100 Years of Progress From Sistrunk to Robot: Surgical Technique for Lingual Thyroglossal Duct Cyst
Courtney Brooke Shires1*, Merry Sebelik2
1West Cancer Center, 7945 Wolf River Blvd, Germantown, TN 38104, USA
2Department of Otolaryngology, Head and Neck Surgery, Emory University, Medical Office Tower, 11th floor, 550 Peachtree Street NE, Atlanta, GA 30308, USA
*Corresponding Author: Courtney Brooke Shires, West Cancer Center, 7945 Wolf River Blvd, Germantown, TN 38104, USA
Received: 13 May 2025; Accepted: 27 May 2025; Published: 12 August 2025
Article Information
Citation: Courtney Brooke Shires, Merry Sebelik. 100 Years of Progress From Sistrunk to Robot: Surgical Technique for Lingual Thyroglossal Duct Cyst. Journal of Surgery and Research. 8 (2025): 402-409.
View / Download Pdf Share at FacebookAbstract
Objective: For thyroglossal duct (TGD) cysts which extend into the tongue base, or have had failed prior excision, exposure through the neck can be challenging. The aim of this study is to describe a case series of patients who underwent combined transcervical and transoral robotic surgery (TORS) to completely excise large or recurrent lingual TGD cysts.
Methods: Retrospective chart review of a case series of 5 adult patients who underwent combined Sistrunk and TORS approach to treat large or recurrent lingual TGD cysts at a tertiary care institution.
Results: 3/5 patients had undergone excision in the past, with cyst recurrence deep to the hyoid bone and extending into the tongue base. 2/5 had not had prior surgery, but the cyst was primarily within the tongue base. All patients underwent combined excision, with the TORS component completed first before the transcervical exposure. All patients required pharyngotomy by the nature and location of the TGD cyst, and all underwent primary closure through the neck incision. All healed well, resumed oral intake, and have demonstrated no recurrence in 2-year follow-up.
Conclusion: A combined transcervical and transoral approach is feasible and successful in treating the adult patient with large or recurrent lingual TGD cysts that have supra- and infrahyoid extension.
Keywords
Sistrunk, Thyroglossal duct cyst, TORS, Resection, Robotic surgery
Sistrunk articles; Thyroglossal duct cyst articles; TORS articles; Resection articles; Robotic surgery articles
Article Details
Introduction
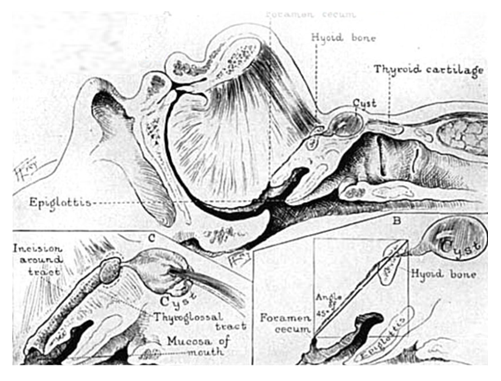
Thyroglossal duct (TGD) cysts are epithelial portions of the thyroid gland remaining after embryonic descent from the tongue base. In 1893, Dr. Hans Schlange described a procedure that required concomitant excision of the central portion of the hyoid bone during a TGD cyst operation. With said procedure, Schlange purported little to no recurrence [1]. In 1920, Dr. Walter Sistrunk took the procedure even further, advising that the suprahyoid region also be excised, along with exploration into and possible extraction of areas within the oral cavity(Figure 1) [2]. In 1928, however, Sistrunk modified his original procedure, recommending that the oral cavity not be explored. Following this modified procedure, Sistrunk purported that practically 100 percent of his patients were cured and had no recurrence [3].
Over time, transcervical excision has become the most common surgical technique to address TGD cysts. For those TGD cysts which extend into the tongue base or have had failed prior excision, exposure through the neck, however, can be challenging. In turn, the removal of thyroglossal duct cysts has seen its share of changes and innovations in overall procedure. Surgical management has traditionally consisted of a formal Sistrunk procedure, but with lingual TGD cysts representing a subset (0.67-8.5%) of total TGD cysts, transoral surgical management has become quite popular, given the lingual TGD cysts are not continuous with the thyroglossal tract [4].
Robotic surgery using the Da Vinci® surgical system was introduced in the early 2000s for use in urology and gynecology. Its magnified three-dimensional vision, diminished surgeon tremor, and superior precision were beneficial to surgeons. The wristed instruments with seven degrees of freedom greatly benefited surgeons in tight spaces [5,6]. Weinstein first described transoral robotic surgery (TORS) in 2007 for radical tonsillectomy [7]. In 2009, the Food and Drug Administration (FDA) approved TORS for resections of T1–T2 malignancies of the oral cavity, pharynx, and larynx, as well as benign head and neck lesions [7-10]. Over the last several years, TORS indications have continued to increase and now include resection of tumors of the larynx, hypopharynx, parapharyngeal space, submandibular space, and skull base [11], as well as neck dissection and thyroidectomy. Robotic access for head and neck surgeries have evolved from transoral approaches to transaxillary and retroauricular approaches [12-14].
Robotic surgery is in the early stages in the pediatric head and neck arena, with more limited experience than in adults. In 2005, two teenage patients were first treated with a robotic transaxillary approach. One patient underwent for a right thyroid lobectomy, and the other underwent placement of a vagal nerve stimulator for intractable seizures [15]. Wu reviewed pediatric patients who underwent robot-assisted neck surgery via a transaxillary or retroauricular approach. He concluded that it was an acceptable option for neck procedures in pediatric patients by most surgeons [16,17]. Erkul evaluated pediatric transoral robotic-assisted surgery and concluded that 90.2% of patients could be treated exclusively with the robot, with only 1 intraoperative complication [18].
The robotic instrumentation itself has gone through much development and evolution. The first Da Vinci® robot approved by the FDA in 2000 was composed of three arms, one with an endoscope and two of them with instruments. Two years later, in 2002, a four-arm version of the robot was approved for clinical use. In 2006 Intuitive Surgical introduced the Da Vinci® S platform with a 3D high-definition (HD) camera vision with a simplified set-up and an interactive touch screen display. Three years later, in 2009, the Da Vinci® Si model was released. The new Si model offered a dual console, allowing for two surgeons to participate and make training easier. In 2014 the Xi model was released with modifications in the patient cart design, with more versatility and flexibility. Its boom-mounted working ports provide docking from any angle and improves access around the patient at any quadrant. In addition, the Xi 30° endoscope can be inverted from the surgeon console without the assistant having to remove and reinstall it. There is also no longer a need for draping, focusing, white balancing, or calibration during surgery [5]. In 2018, the Da Vinci® Single-Port (SP) system was approved by the FDA for its use in urology patients and since then has been used transorally for head and neck patients [19]. This is ideal for smaller mouth patients, including the pediatric population.
Our retrospective study seeks to describe a case series of adult patients who underwent combined transcervical and transoral robotic surgery to completely excise large or recurrent lingual TGD cysts that have infrahyroid extension, as well as to further explore the modifications over time to the Sistrunk procedure and Sistrunk’s varying recommendations.
Methods
We performed a retrospective chart review of a case series of 5 adult patients who underwent combined Sistrunk and TORS approach to treat large or recurrent lingual TGD cysts with infrahyoid extension at a tertiary care institution. We discuss the technique in one of these patients. The same technique was utilized in all 5 of our patients.
This project was approved through expedited review by WCG Institutional Review Board. It was granted approval under protocol number: 2022-002. The Protocol Title was “A retrospective review of clinical outcomes from the West Cancer Center and Research Institute: An Early Adopting Community Cancer Hospital.” On April 14, 2022, WCG IRB approved a request for a waiver of authorization for use and disclosure of protected health information (PHI) for the above-referenced research.
Case
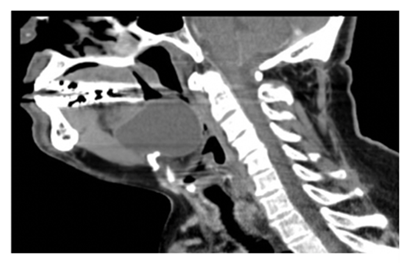
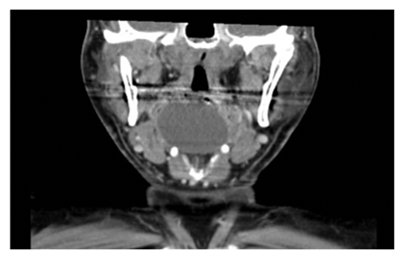
The index patient was a 59-year-old male with obstructive sleep apnea who underwent imaging (Figure 2), for worsening symptoms. Exam revealed a muffled voice and smooth large mass in the vallecula.
Following nasoendotracheal intubation, a 2-0 silk suture was placed through the oral tongue to allow for anterior retraction. A Feyh-Kastenbauer (FK) retractor was then positioned with the short tongue blade and suspended on a Mayo stand. The da Vinci Si surgical robot was docked with a 30° scope for visualization, a spatula tip Bovie in the right arm, and a Maryland dissector in the left arm. Electrocautery was used to make a mucosal cut anterior to the cystic lesion in the base of tongue, down to the cyst capsule. Like the Modified Sistrunk, surrounding normal tissue was taken when excising the capsule. Dissection proceeded along the base of tongue to the vallecula, and the lingual surface of the epiglottic mucosa was transected. After freeing the mass, the robot was undocked and the mouth gag was removed. This concluded the TORS portion of the case.
Then we moved to the transcervical approach. The anterior neck was prepped and draped in usual fashion. A horizontal anterior neck incision was made over the hyoid bone. If present, the platysma was divided near the midline. The strap muscles were exposed and divided in the midline at their raphe and retracted laterally. The cyst was carefully grasped, and careful dissection was performed while bluntly elevating the soft tissue off the posterior and inferior aspects of the cyst. The thyroid cartilage and hyoid bone were palpated as we moved upward and dissected into the suprahyoid region, because the tract and branching ducts reside in this area. The hyoid bone was skeletonized. The infrahyoid strap muscles were freed from the undersurface of the bone. We took care to not injure the hypoglossal nerves above or the superior laryngeal nerves below the hyoid. The middle section of the hyoid bone with the tract was separated from the rest of the hyoid bone with rongeurs and heavy scissors. The middle portion of the hyoid was rotated upward, and the posterior aspect of the hyoid was freed from the surrounding soft tissue with cautery. A finger and a retractor were placed in the patient’s mouth to push the tongue base in the area of the foramen cecum to the neck incision. Then the final incisions were made, maintaining a cuff of muscle around the expected course of the tract, with entering the oral cavity. The midportion of the hyoid bone was resected and the attached cyst pulled through the neck wound.
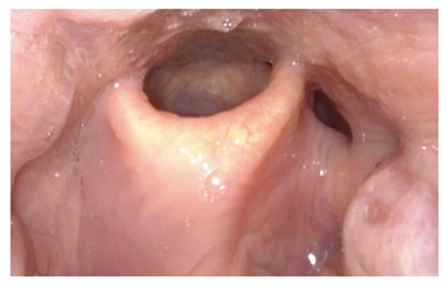
Once the combined transoral robotic and transcervical resections were complete, the surgical opening was thoroughly irrigated. The pharyngotomy was closed primarily with a modified Connell stitch (inverting sutures). The patient was fed via temporary nasogastric tube for 72 hours, and subsequent contrast swallow demonstrated complete healing. Endoscopic view (Figure 3) at 14 days postop revealed fully healed vallecula, and resolution of airway obstruction.
Results
Three of 5 patients had undergone excision in the past, with cyst recurrence deep to the hyoid bone and extending into the tongue base intrinsic musculature. Two of 5 had not had prior surgery, but the cyst was primarily within the tongue base, one massively so (index patient).
All patients underwent combined excision, with the TORS component carried out before the transcervical exposure. All patients required pharyngotomy by the nature and location of the TGD cyst, and all underwent primary closure through the neck incision. All healed well, resumed oral intake, and have demonstrated no recurrence in a minimum of 2-year follow-up.
Discussion
Despite Sistrunk’s assurance that virtually all of his patients were cured following his 1928 modified procedure, recent literature suggests a recurrence rate of up to 10.7%, even ranging from 0 to 19% in primary cases. In revision cases, the recurrence rate increases to 20%, ranging from 0 to 29% [20]. As described by Maddalozzo et al. the recurrence of thyroglossal duct cysts is thought to occur as a consequence of incomplete resection of: 1) infra- and perihyoid tissue and/or 2) microscopic suprahyoid ductules [21]. According to a 2015 study by Huang et al. the hyoid is intact after the first procedure in up to 75 percent of cases. Specifically, Huang and colleagues looked at 44 patients with recurrent thyroglossal duct cysts and found that 33 had an intact hyoid bone post surgery [22]. This study’s findings and numbers correspond well with other studies of a similar nature, particularly those of Mickel and Calcaterra in 1983, Howard and Lund in 1986, and Ahmed and Hartley in 2011. In their study, Mickel and Calcaterra found intact hyoid bones in 24 out of 28 patients (86%) [23], Howard and Lund found intact hyoids in 14 of their 17 patients (82%) [24], and finally, Ahmed and colleagues found intact hyoid bones in 16 of 23 patients (70%) [25]. In turn, completely removing the middle portion of the hyoid is quite difficult, oftentimes given difficult mid-operative visualization and hyoid bone fragmentation [22].
Compounding the difficulty with removing the entire middle portion of the hyoid bone is the fact that the suprahyoid area is also very challenging to navigate. With no obvious landmarks, the presence of multiple, microscopic ducts, a tract that often branches or arborizes, and, most often, an unobvious tract, the suprahyoid region itself poses a major problem to physicians trying to ensure there isn’t a recurrence post thyroglossal duct cyst removal [26]. As noted in Sade’s 1968 study, even the seemingly obvious tract almost always branches into different, miniscule tracts [27]. Thus, despite the more prevalent excision of tissue superior to the thyroid, recurrences still occur as a result of inadequate tract extraction.
As Brown and Judd outline in their 1961 paper, the tract more often than not disappears and is undetectable to the naked eye in the suprahyoid region. For the surgeon, it is then tempting to stop the dissection once the hyoid bone has been reached [28]. With microscopic disease being found superior to the hyoid bone in close to 75 percent of patients, however, surgery termination at the hyoid bone would more than likely lead to recurrence [29]. Even if a tract is purportedly observed during suprahyoid resection, it may not appear in the gross histology, further underlining the point that it’s not necessary to identify a tract [30].
As suggested by Sistrunk, without any attempt to isolate the duct above the hyoid bone, the duct and the tissues surrounding it for a distance of about 3 mm on all sides should be cored out through the muscles of the tongue up to the foramen cecum [3]. Sistrunk also stressed the importance of bearing in mind the direction of the duct and the fact that it’s at an angle of 45 degrees backward and downward toward the foramen cecum (Figure 1). Still, as previously mentioned, we believe that the best approach to the suprahyoid area is to not attempt to isolate the duct and to not measure the width of the tissue to be resected. Instead, it’s important to identify and use the fascia between the geniohyoid and genioglossus, a smooth, glistening layer, to mark the anterior and lateral margins of the resection in the suprahyoid area [31].
TGD cysts confined to the tongue base alone are quite unusual [32]. Utilization of the transoral robotic approach to excise lingual TGD cyst has been described in the literature as single case reports or small series since 2012.
Burkhart presented a series of patients who underwent TORS resection of lingual TGD cyst. Of their 16 patients, 9 presented with labored breathing, shortness of breath, and cyanotic spells or obstructive sleep apnea, while the remaining 7 were identified incidentally on imaging studies due to developmental and speech delay, facial asymmetry, or nystagmus [33]. Endoscopic excision, without a formal Sistrunk procedure, was performed in all cases. With an average follow up of 3.77 years, there were no recurrences. The low recurrence rate of lingual TGD cysts after endoscopic management, along with increased experience using transoral robotic surgery for management of base of tongue squamous cell carcinomas and lingual thyroids, laid the foundation for the removal of a lingual TGD cyst via the above approach [4,34,35]. This approach allows for two-handed manipulation, three-dimensional visualization, tremor filtration, and increased dexterity over endoscopic instrumentation [4].
Aside from Burkhart’s study, 10 other studies have been published on patients with lingual TGD cysts undergoing TORS, with 19 total patients being described: 3 adults, 14 children, and 2 infants (Table 1). 12 of these patients were previously untreated, and were excised or marsupialized through the mouth without cervical incision or hyoid resection [4,18,36-41]. Some of Johnston’s patients also underwent hyoid resection via a TORS approach [42,43].
|
Author |
Year |
#Patients/age |
Technique |
|
Kimple, et al |
2012 |
1/45 yr |
TORS only |
|
Kayhan, et al |
2013 |
1/2 mo |
TORS marsupialization |
|
Carroll, et al |
2016 |
1/6 yr |
TORS only |
|
Erkul, et al |
2017 |
1/child |
TORS only |
|
Kayhan, et al |
2017 |
4/children |
TORS only |
|
Fong, et al |
2018 |
1/68yr |
TORS only |
|
Turri- Zanoni, et al |
2018 |
1/19 yr |
Transoral endoscopic |
|
Turham, et al |
2019 |
1/3 mo |
TORS only |
|
Das, et al |
2023 |
1/7 yr |
TORS only |
|
Johnston, et al |
2023 |
7/children |
TORS only |
|
Total |
19 |
Table 1: Prior case series.
Kimple et al. described a 45-year-old female who presented with sore throat, globus, and throat clearing for 10 years [4]. On examination, she was found to have a 2 x 1.5 cm cystic mass, left of the midline in the vallecula. After undergoing TORS, the cyst was subsequently found to be a lingual TGD cyst, and the patient hasn’t had a recurrence. Fong and colleagues observed a similar cyst in a 68-year-old male. After undergoing TORS, the patient had a smooth recovery and has had no recurrence since [38].
Finally, Turri-Zanoni et al. studied a 19-year-old female that presented with mild dysphagia and phonation impairment. After performing a minimally invasive transoral removal of a bulky cystic mass found at the tongue base, with the assistance of the endoscopic system, the group suggested that such a procedure might be safer and more effective than the transcervical or TORS approach, given the shorter surgery duration and lack of recurrence [40].
Aside from the adults mentioned in the three studies above, Kayhan et al, Carroll, Turham, and Das all suggested that TORS be appropriate in the extraction of TGD cysts in children as well [36,37,41,44]. After performing TORS of a 2 cm cystic mass in the tongue base of a 2-month-old female that presented with respiratory distress, cyanosis, and swallowing difficulties, Kayhan and her team found their patient to be symptom free and able to discharge on postoperative day three [37]. There has not been a recurrence since the surgery.
Carroll saw similar outcomes in a 6-year-old male that presented with obstructive sleep apnea symptoms. Following a TORS of a midline TGD cyst at the base of tongue, the boy has been symptom free and had no recurrence in eleven months of follow-up [36]. Turham, like Turri-Zanoni, recommended a transoral cystectomy as more or less sufficient, noting no post-op complications and a total operating time of 10 minutes in a 3-month-old patient [40,41].
And finally, given the relatively small number of TORS procedures performed for TGD cysts, Erkul and colleagues, along with Kayhan, continued to explore the benefits in their respective studies. Despite only one report, Erkul supported the notion of a TORS procedure in a child for TGD cyst removal, given the low number of intraoperative complications seen in TORS procedures for similar anatomical issues [18]. Kayhan then went a step further, suggesting that TORS is superior to all forms of TGD cyst surgery, based off of better visualization and the robot’s small, flexible arms that allow for quicker and better treatment. Accordingly, this procedure then leads to decreased morbidity compared to open surgical methods [39].
Johnson included 4 patients in his series that underwent TORS resection of lingual TGD but also underwent transoral resection of the central portion of the hyoid bone. He takes advantage of the relatively avascular channel of the midline posterior tongue, vallecula, and posterior hyoid space which provides a safe, relatively bloodless plane of dissection for deep lesions of the midline base of tongue and access to structures in the anterior neck [42,43].
Age does not seem to be a factor in the successful use of our combined approach. Our patients were all adults and had surgery with the Da Vinci® Xi robot. The Da Vinci® robot with a single port will only make for ergonomic ease over a 4 arm robot. One team utilized TORS techniques in a 2-month old [37]. The ports and arms have decreased in required area with time, evolving from three 8 mm ports used in the mouth, to three 5 mm ports, to now a single port transorally. This development will only facilitate the use in smaller patients. As TGD cysts are mostly seen in children, this advancement is welcomed.
Conclusion
A combined transcervical and transoral robotic approach is feasible and successful in treating the adult patient with large or recurrent lingual TGD cyst, allowing hyoid resection and thus minimizing recurrence risk. The evolution of the robot will contribute to application in children along with adults.
Financial support
This particular research received no internal or external grant funding.
Conflicts of interest
The authors report no relevant financial disclosures related to this current work.
Abbreviations
Thyroglossal duct (TGD); transoral robotic surgery (TORS); Feyh-Kastenbauer (FK); high-definition (HD); Single-Port (SP)
Acknowledgements
N/A
Author contribution
Each author contributed to the planning of the article, writing of the article, and editing of the article.
References
- Schlange H. Uber die fistula colli congenita. Arch Klin Chir 46 (1893): 390-392.
- Sistrunk WE. The Surgical Treatment of Cysts of the Thyroglossal Tract. Ann Surg 71 (1920): 121-122.
- Sistrunk WE. Technique of removal of cysts and sinuses of the thyroglossal duct. Surg Gynecol Obstet 46 (1928): 109-112.
- Kimple AJ, Eliades SJ, Richmon JD. Transoral robotic resection of a lingual thyroglossal duct cyst. J Robot Surg 6 (2012): 367-369.
- Morrell ALG, Morrell-Junior AC, Morrell AG, et al. The history of robotic surgery and its evolution: when illusion becomes reality. Rev Col Bras Cir 48 (2021): e20202798.
- Niewinski P., Golusinski W. Current indications and patient selection for transoral robotic surgery in head and neck cancer: A brief review. Wspolczesna Onkol 26 (2022): 91-96.
- Weinstein GS, O’Malley BW, Snyder W, et al. Transoral Robotic Surgery Radical Tonsillectomy. Arch. Otolaryngol. Head Neck Surg 133 (2007): 1220-1226.
- Farooq S, Khandavilli S, Dretzke J, et al. Transoral tongue base mucosectomy for the identification of the primary site in the work-up of cancers of unknown origin: Systematic review and meta-analysis. Oral Oncol 91 (2019): 97-106.
- Vergez S, Cheval M, Chabrillac E. Transoral robotic removal of submandibular sialolith combined with sialendoscopic assistance. Eur. Ann. Otorhinolaryngol. Head Neck Dis 138 (2021): 65-66.
- Quon H, O’Malley BW, Weinstein GS. Transoral Robotic Surgery (TORS) for the Head and Neck: Current and Future Indications. Int. J. Head Neck Surg 1 (2010): 133-140.
- Mendelsohn AH. Transoral robotic assisted resection of the parapharyngeal space. Head Neck 37 (2015): 273-280.
- Garas G, Arora A. Robotic Head and Neck Surgery: History, Technical Evolution and the Future. Orl 80 (2018): 117-124.
- D’Andréa G, Vairel B, Vandersteen C, et al. Is Transoral Robotic Surgery the Best Surgical Treatment for Lingual Thyroid? A Case-Report and Literature Review. Ann. Otol. Rhinol. Laryngol 131 (2022): 39-51.
- Chabrillac E, Morinière S, Jegoux F, et al. Transoral robotic resection of benign tumors of the upper aerodigestive tract: Experience of the French group of GETTEC. Head Neck 40 (2018): 2043-2049.
- Lobe TE, Wright SK, Irish MS. Novel uses of surgical robotics in head and neck surgery. J Laparoend & Adv Surg Tech Part A 15 (2005): 647-652.
- Wu EL, Garstka ME, Kang SW, et al. Robotic neck surgery in the pediatric population. JSLS: J Soci Laparoend Surg 22 (2018): e2018.00012.
- Venkatakarthikeyan C, Nair S, Gowrishankar M, et al. Robotic surgery in head and neck in pediatric population: our experience. Indian J Otolaryngol Head Neck Surg 72 (2020): 98-103.
- Erkul E, Duvvuri U, Mehta D, et al. Transoral robotic surgery for the pediatric head and neck surgeries. Eur Arch Otorhinolaryngol 274 (2017): 1747-1750.
- https://globalrobotics.adventhealth.com/global-robotics-institute/about-institute/da-vinci-sp-robot
- Galluzzi F, Pignataro L, Gaini RM, et al. Risk of recurrence in children operated for thyroglossal duct cysts: A systemic review. J Ped Surg 48 (2013): 222-227.
- Maddalozzo J, Alderfer J, Modi V. Posterior hyoid space as related to excision of the thyroglossal duct cyst. 120 (2010): 1773-1778.
- Huang J, Osterbauer B, Koempel J. Prevalence of an intact hyoid bone at revision excision of a thyroglossal duct remnant. International Journal of Pediatric Otorhinolaryngology 113 (2018): 131-133.
- Mickel RA, Calcaterra TC. Management of recurrent thyroglossal duct cysts. Otolaryngol 109 (1983): 34-36.
- Howard DJ, Lund VJ. Thyroglossal ducts, cysts and sinuses: a recurrent problem. Coll Surg Engl 68 (1986): 137-138.
- Ahmed J, Leong A, Jonas N, et al. The extended Sistrunk procedure for the management of thyroglossal duct cysts in children: how we do it. Clin Otolaryngol 36 (2011): 271-275.
- Kim CH, Byeon HK, Shin YS, et al. Robot-assisted Sistrunk operation via a retroauricular approach for thyroglossal duct cyst. Head Neck 36 (2014): 456-458.
- Sade J, Rosen G. Thyroglossal cysts and tracts: A histological and histochemical study. Ann Otol Rhinol Laryngol 77 (1968): 139-145.
- Brown PM, Judd ES. Thyroglossal duct cysts and sinuses: results of radical (Sistrunk) operation. Am J Surg 102 (1961): 494-501.
- Garcia E, Osterbauer B, Parham D, et al. The incidence of microscopic thyroglossal duct tissue superior to the hyoid bone. Laryngoscope 129 (2019): 1215-1217.
- Soucy P, Penning J. The clinical relevance of certain observations on the histology of the thyroglossal tract. J Ped Surg 5 (1984): 506-509.
- Koempel J. Thyroglossal duct surgery: a reliable, reproducible approach to the suprahyoid region. International J Ped Otorhinolaryngology 78 (2014): 1877-1882.
- O’Malley BW Jr, Weinstein GS, Snyder W, et al. Transoral robotic surgery (TORS) for base of tongue neoplasms. Laryngoscope 116 (2006): 1465-1472.
- Burkart CM, Richter GT, Rutter MJ, et al. 3rd Update on endoscopic management of lingual thyroglossal duct cysts. Laryngoscope 119 (2009): 2055-2060
- May J, Newman J, Padhya T. Transoral robot-assisted excision of a lingual thyroid gland. J Robotic Surg 5 (2011): 217-220.
- Byeon HK, Ban MJ, Lee JM, et al. Robot-assisted Sistrunk’s operation, total thyroidectomy, and neck dissection via a transaxillary and retroauricular (TARA) approach in papillary carcinoma arising in thyroglossal duct cyst and thyroid gland. Ann Surg Oncol 19 (2012): 4259-4261.
- Carroll DJ, Byrd JIK, Harris GF. The feasibility of pediatric TORS for lingual thyroglossal duct cyst. Int J Pediatr Otorhinolarngol 88 (2016): 109-112.
- Kayhan FT, Kaya KH, Koc AK, et al. Transoral surgery for an infant thyroglossal duct cyst. Int J Pediatr Otorhinolaryngol 77 (2013): 1620-1623.
- Fong S, Hodge JC, Foreman A, et al. Transoral robotic excision of a lingual thyroglossal duct cyst. J Robot Surg 12 (2018): 357-360.
- Kayhan FT, Yigider AP, Koc AK, et al. Treatment of tongue base masses in children by transoral robotic surgery. Eur Arch Otorhinolaryngol 274 (2017): 3457-3463.
- Turri-Zanoni M, Battaglia P, Castelnuova P. Thyroglossal Duct Cyst at the Base of Tongue: The Emerging Role of Transoral Endoscopic-Assisted Surgery. J Craniofac Surg 29 (2018): 469-470.
- Turhan M, Bostanci A. Robotic resection of lingual thyroglossal duct cyst in an infant. J Robot Surg 13 (2019): 331-334.
- Johnston DR, Maurrasse SE, Maddalozzo JM. Avascular midline oropharyngeal anatomy allows for expanded indications for transoral robotic surgery in pediatric patients. J Robot Surg 17 (2023): 1803-1808.
- Johnston DR, Maurrasse SE, Maddalozzo J. Transoral Robotic Surgery Excision of Lingual Thyroglossal Duct Cysts Including the Central Hyoid Bone.Laryngoscope 131 (2021): E1345-E1348.
- Das S, Sekar R, Alexander A, et al. Transoral Robotic Excision of Paediatric Lingual Thyroglossal Duct Cyst. Indian J Otolaryngol Head Neck Surg 75 (2023): 2423-2426.



 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 