ophthalmology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Shahbagh, Dhaka, Bangladesh
2Associate Professor, National Institute of Ophthalmology & Hospital, Sher-e-Bangla nagar, Dhaka. Bangladesh
3Assistant Surgeon, National Institute of Ophthalmology & Hospital, Sher-e-Bangla nagar, Dhaka. Bangladesh
4Assistant Professor, Department of Community Ophthalmology, BSMMU, Dhaka, Bangladesh
5Assistant Professor, Department of Ophthalmology, BSMMU, Dhaka, Bangladesh.
6Associate Professor, Department of Community Ophthalmology, BSMMU, Dhaka, Bangladesh.
*Corresponding author: Mazharul Hoque Bhuiyan, Assistant Surgeon, National Institute of Ophthalmology & Hospital, Sher-e-Bangla nagar, Dhaka. Bangladesh.
Received: 17 June 2025; Accepted: 23 June 2025; Published: 07 July 2025
Article Information
Citation: Md Golam Faruk Hossain, Md Miftahul Hossain Chowdhury, Mazharul Hoque Bhuiyan, Mohammad Mazaharul Islam, Md Saiful Islam, Md Moinul Hoque. Assessment of Visual Acuity Following Nd:YAG Laser Posterior Capsulotomy: A Six-Month Prospective Study. Fortune Journal of Health Sciences. 8 (2025): 633 - 638.
View / Download Pdf Share at FacebookAbstract
Background: Posterior capsule opacification (PCO) remnants a communal difficulty following cataract surgery, significantly impacting visual outcomes worldwide. In Bangladesh, where access to innovative eye care can be stimulating, actual and safe interferences like Nd:YAG laser posterior capsulotomy are vital for renovating vision and refining quality of life for a large people affected by this condition.
Aim: To evaluate the effect of Nd:YAG laser posterior capsulotomy on visual acuity over a six-month period and to explore the association between the size of the capsulotomy and visual outcomes, along with observation of any clinically evident intra- or post-operative complications.
Methods: A prospective, cross-sectional study was conducted at BSMMU, Dhaka, from April 2022 to March 2023, concerning 81 pseudophakic patients with declined visual acuity due to posterior capsule opacification. Patients were nominated based on predefined inclusion and exclusion criteria, and all underwent Nd:YAG laser posterior capsulotomy executed by a single ophthalmologist using a uniform protocol. Pre-and post-procedure assessments included visual acuity, intraocular pressure, and comprehensive anterior and posterior segment checkups. Capsulotomy size was assessed using variable slit-lamp beam widths at various angles. Postoperative medications were prescribed for 15 days, and all patients were followed for six months. Statistical analysis was conducted using SPSS v26, with significance set at p <0.05.
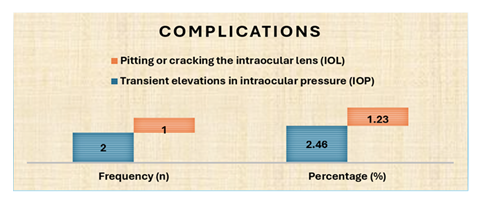
Results: A significant improvement in visual acuity was observed in both eyes following Nd:YAG laser posterior capsulotomy, sustained up to six months post-treatment (p < 0.001). The highest developments were seen with medium-sized (3 mm) capsulotomies. Visual outcomes varied significantly with capsulotomy size, mainly at one- and six-month post-procedure (p < 0.001). The procedure was well-tolerated, with minimal complications: transient intraocular pressure (IOP) rise in 2.5% and IOL pitting in 1.2% of cases.
Conclusion: Nd:YAG laser posterior capsulotomy significantly and sustainably progresses visual acuity with nominal complications; 3 mm capsulotomy size confirms optimal visual gains.
Keywords
<p>Nd:YAG, capsulotomy, visual acuity, PCO, complications, 3mm, LogMAR</p>
Article Details
Introduction
Posterior capsule opacification is the utmost common late complication following cataract surgery, important to reduced visual acuity and reduced patient satisfaction [1-3]. Nd:YAG laser posterior capsulotomy is the standard intervention for PCO, efficiently restoring vision in maximum cases [4-6]. However, the outcomes can differ based on capsulotomy size and energy situations [7]. Various studies have discovered the role of capsulotomy diameter in optimizing visual outcomes. 8-10 Medium-sized openings (~3mm) are frequently recommended to offer a stability between visual improvement and minimizing complications such as increased intraocular pressure or IOL damage [11-13]. Nevertheless, the optimum capsulotomy size remnants debatable due to uneven results [14-16]. The energy carried during the practice and the number of laser pulses have also been concerned in postoperative problems. Advanced energy levels correlated with transient IOP spikes and a higher incidence of IOL damage [17-18]. Current developments in laser technology and energy modulation may facilitate safer, more active treatments [19-20]. While short-term outcomes have been well recognized, long-term data, specially studies covering to six months, are comparatively scarce.5 [21-23]. Our study aims to evaluate the effect of Nd:YAG laser posterior capsulotomy on visual acuity over a six-month period and to investigate the association between capsulotomy size and visual outcomes. We also observed intra-and postoperative difficulties, such as transient IOP elevation and IOL pitting. In our prospective cohort of 81 patients, we detected substantial and sustained visual upgrading for six months, mainly in the 3mm capsulotomy group (p<0.001). Difficulty rates were low, with only 2.5% feeling IOP elevation and 1.2% supporting IOL damage. These results support the use of medium-sized capsulotomy to increase efficacy while minimizing risk.
Methods
This prospective, comparative cross-sectional study was conducted at the Ophthalmic Laser Unit of BSMMU, Dhaka, over a one-year period from April 2022 to March 2023. A total of 81 pseudophakic patients presenting with visual deterioration due to PCO were employed using purposive sampling. Informed written consent was obtained from all participants, and ethical principles were adhered to in accordance with the Declaration of Helsinki. Patients were included if they had good postoperative visual acuity directly following cataract surgery and then practiced visual decline. Exclusion criteria included patients less than three months post-cataract surgery or those with ocular comorbidities such as high myopia, corneal or retinal pathologies, amblyopia, uveitis, optic atrophy, or glaucoma. All laser procedures were performed by a single ophthalmologist using the VISULAS YAG III laser system (Carl Zeiss Meditec, Germany). Prior to the intervention, patients experienced complete ophthalmic evaluation with uncorrected and best-corrected visual acuity (UCVA and BCVA) assessed with a Snellen chart, IOP measurement using Goldmann applanation tonometry, slit-lamp biomicroscopy, and fundus examination. Pupil dilation was achieved with 5% phenylephrine hydrochloride and 0.8% tropicamide, and topical anesthesia was administered with 0.5% proparacaine hydrochloride. A contact lens (Ocular ABRAHAM Capsulotomy Lens, USA) was used for accurate laser directing. The capsulotomy size was assessed postoperatively using slit-lamp beam widths of 2 mm, 3 mm, and 4 mm at changing angles (0°, 45°, 90°, and 135°) in diverse patients.
Postoperative managing included topical management of Nepafenac, and a fixed combination of Brimonidine Tartrate and Timolol Maleate for 15 days. Patients were followed at regular intervals for six months post-procedure, with repetitive assessments of visual acuity, IOP, and anterior and posterior segment discoveries. Data was analyzed using Statistical Package for Social Sciences (SPSS) version 26. Continuous variables were presented as mean, standard deviation, median, and range, while categorical variables were expressed as frequencies and percentages. The Shapiro-Wilk test was applied to test for normality. The Wilcoxon signed-rank test was used to compare pre-and post-laser visual acuity. A p-value of less than 0.05 was measured statistically significant.
Results
Overall, patients practiced significant development in visual acuity following Nd:YAG laser posterior capsulotomy, continued over a six-month period. Among the capsulotomy sizes, 3 mm showed the most consistent visual gains, while the 2 mm size yielded restricted upgrading and 4 mm disclosed modest benefit. The right and left eyes in the 3 mm group demonstrated statistically significant reductions in LogMAR scores (p < 0.001). Difficulties were slight, with only a few cases of transient IOP elevation (2.5%) and IOL pitting (1.2%).
Table 1: Baseline Demographic, Clinical, and Cataract Characteristics of Participants (N=81)
|
Characteristic |
Frequency (n) |
Percentage (%) |
|
Age (years) |
||
|
20-40 |
3 |
3.7 |
|
41-60 |
28 |
34.6 |
|
61-80 |
50 |
61.7 |
|
Mean ± SD |
60.91 ± 12.21 |
|
|
Median (Range) |
64 (21-78) |
|
|
Gender |
||
|
Male |
38 |
46.9 |
|
Female |
43 |
53.1 |
|
Occupation |
||
|
Business |
9 |
11.1 |
|
Housewife |
37 |
45.7 |
|
Banker |
6 |
7.4 |
|
Maid |
4 |
4.9 |
|
Others |
16 |
19.8 |
|
Student |
3 |
3.7 |
|
Teacher |
6 |
7.4 |
|
Religion |
||
|
Islam |
74 |
91.4 |
|
Hindu |
7 |
8.6 |
|
Presenting Complaints |
||
|
Difficulty of vision in affected eye |
77 |
95.1 |
|
Watering |
7 |
8.6 |
|
Blurring of vision |
4 |
4.9 |
|
Foreign body sensation |
4 |
4.9 |
|
Eye ache or discomfort in the eye |
3 |
3.7 |
|
Itching |
3 |
3.7 |
|
Cataract Affected Eye |
||
|
Right |
27 |
33.3 |
|
Left |
24 |
29.6 |
|
Both |
30 |
37 |
|
Type of Cataract |
||
|
Age-Related Cataract (ARC) |
75 |
92.6 |
|
Developmental |
3 |
3.7 |
|
Presenile Cataract |
3 |
3.7 |
|
Type of Cataract Extraction |
||
|
Small Incision Cataract Surgery (SICS) |
46 |
56.8 |
|
Phacoemulsification |
34 |
42 |
|
Extracapsular Cataract Extraction (ECCE) |
1 |
1.2 |
|
Type of IOL Implant |
||
|
Polymethyl methacrylate (PMMA) |
46 |
56.8 |
|
Foldable |
35 |
43.2 |
|
Comorbidities |
||
|
Diabetes Mellitus |
34 |
42 |
|
Hypertension |
31 |
38.3 |
|
Chronic Kidney Disease |
3 |
3.7 |
|
Hearing problem |
3 |
3.7 |
Multiple responses were allowed for presenting complaints.
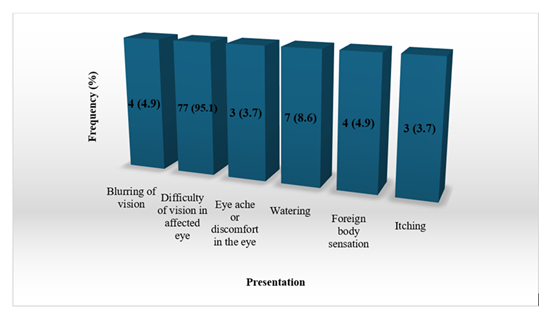
Table 1 shows that the majority of the 81 participants were aged 61-80 years 61.7%, with a mean age of 60.91 ± 12.21 years, and more than half were female 53.1%. Most were housewives 45.7% and followed Islam 91.4%. The predominant donating complaint was difficult seeing in the affected eye 95.1%, while watering, blurring, and eye discomfort were less common. Cataracts affected both eyes in 37% of cases, and ARC was the most frequent type 92.6%. SICS was the most performed procedure 56.8%, and PMMA lenses were implanted in over half the cases. Common comorbidities diabetes 42% and hypertension 38.3%.
Figure 1 shows difficulty in vision of the affected eye 95.1% was the chief complaint of the participants, followed by watering 8.6%, blurring of vision 4.9%, and foreign body sensation 4.9%.
Table 2: Characteristics of Posterior Capsule Opacification and Nd:YAG Laser Application
|
Variable |
Values |
|
Type of Posterior Capsule Opacification |
|
|
Elschnig's Pearl |
34 (42.0%) |
|
Fibrosis |
34 (42.0%) |
|
Wrinkling |
10 (12.3%) |
|
Dense PCO |
3 (3.7%) |
|
Duration of PCO development after PCIOL implant (months) |
|
|
Mean ± SD |
59.22 ± 54.60 |
|
Median (Range) |
36.0 (4-240) |
|
Number of Eyes Undergone YAG Laser |
|
|
Right |
30 (37.0%) |
|
Left |
30 (37.0%) |
|
Both |
21 (25.9%) |
|
YAG Laser Energy Level per Pulse (mJ) |
|
|
Mean ± SD |
2.80 ± 0.43 |
|
Median (Range) |
2.70 (2.20-4.10) |
|
Total Number of YAG Laser Burns |
|
|
Right eye: Mean ± SD |
37.76 ± 18.06 |
|
Right eye: Median (Range) |
34.0 (20-114) |
|
Left eye: Mean ± SD |
66.18 ± 76.50 |
|
Left eye: Median (Range) |
40 (14-350) |
|
Total Energy Used (mJ) |
|
|
Right eye: Mean ± SD |
103.58 ± 58.07 |
|
Right eye: Median (Range) |
96 (46-319) |
|
Left eye: Mean ± SD |
216.61 ± 320.69 |
|
Left eye: Median (Range) |
100 (50-1435) |
|
Size of YAG Laser Capsulotomy |
|
|
Small |
3 (3.7%) |
|
Medium |
59 (72.8%) |
|
Large |
19 (23.5%) |
Table 2 presents that the Elschnig’s Pearl and fibrosis, each accounting for 42% of cases, followed by wrinkling 12.3% and dense PCO 3.7%. The mean duration for PCO development after PCIOL implantation was approximately 59.2 months. Nd:YAG laser capsulotomy was performed on the right and left eyes equally 37% each, while 25.9% had bilateral procedures. The mean energy level per pulse was 2.80 ± 0.43 mJ. The mean number of laser burns and total energy used were higher in the left eye (66.18 burns, 216.61 mJ) compared to the right eye (37.76 burns, 103.58 mJ). Most capsulotomies were of medium size 72.8%, with fewer small 3.7% and large 23.5% openings.
Table 3: LogMAR Visual Acuity Changes Following Nd:YAG Laser Posterior Capsulotomy at Different Follow-up Periods
|
Eye |
Statistical Measure |
Pre-treatment Visual Assessment (LogMAR) |
Post-treatment Visual Assessment (LogMAR) |
P-value |
|
|
|
|
7 Days |
|
|
Right |
Mean ± SD |
0.88 ± 0.23 |
0.21 ± 0.10 |
<0.001 |
|
Median (Range) |
1.0 (0.6-1.3) |
0.18 (0.0-0.30) |
||
|
Left |
Mean ± SD |
0.77 ± 0.25 |
0.19 ± 0.09 |
<0.001 |
|
Median (Range) |
0.60 (0.60-1.3) |
0.18 (0.0-0.30) |
||
|
|
|
|
1 Month |
|
|
Right |
Mean ± SD |
0.88 ± 0.23 |
0.20 ± 0.101 |
<0.001 |
|
Median (Range) |
1.0 (0.6-1.3) |
0.18 (0.0-0.30) |
||
|
Left |
Mean ± SD |
0.77 ± 0.25 |
0.1886 ± 0.095 |
<0.001 |
|
Median (Range) |
0.60 (0.60-1.3) |
0.18 (0.0-0.30) |
||
|
|
|
|
6 Months |
|
|
Right |
Mean ± SD |
0.88 ± 0.23 |
0.2025 ± 0.0966 |
<0.001 |
|
Median (Range) |
1.0 (0.6-1.3) |
0.18 (0.0-0.30) |
||
|
Left |
Mean ± SD |
0.77 ± 0.25 |
0.1875 ± 0.0890 |
<0.001 |
|
Median (Range) |
0.60 (0.60-1.3) |
0.18 (0.0-0.30) |
P-values calculated using the Wilcoxon signed-rank test.
Table 3 shows significant improvement in visual acuity following Nd:YAG laser posterior capsulotomy. In both right and left eyes, the mean LogMAR visual acuity markedly improved from baseline at all follow-up periods -7 days, 1 month, and 6 months post-treatment with p-values <0.001 in all comparisons. For the right eye, the mean LogMAR score decreased from 0.88 pre-treatment to approximately 0.20 at all follow-ups. Similarly, the left eye showed improvement from 0.77 pre-treatment to about 0.19 post-treatment. The median values consistently dropped to 0.18, indicating a stable and sustained visual gain over time.
Table 4: The difference of Pre - treatment and post-treatment LogMAR visual acuity at one and six month following (Nd: YAG Laser Posterior Capsulotomy) periods according to the size of the capsulotomy
N/A: Data did not receive for left eye
Wilcoxon signed-rank test
Table 4 reveals that patients who underwent 3 mm and 4 mm Nd:YAG capsulotomy showed statistically significant improvements in visual acuity at both one-month and six-month follow-ups (p<0.001 for 3 mm; p=0.008 for 4 mm in right eyes, and p=0.001 for left eyes with 4 mm openings). Specifically, mean LogMAR values improved from 0.78 to 0.19 in 3 mm right eyes and from 1.0 to 0.41 in 4 mm left eyes. However, no statistically significant improvement was observed for the 2 mm group (p=0.083), likely due to the small sample size. No data has been collected for 2mm left eyes. These results suggest that medium- and large-sized capsulotomies (≥3 mm) are more effective in improving visual acuity post-treatment.
Figure 2 shows that complications following Nd:YAG laser posterior capsulotomy were minimal. Transient elevation in IOP was observed in 2 patients 2.46%, while pitting or cracking of the IOL occurred in only 1 patient 1.23%.
Discussion
The existing prospective study aimed to evaluate the long-term effect of Nd:YAG laser posterior capsulotomy on visual acuity and to investigate the relationship between capsulotomy size and visual outcomes, while also observing associated complications. Our findings reveal a significant and sustained development in visual acuity over a six-month period resulting Nd:YAG laser posterior capsulotomy. This practical upgrading is consistent with prior research that has stated a significant visual benefit after the procedure, attributable to the effective permission of posterior capsule opacification [5, 6, 21, 22, 23]. The sustained visual gains noted at 7 days, 1 month, and 6 months post-treatment focus the lasting efficacy of Nd:YAG laser capsulotomy in restoring vision cooperated by PCO. A key aspect of this study was the examination of visual outcomes in relation to capsulotomy size. Our results signify that a 3 mm capsulotomy size yielded the most consistent and statistically significant visual gains in both right and left eyes (p < 0.001). This recommends an optimal balance between making an satisfactory optical opening and minimizing collateral effects. The 2 mm capsulotomy, however, showed limited development that was not statistically significant (p = 0.083), likely due to a smaller sample size for this group and possibly an insufficient opening to effectively improve symptoms caused by PCO, which is consistent with some literature signifying larger openings for optimal visual function [15]. Equally, the 4 mm capsulotomy size displayed modest, statistically significant benefits (p = 0.008 for right eyes, p = 0.001 for left eyes). While greater openings may offer a wider optical zone, previous studies have debated the optimal diameter, with some signifying that unduly large capsulotomies might not forever confer extra visual benefits and could possibly rise the risk of glare or other aberrations [7, 8, 10, 14]. Our findings, therefore, support the concept that medium-sized capsulotomies, mostly 3 mm, are most effective in attaining significant visual acuity improvement. The safety profile of Nd:YAG laser posterior capsulotomy in our cohort was outstanding, with nominal complications detected. Transient intraocular pressure elevation happened in only 2.5% of patients, and intraocular lens pitting was noted in 1.2%. These low rates of adverse events are reassuring and align with the consensus on the safety of Nd:YAG laser capsulotomy, as stated in various studies [11, 17, 23]. The absence of more severe problems, such as cystoid macular edema or retinal detachment, which are occasionally associated with Nd:YAG capsulotomy [12, 13] more underlines the procedure's safety when achieved with suitable parameters. The mean energy level per pulse (2.80 ± 0.43 mJ) and the total number of laser burns were within satisfactory ranges, reflecting a careful method to laser application, which is critical for minimizing difficulties like IOL damage or IOP spikes [17, 18]. Concerning the characteristics of PCO, Elschnig's Pearl and fibrosis were similarly prevalent (42% each), steady with the diverse morphological presentations of PCO [1]. The mean duration of PCO growth after PCIOL implantation was about 59.2 months, highlighting the late onset of this common postoperative complication [2]. The higher mean number of lasers burns, and total energy used in the left eyes associated to the right eyes proposes separately variability in PCO density and morphology, requiring tailored treatment methods [20].
Conclusions
This prospective study authorizes that Nd:YAG laser posterior capsulotomy is an extremely effective and safe procedure, important to significant and sustained visual acuity improvement over six months. The 3 mm capsulotomy size established superior and consistent visual gains, signifying it as an optimal target for attaining best outcomes. With a remarkably low frequency of transient difficulties, the procedure remains a vital intervention for handling posterior capsule opacification.
Authors Contributions
Dr. Md Golam Faruk Hossain conceptualized the study and designed the methodology. Dr. Md Miftahul Hossain Chowdhury and Dr. Mazharul Hoque Bhuiyan contributed data management and statistical analysis. Dr. Mohammad Mazaharul Islam assisted in manuscript drafting and critical revisions. Dr. Md Shaiful Islam and Md Golam Faruk Hossain supervised the research and provided final manuscript approval. All authors reviewed and approved the final version.
Declaration of Interest
The authors declare no competing financial interests.
Conflict of Interest: The authors declare no conflicts of interest related to this study.
References
- Apple DJ, Peng Q, Visessook N, et al. Posterior capsule opacification. Surv Ophthalmol 59 (2014): 111–32.
- Mamalis N, Brick R, Davis MS. Incidence of posterior capsule opacification after cataract surgery. Am J Ophthalmol 162 (2016): 61–8.
- Liu Y, Chang P, Lu Y. PCO: A persistent issue in modern cataract surgery. Eye (Lond) 34 (2020): 201–10.
- Pandey SK, Werner L. Nd:YAG laser capsulotomy: indications and outcomes. J Cataract Refract Surg 44 (2018): 371–8.
- Acar BT, Acar S. Visual outcomes after Nd:YAG capsulotomy at one and six months. Eur J Ophthalmol 29 (2019): 528–35.
- Liu C, Xu M, Song H. Efficacy of Nd:YAG laser in PCO. J Refract Surg 37 (2021): 124–30.
- Shah SM, Hodge C. Capsulotomy size and glare disability. Br J Ophthalmol 106 (2022): 499–505.
- Kim HJ, Lee SY. Optimal diameter in Nd:YAG capsulotomy: clinical trial. Int Ophthalmol 39 (2019): 2451–8.
- Tseng VL, Yu F. Capsulotomy size and posterior segment complications. Ophthalmic Surg Lasers Imaging Retina 51 (2020): 346–52.
- Packard R, Nguyen P. Visual benefit vs risk in capsulotomy size. Cornea 37 (2018): 350–6.
- Olson RJ, Shah M. Managing IOP spikes after Nd:YAG capsulotomy. J Clin Aesthet Dermatol 12 (2019): E68–71.
- Vasavada AR, Singh R. Capsulotomy size and macular edema incidence. J Cataract Refract Surg 44 (2018): 356–61.
- Bjerregaard A, Robson AG. Capsulotomy diameter and retinal detachment risk. Eye (Lond) 36 (2022): 1998–2005.
- Chen HC, Chang YC. Discrepancies in capsulotomy outcomes by size. Ophthalmic Res 58 (2017): 82–90.
- Patel DV, Kalyani P. Small versus large capsulotomy: systematic review. Ophthalmol Ther 9 (2020): 353–65.
- Nguyen PD, Morales E. Capsulotomy size and glare: meta-analysis. BMC Ophthalmol 23 (2023): 15.
- Holland SP, Shugar JK. Laser energy and IOP fluctuations. J Cataract Refract Surg 44 (2018): 1242–8.
- Kumar M, Venkatesh R. Energy settings and IOL integrity. J Refract Surg 37 (2021): 508–16.
- Cionni RJ, Osher RH. Advances in laser delivery systems. J Cataract Refract Surg 49 (2023): e1-8.
- Das AV, Kumar A. Algorithms to optimize capsulotomy size and energy. Ophthalmology 127 (2020): 459–66.
- Hwang B, Nam S. Long-term visual outcomes after Nd:YAG capsulotomy. Asia Pac J Ophthalmol 8 (2019): 380–6.
- O’Boyle C, Shafi M. Visual acuity at 6 months post-capsulotomy. Clin Ophthalmol 16 (2022): 1839–47.
- Patel HT, Trivedi R. Six-month efficacy and safety of Nd:YAG capsulotomy. Ophthalmic Surg Lasers Imaging Retina 55 (2024): 49–56.
Article Views: 952
Journal Statistics




Discover More: Recent Articles
Grant Support Articles
- Explicating the Role of miR-638 in the Pathogenesis of Exfoliation Syndrome and Exfoliation Glaucoma
- Contributing Factors to The Awareness of Health Risks of Geophagy Among Pregnant Women in Lubumbashi
- Support of Patients Admitted with COVID-19 at Public Hospitals in South Africa by the Family Members
- View More
© 2016-2026, Copyrights Fortune Journals. All Rights Reserved!