Cardiothoracic Surgery Training: An Honest and Anonymous Assessment of the Trainee Experience
Fatima G Wilder, MD MSc1*, Jason Han, MD2, William G Cohen BA2, Clauden Louis MD MS3, J Hunter Mehaffey MD MSc4, Alexander Brescia MD5, David Blitzer, MD6, Jessica GY Luc MD7, Garrett Coyan MD8, Jordan P. Bloom MD, MPH9, Marisa Cevasco MD2, Ahmet Kilic MD1
1Division of Thoracic Surgery, Brigham and Women’s Hospital, Boston, MA, USA
2Division of Cardiothoracic Surgery, University of Pennsylvania, Philadelphia, PA, USA
3Department of Cardiothoracic Surgery, University of Rochester, Rochester, NY, USA
4Division of Thoracic and Cardiovascular Surgery, University of Virginia, Charlottesville, VA, USA
5Department of Surgery, University of Michigan, Ann Arbor, MI, USA
6Department of Surgery, Columbia University, New York, NY, USA
7Division of Cardiovascular Surgery, University of British Columbia, Vancouver, BC, USA
8Department of Cardiothoracic Surgery, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
9Division of Cardiac Surgery, Massachusetts General Hospital, Boston, MA, USA
*Corresponding Author: Fatima G Wilder, Division of Thoracic Surgery, Brigham and Women’s Hospital, Boston, MA, USA
Received: 15 December 2022; Accepted: 22 December 2022; Published: 27 January 2023
Article Information
Citation: Fatima G Wilder, Jason Han, William G Cohen, Clauden Louis, J Hunter Mehaffey, Alexander Brescia, David Blitzer, Jessica GY Luc, Garrett Coyan, Jordan P. Bloom, MPH, Marisa Cevasco, Ahmet Kilic. Cardiothoracic Surgery Training: An Honest and Anonymous Assessment of the Trainee Experience. Journal of Surgery and Research 6 (2023): 13-21.
View / Download Pdf Share at FacebookAbstract
Objective(s): Trainee assessments aim to identify areas for improvement and address problems within training programs. However, effectiveness is limited by an inability to assess programs anonymously. We hypothesized concern for undesired repercussions may discourage honest responses. To test this, we conducted a comprehensive survey of trainees to assess their educational and work-related experiences anonymously.
Design: A 51-question survey was distributed electronically to the Thoracic Surgery Residents Association (TSRA) membership. Questions were multiple-choice. The Likert scale was utilized.
Setting: The survey was accessed electronically and was completed by participants nationwide.
Participants: Trainees were incentivized to complete the survey with the opportunity to receive a $50 gift card or TSRA textbook. 109 of 551 cardiothoracic surgery trainees completed the survey.
Results: 109 trainees (109/551, 19.8%) completed the survey. 57.8% of respondents reported complying with work hour restrictions, but 32.2% (n=35) did not feel comfortable reporting violations honestly. The majority of respondents agreed or strongly agreed that their program was preparing them to independently perform low risk cardiac (4.19 [1.22]) and thoracic (4.08 [1.13]) cases independently, 30.3% of chief residents reported planning to pursue additional training. 66% of respondents stated they would select the same program again. 33% reported having high morale, 47.7% moderate and 19.3% poor or declining morale. 84.4% of respondents did not feel their race or gender significantly impacted their training, 26.6% reported systemic bias in recruitment of new trainees or faculty, and 38.5% believed there was inadequate diversity a
Keywords
<p>Cardiothoracic surgery trainees, ACGME, Surveys, Training experience</p>
Article Details
Introduction
In the field of cardiothoracic (CT) surgery, training experiences can vary widely across the country, so regulatory mechanisms are especially important in enforcing guidelines and standards to promote a safe, fair and equitable training experience. Establishing and enforcing these guidelines is partly reliant on the feedback that is obtained from the trainees that are affected by them. The Accreditation Council for Graduate Medical Education (ACGME) is the national regulatory body responsible for accrediting residency and fellowship programs across the United States. Through annual surveys, they are provided with information that allows them to evaluate the well-being and needs of trainees and faculty. The current mechanism of the survey is anonymous to the individual, but it is not anonymous regarding the program. One question that arises based on the current system is, how might the responses of trainees vary when the surveys they complete are anonymous? It is our suspicion that anonymity may better capture the real experience of trainees.
Participants and Methods
This cross-sectional survey study was determined to be exempt research by the Johns Hopkins Medicine Institutional Review Board (IRB00267786). Consent was obtained from each participant at the start of each survey. The identities and institutions of each respondent were not collected and anonymity was maintained.
Survey
A 51 question self-report survey was created using Google Forms (Mountain View, CA) to assess respondent’s perspectives on the following aspects of their training programs: demographics, operative experience, work hours, work environment, diversity and inclusion, trainee morale, and overall quality. Questions were multiple choice, with the Likert scale (1=strongly disagree and 5=strongly agree) being utilized for applicable questions. One question allowed additional free response. The survey was reviewed by the Thoracic Surgery Directors Association (TSDA) and Thoracic Surgery Residents Association (TSRA).
Distribution
The TSRA is a national organization for all cardiothoracic surgery trainees representing the three accredited training pathways: Integrated (6 year), hybrid (4+3 year), and traditional (2-3 year). The survey was distributed electronically via newsletter to all members of the TSRA between April and June, 2021. In 2021, there were 551 total CT surgery residents and congenital fellows. The survey closed after 3 months of open completion. Incentives included the opportunity to receive a $50 gift card or a TSRA textbook.
Analysis
Responses were downloaded and reviewed. Duplicate responses were removed. Normality of data was assessed using the Shapiro-Wilk test. Data are presented as n (%), mean (SD), or median [IQR] as appropriate. Data analysis was conducted using Stata 16 (StataCorp, College Station, TX).
Results
Demographics
A total of 109 surveys were completed with the majority of respondents being male [67.9% [n=74] vs 32.1% [n=35]). The majority of participants identified as White (71.6%, n=78), with the remainder being Asian (19.2%, n=21), Black/African American (5.5%, n=6), and Other (0.9%, n=1). Three participants (2.8%) preferred not to identify their race/ethnicity. The post-graduate year (PGY) distribution was equally distributed between years 1-9. [Table 1].
The majority of trainees were in integrated (I-6) programs (n=60, 55.1%), followed by traditional programs (n=40 36.7%), and 4+3 programs (n=8, 7.3%). The majority of participants (n=58, 53.2%) anticipated pursuing a career in adult cardiac surgery while 24% (n=24) planned to pursue thoracic surgery, 14.7% (n=16) congenital, and 9.2% (n=10) a hybrid practice. The anticipated practice type was most commonly academic [69.7% (n=76)].
|
Demographics |
n (%) |
|
Gender |
|
|
Male |
74 (67.9%) |
|
Female |
35 (32.1%) |
|
Race/Ethnicity |
|
|
Asian |
21 (19.2%) |
|
Black/African American |
6 (5.5%) |
|
White |
78 (71.6%) |
|
Other |
1 (0.9%) |
|
Prefer not to say |
3 (2.8%) |
|
Current PGY year (including research) |
|
|
PGY 1 |
12 (11.0%) |
|
PGY 2 |
12 (11.0%) |
|
PGY 3 |
7 (6.4%) |
|
PGY 4 |
11 (10.1%) |
|
PGY 5 |
9 (8.3%) |
|
PGY 6 |
17 (15.6%) |
|
PGY 7 |
12 (11.0%) |
|
PGY 8 |
16 (14.7%) |
|
PGY 9 |
10 (9.2%) |
|
PGY >9 |
3 (2.8%) |
|
Program Type |
|
|
I-6 |
60 (55.1%) |
|
4+3 |
8 (7.3%) |
|
Traditional |
40 (36.7%) |
|
Other |
1 (0.9%) |
|
Anticipated Career Plans |
|
|
Cardiac |
58 (53.2%) |
|
Thoracic |
24 (22.0%) |
|
Congenital |
16 (14.7%) |
|
Hybrid |
10 (9.2%) |
|
Undecided |
1(0.9%) |
|
Anticipated Practice Setting |
|
|
Academic |
76 (69.7%) |
|
Private |
10 (9.2%) |
|
Academic Affilitated |
22 (20.2%) |
|
Other |
1 (0.9%) |
Table 1: Demographics and anticipating practice plans
Operative experience
Participants’ operative experiences were generally positive. The majority strongly agreed with the statement that their program provides adequate supervision in the operating room (5 [4-5]), and that their program provides an adequate variety of cases (4.4, SD 0.96). Most did not feel they had to compete for cases (2 [1-3]) [Figure 1].
On the topic of autonomy, responses trended toward agreement with the statement that their program gives significant autonomy to their senior residents or fellows in the cardiovascular intensive care unit (ICU) (4 [3-5]). For trainees that are part of an integrated program, the majority reported feeling accepted as part of the team (4 [3-5]) during their general surgery rotations. Similarly, the majority reported that they are given opportunities similar to general surgery residents while on those rotations (5 [4-5]) [Figure 1].
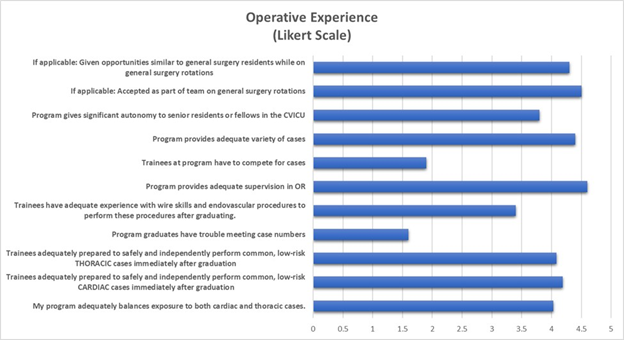
Figure 1: Operative Experience and Trainee Preparedness
Trainees agreed with the statement “My program adequately balances exposure to both cardiac and thoracic cases” (4 [3-5]), and “My program adequately prepares trainees to safely and independently perform common, low-risk cardiac cases (e.g., CABG, AVR) immediately after graduation” (4 [4-5]). The majority of trainees reported routinely performing >50% of common, low-risk cardiac cases autonomously at the senior or chief integrated resident level or after 1st year of traditional fellowship (73.4% (n=80). Interestingly, 10.1% (n=11) reported never being able to perform >50% of common, low-risk cardiac cases autonomously throughout their training. Of these, n=5 were from an I-6 program, n=5 traditional and n=1 a hybrid program [Table 2].
Regarding thoracic surgery, trainees generally agreed with the statement “My program adequately prepares trainees to safely and independently perform common, low-risk thoracic cases (e.g., Lobectomy, etc.) immediately after graduation.” (4 [3-5]). When compared to cardiac cases, a greater number of respondents felt ready to perform >50% of common, low-risk thoracic cases autonomously (i.e. lobectomy, wedge resection, VATS procedures) as a junior integrated resident (PGY 1-3) or during 1st year of traditional fellowship (26.6% (n=29)). However, the majority of fellows (59.6%, n=65) reported being ready as a senior or chief integrated resident or after 1st year of traditional fellowship. Interestingly, 11.9% (n=13) reported never feeling ready to perform >50% of common low-risk thoracic cases autonomously. Of these, n=10 were in an I-6 program and the remainder (n=3) were in a traditional program.
The majority of respondents strongly disagreed with the statement “Program graduates have trouble meeting case numbers” with a mean Likert response of (1 [1-2]). Responses were less affirmative regarding the statement, “Program trainees have adequate experience with wire skills and endovascular procedures (e.g., TAVR, TEVAR) to perform these procedures after graduating” (4 [2-4]), and not all trainees (86.2%) reported having access to robotic surgery training if interested.
Nearly a third of participants (30.3%, n=33) planned to pursue additional training after residency/fellowship while another third (28.4%, n=31) were undecided. The most common reason cited for pursuing additional training was desiring a “niche area of practice” (21.1%, n=23) [Table 2]
|
OPERATIVE EXPERIENCE |
N (%) |
|
At what stage do trainees routinely perform >50% of common, low-risk CARDIAC cases autonomously? |
|
|
Junior Integrated resident (PGY 1-3) or 1st year of traditional fellowship |
16 (14.7%) |
|
Senior or Chief Integrated Resident or after 1st year of traditional fellowship |
80 (73.4%) |
|
Superfellow |
2 (1.8%) |
|
Never |
11 (10.1%) |
|
At what level do trainees perform >50% of common, low risk THORACIC cases autonomously (i.e. lobectomy, wedge resection, VATS procedures)? |
|
|
Junior Integrated resident (PGY 1-3) or 1st year of traditional fellowship |
29 (26.6%) |
|
Senior or Chief Integrated Resident or after 1st year of traditional fellowship |
65 (59.6%) |
|
Superfellow |
1 (0.9%) |
|
Never |
14 (12.8%) |
|
Trainees have access to robotic surgery training if interested |
94 (86.2%) |
|
Planning to pursue additional training after residency/fellowship |
|
|
Yes |
33 (30.3%) |
|
No |
45 (41.3%) |
|
Undecided |
31 (28.4%) |
|
If planning to pursue additional training, why? |
|
|
No additional training planned |
43 (39.5%) |
|
Niche area of practice |
23 (21.1%) |
|
Additional training required for interest |
21 (19.3%) |
|
Networking and mentorship |
9 (8.3%) |
|
Don't feel prepared for practice |
6 (5.5%) |
|
Job market concerns |
5 (4.6%) |
|
Undecided on additional training |
2 (1.8%) |
|
Program has elective time for extra sub-specialty interests |
71 (65.1%) |
Table 2: Operative experience and future plans
Work Hours
The majority of respondents report adherence to work hour restrictions [Figure 2]. When asked about the 80-hour work week, 75.2% of trainees reported compliance “always”, “almost always” or “>50% of the time”. When asked about having on average 1 day off a week (or an average of 4 days total off from clinical duties over a 28 day period), greater than 89% of respondents reported compliance “always”, “almost always” or “>50% of the time”. Despite such high compliance, when given the statement “I am comfortable reporting work hour violations honestly”, the mean Likert score was neutral 4 [2-5] with only a minority 34/109 (31.2%) stating “Strongly agree”.
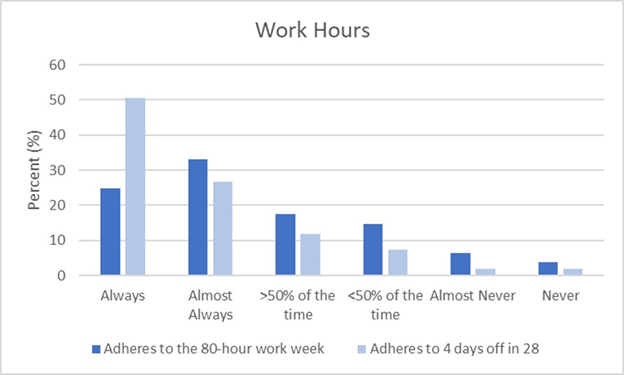
Figure 2: Trainee Adherence to Work Hour Restrictions
Education and Work Environment
The majority of respondents 73.4% (n=80) agreed that education outside of the operating room (OR) is either a high priority or somewhat of a priority at their program. Attending involvement with didactics, board preparation, and opportunities for research, and leadership development were generally positive (Figure 3). Most felt adequately prepared for their boards (4 [3-5]), that their programs are receptive to feedback (4 [3-5]), and agreed that their program directors were invested in their training and professional well-being (4 [4-5]). Yet, surprisingly, only about half (52.3%, n=57) of respondents had a designated mentor.
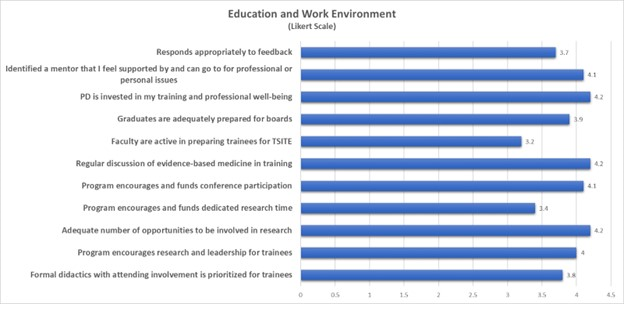
Figure 3: Trainee Opinions on Education and Work Environment
Diversity and Inclusion
While most trainees felt their race/ethnicity has no impact on their training (70.6%, n=77), 8.3% (n=9) of respondents felt that there was a negative impact. Slightly more than half (61.5%, (n=59)) of respondents felt there is adequate diversity among faculty and trainees at their institution. 26.6% (n=25) respondents perceive systematic bias in the recruitment of new trainees or faculty at their program. 67.9% (n=74) respondents feel that their gender has no impact on their training. Of these, 70.3% were male. 11 trainees reported that their gender has a positive impact on their training and 9 reporting a negative impact of their gender on their training [Table 3]. Of those reporting a negative impact, n=7 were female and n=2 were male. Of those reporting a positive impact, n=1 was female and n=10 were male [Table 3].
Notably, 30.3% (n=33) of respondents reported verbal or physical harassment by an attending and or senior resident/fellow (14.7%, n=16). The majority of respondents (74.3%, n=81) reported that their institution has a method of safe reporting of harassment or other issues [Table 3].
|
Diversity and Inclusion |
n(%) |
|
Impact of your gender on your training |
|
|
No answer |
15 (13.8%) |
|
No Impact |
74 (67.9%) |
|
Positive Impact |
11 (10.1%) |
|
Negative Impact |
9 (8.3%) |
|
Impact of your race/ethnicity on your training |
|
|
No answer |
15 (13.8%) |
|
No Impact |
77 (70.6%) |
|
Positive Impact |
8 (7.3%) |
|
Negative Impact |
9 (8.3%) |
|
Adequate diversity among faculty and trainees at your program |
59 (61.5%) |
|
Systematic bias in recruitment of new trainees or faculty at your program |
25 (26.6%) |
|
Verbally or physically harassed by an attending at your program |
33 (30.3%) |
|
Verbally or physically harassed by a senior resident or fellow at your program |
16 (14.7%) |
|
Institution has method of safe reporting of harassment or other issues |
|
|
Yes |
81 (74.3%) |
|
No |
5 (4.6%) |
|
Unsure |
23 (21.1%) |
Table 3: Trainee experiences surrounding diversity, inclusion and harassment
Overall Opinion and Morale
In assessing overall opinion of their program, slightly more than half of residents (66%, n=72) would pick the same program again [Figure 4]. When asked why “No” or “Unsure” the most cited reason was training quality (n=7) [Table 4]. The mean score was a 4 [3-5] in response to the statement “I would recommend my program to future trainees”. Morale was high among a minority of participants (33%, n=36) and moderate among the majority (47.7%, n=52). 8.3% (n=9) said morale was poor and declining (11%, n=12) .
|
Opinion/Morale (If no or unsure, why? (mentions, FRQ)) |
N |
|
Training Quality |
7 |
|
Faculty |
6 |
|
Changes since starting or mislead |
6 |
|
Non Training Reason |
3 |
|
Culture |
2 |
|
Research/Mentorship |
2 |
|
Change type of program |
1 |
Table 4: Reasons why trainees reported “No” or “Unsure” when asked if they would pick the same program again.
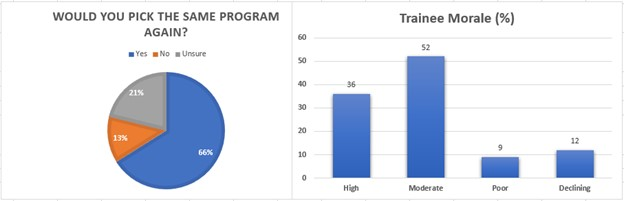
Figure 4: Trainee Thoughts on Programs and Overall Morale
Discussion
Honest assessment of CT surgery trainee experiences in the United States is a complicated process. The annual residency surveys currently utilized are a significant component of the certification process. Areas that are assessed within the survey include: Clinical Experience and Education, Faculty Teaching and Supervision, Evaluation, Educational Content, Diversity and Inclusion, Resources, Patient Safety/Teamwork, Professionalism and Overall Evaluation of the program. All accredited programs are expected to participate in the survey with a required completion rate of 70%. Program accreditation relies heavily on the responses to these surveys as they are used to provide early warning of areas in which the program may be non-compliant with ACGME requirements. When warning areas are identified, the ACGME charges the program director with demonstrating methods through which they will rectify any issues that may have been identified [1]. While this method is well-structured, there is concern about the reliability of results obtained via this method due to non-anonymity and fear of repercussions to participants.
The survey discussed here was created with the intention of assessing the responses provided when trainees are given an opportunity to give feedback anonymously without fear of negative consequences. Importantly, the results of the survey highlight a general sense of satisfaction amongst current trainees in cardiothoracic surgery that completed the survey. The majority feel prepared to go into practice by the completion of their training. For those pursuing more training, the primary reason is the desire for a niche area of practice, as opposed to lack of preparation. There is a general sense of support for conference attendance, adequate research opportunities, and adequate in-service exam preparation. Most feel their education is supported and prioritized by faculty. All these responses provide reassurance that most of the programs represented by survey respondents are meeting the expected thresholds in the areas of Clinical Experience, Education, Faculty Teaching, Resources, Teamwork and Educational Content.
Although the general feedback obtained from the survey was positive, there were several responses that raise concern. The first of these is duty hour adherence. 57.8% reported that their program adheres to the 80-hour work week and get at least 4 days off in a 28-day period. However, when asked about comfort reporting work hours honestly, 12.8% (n=14) respondents selected disagree and 19.2% (n=21) selected strongly disagree. If greater than 30% of survey respondents do not feel comfortable reporting work hour violations honestly, one would suspect that when completing the annual survey, the answers provided are not accurate. As a result, the data gathered from those results may not in fact be representative of the true trainee experience.
Another important finding of this survey is regarding inclusion and diversity. The results of this survey suggest that there is a perceived sense of recruitment bias amongst not only trainees, but faculty as well. Concerns around the topics of gender and diversity have been highlighted in other settings both at the trainee and the faculty level. In a publication looking at trends in integrated CT surgery programs, Powell et al2 found that amongst trainees in integrated CT surgery programs, there were 26.2% that identified as Asian, 5.3% as Hispanic and 2.2% as African-American. 66.4% were caucasian. When time trend analyses were used, they did not find any improvements in gender diversity or representation of African Americans and Hispanic residents in integrated cardiothoracic programs over the 14-year time-period that was reviewed. This suggests that despite efforts that programs may be making to increase diversity, the trainee pool is not becoming more diverse.
When one extends this look to the faculty level, the numbers are not much more encouraging according to the available data. Although Blacks/African Americans and Hispanics compose 13.4% and 18.3%, respectively, of the U.S. population according to the 2018 Census data3, these groups only comprised 5% and 5.8% of all practicing physicians in the same year4. Along similar lines, in 2018 although 50.8% of the U.S. population was female, only 35.8% of practicing physicians identified as female5. Ortmeyer et al6 assessed the racial/ethnic and gender diversity in the field of CT surgery as compared to other surgical subspecialties and medicine overall in the year 2018. They found that 17% of CT surgery faculty were female (compared to 27% of surgical faculty (p<0.01)). Black/African American faculty comprised 3% and Hispanic comprised 5% of CT surgery faculty which was similar to surgical faculty. 24% of CT surgery trainees were women, compared to 36% of surgical trainees (p<0.01). 4% of residents were Black/African American and 5% were Hispanic. These findings suggest a notable discrepancy between reality versus the expectation of diversity in our programs.
The fact that trainees are identifying this issue creates concern in that it may not only affect morale, but it may also limit the option for trainees to select mentors from a diverse pool of faculty. Additionally, this may impact recruitment of a broader pool of trainees that will eventually swing the pendulum to a more diverse workforce. If we are unable to improve the diversity at the faculty level, the challenge of recruiting medical students who will eventually grow into a diverse workforce, may continue to be an uphill battle.
A somewhat alarming finding of this survey was the report of verbal or physical harassment by a senior resident, fellow or attending. 30.3% of respondents endorsed harassment by an attending at their program and 14.7% harassment by a senior resident or fellow. The culture of surgery has progressed significantly from the anecdotal days of surgeons with “bad behavior” that goes unchecked in and out of the operating room. There should be no place for verbal or physical harassment by ones’ colleagues at any level. An important take-away from these findings would be the need for programs to invite trainees to discuss episodes of harassment in a safe, non-retaliatory environment. This should include the individual experiencing the harassment as well as those that may observe it.
Finally, it is important to note the report of poor/declining morale in 19% of participants. The culture of “suck it up” is still prevalent in the CT surgery environment. This has proven detrimental in surveys assessing well-being7. A systematic review and meta-analysis evaluating over 17,000 physicians in training identified that 20.9-43.2% of trainees screened positive for depression or depressive symptoms. The effects of this poor state of mental health include lower-quality patient care and increased risk for future depression amongst physicians. The need to identify and address this early on is paramount.
A limitation of this survey is that it may be more beneficial to separate the responses of this survey by program-type. As suggested by Lebastchi and Yuh8, trainees in I-6 programs expressed significant overall satisfaction with their training choice for various reasons including more streamlined education, less general surgical time, and integration of cardiovascular and pulmonary medicine. Due to anonymity, we are unable to determine the distribution of trainee programs amongst respondents (e.g. multiple people responding from within the same program). As a result, there may be skewed representation of one program where certain patterns are more prevalent. Another limitation is that this survey does not assess all current cardiothoracic surgery trainees in the United States. Therefore, it is not entirely representative of the current trainee pool. In addition, an individual’s interpretation or varied terms may affect how they answer. For example, a trainee’s personal understanding of adequate experience, comfort with procedures, harassment and diversity may skew how they answer a question. Future efforts would be aimed at distribution to the broader pool, potentially with directed support from individual programs.
There is little data evaluating the effectiveness of the anonymous program surveys. The lack of this information raises concern that the current method fails to identify the real issues within current cardiothoracic surgery (CT) training programs, thus limiting opportunities to identify ways to correct potential problems in a meaningful way. Several factors weigh on a trainee's willingness to be honest on the annual survey. One is the impact on their training program. Often, highlighting grievances can lead to the program being placed on probation or potentially shut down. This could have a significant impact on trainees who are not only are dependent on the program for their training and future career preparation, but their income. The risk of having one’s program placed on probation (and consequently being unable to complete training if the program is shut down) is likely higher than the benefit of airing grievances that trainees may feel are minor. Additionally, trainees may consciously or subconsciously be affected by fear of retaliation by faculty in their program. Although the ACGME surveys are designed to be anonymous, there may be a concern that the results can be traced back to the trainee. A suggestion for managing this fear is to have trainees complete the survey after they have completed their training, almost as an “exit interview”. The benefit of this is that it removes the fear of immediate, potentially detrimental effects on the program. However, some may argue that this would result in a delay in intervention on the part of the ACGME if something significant is reported.
Conclusions
Training future cardiothoracic surgeons is a challenging and sometimes unrewarding process. Technical readiness, cognitive development, and clinical savvy must be balanced with quality of life, mentorship, and mental health. At times, the demands of this field make it difficult to appropriately balance both sides while trying to produce competent, safe surgeons in a limited training period. In addition, this development needs to take place while adjusting to a changing society where the calls for greater inclusion and diversity get louder. It would only serve to benefit the world of CT surgery and our patients if efforts are made to assess the experience of trainees in a reliable way, and utilize the feedback obtained to continually improve programs across the country.
Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- ACGME Resident/Fellow and Faculty Surveys (2022).
- Powell M, Wilder F, Obafemi O, et al. Trends in Diversity in Integrated Cardiothoracic Surgery Residencies. Ann Thorac Surg (2022).
- US Census Bureau. QuickFacts: United States (2022).
- Association of American Medical Colleges. Diversity in Medicine: Facts and Figures 2019. Figure 18. Percentage of all active physicians by race/ethnicity (2022).
- Association of American Medical Colleges. Physician Specialty Data Report. Active Physicians by Sex and Specialty (2017).
- Ortmeyer KA, Raman V, Tiko-Okoye C, et al. Women and Minorities Underrepresented in Academic Cardiothoracic Surgery: It’s Time for Next Steps. Ann Thorac Surg 112 (2021): 1349-1355.
- Mata DA, Ramos MA, Bansal N, et al. Prevalence of Depression and Depressive Symptoms Among Resident Physicians: A Systematic Review and Meta-analysis. JAMA 314 (2015): 2373-2383.
- Lebastchi AH and Yuh DD. Nationwide survey of US integrated 6-year cardiothoracic surgical residents. JTCVS 148 (2014): 401-407.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 