Clinical impact of Gynaecological Prediction models on decision making of both patients and doctors: A Prospective survey study
Stevens KYR1,2*, Vander Donck E2, Houterman S3, Gelderblom M1, Jansen CLR4, Knol GJA5, Weyers S2, Schoot BC1,2
1Department of Obstetrics and Gynaecology, Catharina Hospital, Michelangelolaan 2, 5623 EJ Eindhoven, the Netherlands
2Department of Obstetrics and Gynaecology, Women’s Clinic, Ghent University Hospital, Corneel Heymanslaan 10, 9000 Ghent, Belgium
3Department of Education and Research, Catharina Hospital, Michelangelolaan 2, 5623 EJ Eindhoven, the Netherlands
4Department of Obstetrics and Gynaecology, ZorgSaam Hospital De Honte, Wielingenlaan 2, 4535 PA Terneuzen, the Netherlands
5Department of Obstetrics and Gynaecology, Amphia Hospital, Molengracht 21, 4818 CK, Breda, the Netherlands.
*Corresponding Author: Stevens KYR, Department of Obstetrics and Gynaecology, Catharina Hospital,
Present address: Michelangelolaan 2, 5623 EJ Eindhoven, the Netherlands.
Received: 16 April 2025; Accepted: 24 April 2025; Published: 07 August 2025
Article Information
Citation: Stevens KYR, Vander Donck E, Houterman S, Gelderblom M, Jansen CLR, Knol GJA, Weyers S, Schoot BC. Clinical impact of gynaecological prediction models on decision making of both patients and doctors: A prospective survey study. Journal of Surgery and Research. 8 (2025): 392-401.
View / Download Pdf Share at FacebookAbstract
Background: Clinical prediction models are increasingly used to assist well-informed decisions about patient treatment, thereby facilitating the shared decision-making process.
However, it remains unclear in how far doctors and patients will use these predicted percentages, and if thresholds for these individualised failure rates differ within and between these groups.
Objective: This study investigated how the outcomes of a gynaecological prediction model impact the clinical decision-making process for both patients and professionals.
Design: A prospective multicentre survey study with data collection between 1st of February 2019 and 1st of August 2020. Dutch-speaking female patients (age 18-75 years) visiting the gynaecology outpatient department, and physicians involved in benign gynaecology were asked to participate.
Interventions: Both patients and professionals gave their baseline treatment preference (Endometrial ablation (EA) or Uterus Extirpation (UE)) after being presented a general known literature-based failure percentage of EA (15%) in a fictive case. Subsequently, their treatment preference was asked again after knowing a personal failure rate generated by a prediction model (61%).
Results: Patients and professionals significantly changed their choice from EA to UE in respectively 48.3 % and 48.9 % (p < 0.001). The average acceptable failure rate for EA showed no significant difference between patients (56.7%) versus professionals (53.6%) (p = 0.145). Motives for choice of treatment seemed to differ between patients and professionals, underscoring the importance of considering these differences in the decision-making process.
Conclusion: A personalised clinical prediction model can influence treatment choice compared to counselling based on general information. The additional information, provided by such a model contributes to improved counselling and optimises shared decision-making, potentially enhancing overall satisfaction.
Keywords
<p>Prediction model, Shared decision, Endometrial ablation, Counselling, Clinical application</p>
Article Details
Introduction
Shared decision-making is a collaborative process in which choices are made through mutual consultation, with both the patient and professional possessing sufficient knowledge [1]. This type of informed decision-making is increasingly being used and promoted in clinical care [2,3]. Patients seek additional information about their condition and prefer to play a more active role in decisions regarding their health. However, they also depend on their consulting professional to provide guidance and educate them their treatment options [4,5]. The professional contributes technical knowledge and clinical experience regarding the efficacy of an intervention. On the other hand, the patient serves as expert concerning the impact that the intervention will have on her life. Both parties’ expertise is essential for ensuring patient-centred and effective care to enhance patient’s quality of life [1]. In brief, shared decision-making involves understanding the evidence concerning risks and benefits associated with all options while considering patient’s values and preferences [1,2,6].
Decision aids, including clinical prediction models, are increasingly utilized in clinical practice. They aid in selecting the optimal treatment and improve shared decision-making by supporting patient counselling [7]. It is designed to complement, not replace, physician counselling [2].
Stevens et al. previously developed a failure- and re-intervention prediction model for endometrial ablation (EA) [8]. After entering individual variables into the models, the outcome shows individualised failure rates that differ from the overall published failure levels of 15-20% [8,9]. Patients are commonly informed to have a general failure rate based on literature and information from the manufacturer. However, this approach is too general and lacks personalisation. The importance of selecting patients with the ‘right’ characteristics for success of treatment is underemphasized by the general approach, along with recognizing that certain characteristics are more strongly associated with treatment failure.
Literature indicating which factors contribute to a lower success rate is available. However, apart from El Nashar et al’s predictive model [10], there has been no personalised information provided to patients about EA, allowing them to understand how their personal characteristics affect the procedure’s success.
Contrastingly, incorporating a more individualised predicted percentage into the decision-making process can assist both patient and professional in making informed choices. However, it remains unclear to what extent doctors and patients will use these predicted percentages, what concretely acceptable height of thresholds for failure are, and in how far thresholds for these individualised failure rates differ within and between patients and doctors.
Following internal and external validation of failure and re-intervention prediction algorithms, this study investigates how the outcomes of a prediction model influence clinical decision-making for both the patient and professional. The previously developed failure model, to predict failure of EA in patients experiencing heavy menstrual bleeding, served as example in this prospective survey study [11].
Material and Methods
Study design
A prospective survey study was developed to determine how the results of a gynaecological prediction model might affect the decision-making process for both patients and professionals.
The study received approval from the local medical ethical boards of all three participating hospitals. Two non-university teaching hospitals[1] and one regional hospital[2] in the Netherlands participated in this study.
Two dedicated surveys were developed, admitting the differences in patients’ and professionals’ perspectives concerning their treatment choices.
Participants and recruitment
Patients
Dutch-speaking females (age 18-75 years) visiting the gynaecology outpatient department for benign gynaecological complaints, were invited to complete a survey.
During pre-visit registration, patients were asked to participate in the study.
If patients consented, they completed a paper or online survey during the pre-consultation waiting time.
Consent for the survey was assumed if patients signed to participate, following study explanation. Patients were informed about the approximate time to completion of the survey, the study’s purpose, and the anonymously handling of data. No incentives were provided.
Data protection of the online survey was conducted through an authorised account, managed by one of the researchers (KS).
Data collection occurred between the 1st of February 2019 and the 1st of August 2020, with a delay in data collection due to COVID-19.
Professionals
Physicians involved in the gynaecological field (gynaecologist, PhD-researchers and residents) were invited to participate in the study. Invites for the medical staff were sent online through approached heads of gynaecology departments in the Netherlands and Belgium. A reminder was sent after four and six weeks.
Instrument development and content
To account for potential differing perspectives of patients and professionals, two different surveys were created.
The surveys underwent testing and subsequent adjustments for comprehensibility, with input from independent female volunteers. All questions were based on outcomes of previous research leading to the construction of our prediction models [8].
Patients survey:
Surveys were accessible online by the use of google forms [12] or could be completed on paper. It was possible to stop the survey at any time or to change answers afterwards. Most fields in the web-based survey were obligatory to minimise missing data. The survey consisted of three sub-sections, with a total of 47 questions in all sections (Appendix 1). Because a choice which needed to be made in the third subsection, respondents answered a total of 35 questions.
There were twenty-six multiple choice questions, of which four providing an option for additional comments. Two questions were open-ended, and seven questions required scoring on the Likert scale (1 = strongly disagree, 5 = strongly agree).
The first section contained baseline characteristics including age, education level, parity, previous caesarean section (Yes/ No), postmenopausal status, and complaints of heavy menstrual bleeding. Furthermore, commonly used decision grounds for patients (physician expertise, information gained through internet, prior experience of family or friends) were explored.
In the second part, patient’s expected success rate was asked for four different types of surgery (appendectomy, inguinal hernia repair, caesarean section, and endometrial ablation).
The third and final part of the survey contained a hypothetical fictional case.
In the first part of the case, participants were provided with a brief overview of background information, including general information about treatments for heavy menstrual bleeding and the advantages and disadvantages of EA and hysterectomy (UE) as treatment options. Drug related options (such as oral contraception and Mirena hormonal IUD) proved ineffective as treatment options in this fictional case. A general failure rate of 15% for EA was mentioned. Following this information, patients were asked to choose between EA or UE and describe their specific reason(s) for the chosen treatment. In both options patients could also fill in additional reasons.
Subsequently, patients were informed about the possibility of a personal prediction model. In this hypothetical case, the personalised failure rate of EA was calculated at 61%. Considering this individualised failure percentage, patients were then asked whether they would still opt for the same treatment.
Furthermore, participants were asked to indicate a specific percentage of EA failure rate they would personally find unacceptable, thereby excluding EA as potential treatment. Motives for their chosen percentages were asked, participants could fill in additional reasons as well.
Survey for professionals:
Surveys were accessible online by the use of google forms [13] or could be completed on paper. Participants were able to change their answers in both versions. Most of the web-based survey fields were, just as with the patients’ survey, obligatory to fill in, to minimise missing data.
The survey was structured in the same way as that of the patients to easily compare the data where appropriate. It also consisted of three subsections, with a total of 37 questions. (Appendix 2). Depending on their choice of treatment after reading the same case, only 23 or 24 questions needed to be filled in.
Fifteen were multiple choice questions; of which three providing an option for additional comments. Two questions were open-ended and depending on their choice, eight or nine questions required scoring on the Likert scale.
The first section contained questions about demographics and current work status, including: age, country of employment, subspecialty and whether they performed EA. Furthermore, we asked which device was used for EA in their hospitals and inquired as to whether professionals had positive or negative thoughts about EA in general.
In the second part, the professionals’ perception of success rate was asked for the same four operations (appendectomy, inguinal hernia repair, caesarean section and EA) as in the patient survey.
The last part of the survey contained the same fictional case, with a similar brief overview of background information about EA as provided to the patients. However, this time professional jargon was used. The same general failure rate of 15% for EA was mentioned. Based on this information, the professionals were also asked to make a choice and describe the specific reason(s) for the chosen treatment, EA or UE. Additional reasons could be filled in if necessary.
Subsequently, they were informed about the possibility of a personal prediction model with the same individualised failure rate of EA being about 61%. Considering this personalised failure percentage, professionals were asked whether they would still opt for the same treatment. Furthermore, they were also asked to indicate a specific percentage of EA failure rate they would personally find unacceptable, thereby excluding EA as potential treatment. Motives for their chosen percentages were asked, where professionals could fill in additional reasons as well.
Statistical data analysis
IBM SPSS statistics, software version 26.0 (IBM Corp., Armonk, NY, USA) was used to perform statistical analysis.
Baseline characteristics of both patients and professionals are mentioned in table 1. Categorical variables were reported as numbers and frequencies, continuous variables as means with standard deviations or median and minimum-maximum, depending on normality.
Frequencies were used to scale the multiple-choice questions. The Likert scale was classified as disagreement (score 1 or 2), neutral (score 3), or agreement (score 4 or 5).
A Chi-square test or T-test was used, depending on normality, to calculate possible significant differences. A p-value <0.05 was considered significant.
Results
Surveys with at least 75% of the answers completed were included.
Results are summarised in the category of patients and professionals.
Patients
A total of 607 surveys were filled in, of which 585 available for analysis.
Twenty-two surveys were excluded, of which thirteen due to incompleteness, and four were filled in incorrectly. Five surveys were excluded from analysis due to patient age above 75 years.
|
Characteristic |
Patient participants (N=585) |
|
|
N |
Frequency or median * |
|
|
Age (y) |
581 |
38 (18-75) |
|
Current Child Wish |
585 |
48.9% |
|
Gravida (No.) |
585 |
2 (0-18) |
|
Parity (No.) |
585 |
1 (0-6) |
|
Previous caesarean section |
585 |
13.5% |
|
Sterilisation |
585 |
6.7% |
|
Amenorrhea |
585 |
41.7% |
|
Duration of menstruation (No.) |
575 |
5 (0-32) |
|
Duration of menstruation > 7 days |
75 |
13.0% |
|
Dysmenorrhea |
584 |
76.0% |
|
Menorrhagia |
584 |
33.7% |
|
Familiar with EA |
584 |
43.3% |
|
Treated by EA |
584 |
4.3% |
|
Knowing UE |
584 |
91.6% |
|
Treated by UE |
585 |
3.4% |
|
Characteristic |
Professional participants (N=102) |
|
|
N |
Frequency or median* |
|
|
Age (y) |
93 |
34 (24-66) |
|
Performing EA |
100 |
Yes 62.0% |
|
No 38.0% |
||
|
Function |
102 |
Gynaecologist 46.1% |
|
Resident 47.0% |
||
|
PhD 6.9% |
||
|
Country |
97 |
Belgium 29.9% |
|
The Netherlands 70.1% |
||
|
Type of EA if being performed |
97 |
NovaSure ® ** 74.3% |
|
Bipolar resection (Hysteroscopic resection) 19.6% |
||
|
Thermablate ® *** 4.1% |
||
|
Thermachoice ® **** 1.0% |
||
|
Minitouch ® ***** 1.0% |
||
*Categorical variables are mentioned as frequencies, continuous variables as median and minimum-maximum, since data was not normally distributed.
** NovaSure ® by Hologic, Marlborough, US
*** Thermablate ® by Idoman Tearanta, Ireland
**** Thermachoice ® by Ethicon, Sommerville, US
***** Minitouch ® by Minitouch, UK
Table 1: General characteristics of the survey participants (both patients and professionals)
Table 1 shows baseline characteristics of both patients and professionals. The median age of the patients was 38 years (range 18-75), the median gravidity was two (0-18), whereas the median parity was one (0-6). Of the patients, 13.5% (N = 79) had undergone previous caesarean section, and 6.7% (N = 39) had a previous sterilisation.
Amenorrhoea was found in 41.7% (N = 244) of the patients, 76.0% (N = 444) and 33.7% (N = 197) have or have had dysmenorrhea and menorrhagia respectively.
43.4% (N = 253) of the patients were familiar with EA, and 4.3% (N = 25) underwent an EA themselves.
Of the patients who were familiar with EA, 35.2% (N = 89) was positive, 61.6% (N = 156) neutral and 2.4% (N = 6) was negative about it. Two patients (0.8%) did not mention how they felt about EA beforehand.
UE was known by 91.6% (N = 535) of the patients, 3.4% (N = 20) had undergone UE.
Based on our survey, we observed that patients made the decision of their treatment based on the knowledge of the doctor, internet or books, experience of their friends or family or a combination of these factors.
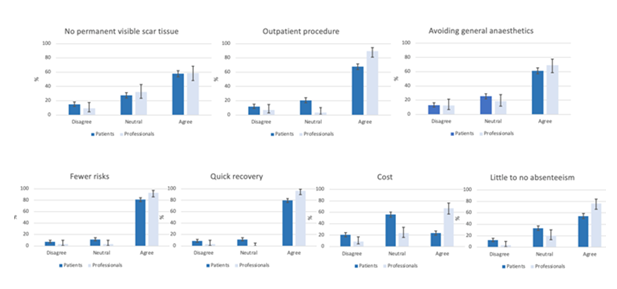
After reading the case and knowing the general failure rate of EA being 15%, a total of 86.7% (N=507) of the women preferred EA over UE. The main reason for their choice seemed to be that EA has fewer risks (81.1%). Other notable motives included: Quick recovery (79.7%), avoiding general anaesthetics (61.3%), the fact that EA can be performed as an outpatient procedure (67.9%) and the absence of a permanent visible scar (57.8%) as illustrated in figure 1.
Age <40 was a significant factor for choosing EA over UE (p-value 0.038).
When the personal predicted failure rate appeared to be 61% (instead of the previously mentioned 15% in the general population), 51.7% (N=262) of the patients that initially chose EA, maintained their original preference. The reason for their choice was multifaceted, including beliefs that EA has fewer risks compared to UE, the perceived benefits outweigh the drawbacks, and the desire to retain their uterus.
A significant total of 48.3% (N=245) changed their preference from EA to UE (p-value < 0.001) as shown in table 2. The main factor contributing for this switch was that the failure rate in this fictional case was too high.
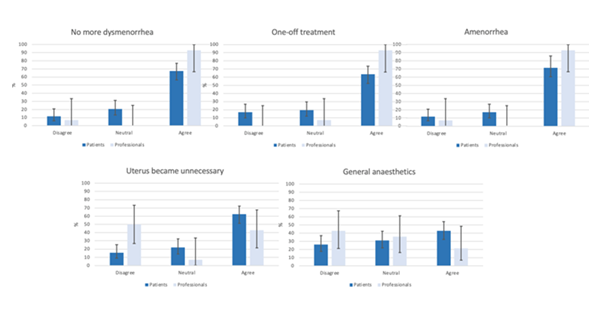
After reading the case and being aware of the general failure percentage of EA being 15%, 13.3% (N=78) opted UE as treatment, based on a combination of motives, primarily: amenorrhoea (71.4%) and no more dysmenorrhea (67.5%). Other important reasons were: no more need for contraceptives (65.0%), one-time treatment (63.6%) and no need for a uterus (62.3%) as shown in figure 2.
From the patients who initially opted UE, 97.4% (N=76) still did this after considering the personal percentage of 61%. Two patients (2.6%) switched from UE to EA after knowing the personal calculated failure rate of EA.
Age was not a significant factor in the choice for EA or UE after knowing the personal failure rate.
Patients thus significantly adapted their treatment preference after reading the personal failure rate of 61% (p-value < 0.001).
The average failure percentage accepted by the patients who chose EA was 60.2% (10-100), 33.5% (10-80) for those who chose UE, and 56.7% (10-100) of all the patients together as shown in table 3.
Additional inquiry showed that patients who thought negatively about EA, comparatively did not chose UE over EA (p-value 0.321); even after knowing the personal failure rate (p-value 0.212). Patients who underwent EA themselves, did not chose EA over UE (p-value 0.358). Similar findings were shown after giving the personal failure percentage (p-value 0.897). On the contrary, patients with a history of UE, preferred UE over EA (p-value <0.001) and kept their initial stance after knowing the personal calculated failure rate (p-value 0.021).
Patients who have or had experienced problems of menorrhagia themselves, also changed their choice significant from EA to UE, after reading the fictional case (p-value <0.001).
Professionals
In the group of the professionals there were 102 respondents, with all surveys available for analysis.
62% stated that they perform EA in their daily practice. The different kinds of EA used were: (Hysteroscopic) bipolar resection (19.6%, N=19), NovaSure® by Hologic, Marlborough, US (74.3%, N=72), Minitouch® by Minitouch, UK (1%, N=1), Thermablate® by Idoman Tearanta, Ireland (4.1%, N=4), and Thermachoice® by Ethicon, Sommerville, US (1%, N=1).
The median age of the professionals was 34 years (24-66). 29.9% (N = 29) had the Belgian nationality, 70.1% (N = 68) were Dutch. 46.1% (N = 47) were gynaecologists, 47.0% (N = 48) were residents and 6.9% (N = 7) were PhD students as shown in table 1.
After reading the case and being aware of the general failure rate of EA being 15%, a total of 86.3% (N=88) of the professionals preferred treatment with EA over UE. The main reason for their choice seemed to be that EA has quick recovery (96.6%), fewer risks (93.2%) and is an outpatient procedure (89.7%). Other notable motives were little to no absenteeism (76.1%) as shown in figure 1. Age of the professionals was not a significant factor influencing choice of EA or UE after knowing the general failure rate.
When the failure rate seemed to be 61% based on the personal calculated percentage (instead of the previously mentioned 15% in the general population), 51.1 % (N=45) of the professionals that initially chose EA, persisted in their choice. A total of 48.9 % (N= 43) significantly changed their choice (p-value < 0.001) from EA in UE as shown in table 2. The most important reason for this switch was the high failure rate.
|
Percentage endometrial ablation as preferred treatment option |
||||
|
Informed about the general failure percentage (15%) |
Informed about the personalised failure rate (61%) |
Patients that switched from EA to UE after knowing the personalised failure rate (61%) |
P-value |
|
|
Patients that choose EA before and after personalised failure rate. |
||||
|
Patients |
86.7% (N=507) |
45.1% (N=264) |
48.3% (N=245) |
<0.001 |
|
51.7% (N=262) maintained their choice for EA N=2 switched UE → EA |
||||
|
Professionals |
86.3% (N=88) |
44.1% (N=45) |
48.9% (N=43) |
<0.001 |
|
51.1% (N=45) maintained their choice for EA |
||||
Table 2: Percentage of both patients and professionals choosing EA as preferred treatment option, after knowing the general failure rate of 15% and after knowing the personalised failure rate of 61%.
After being aware of the general failure rate of 15% for of EA, 13.7% (N=14) chose UE as treatment. Notable motives were: amenorrhoea (92.9%), no more dysmenorrhea (92.9%) and one-time treatment (92.9%). Another important reason was patient satisfaction (78.6%) as shown in figure 2.
Age was not a significant factor in the choice for EA or UE after knowing the personal failure rate.
From the professionals opting UE in the first place, 100% (N=14) still did this after being informed of the personal percentage of 61%. Professionals stated to retain their choice because they believed UE was a better solution.
The average failure percentage accepted by the professionals who chose EA was 57.0% (range 20-100), 28.6% (range 10-50) for those who chose UE, and 53.6% (range 10-100) when looked at the average of all the professionals together as shown in table 3.
Professionals significantly adapted their treatment preference after being informed about the individualised failure rate (p-value < 0.001).
|
Threshold of failure rate (preferred EA to UE) |
|||
|
Choosing EA |
Choosing UE |
Whole group |
|
|
Patients |
60.2% |
33.5% |
56.7% |
|
Professionals |
57.0% |
28.6% |
53.6% |
Table 3: The failure percentage of EA where both patients and professionals would no longer choose for this treatment.
Preference of treatment (before and after reading the personalised risk) was independent of country of employment (before: p-value 0.454; after p-value 0.205). Professionals performing EA did not significantly choose EA over UE (p-value 0.158).
Comparing patients and professionals:
Before reading the fictional case, the success rates of same four different surgeries was asked. There were no important differences between the patients and professionals as shown in appendix 3.
After being informed about the general failure rate of EA (15%), no significant difference in treatment preference was observed between the patients and professionals (EA p-value 0.196 or UE p-value 0.347). When knowing the personal adapted percentage (61%), no significant difference in choice of treatment was seen as well (p-value 0.850).
Age appeared to influence the treatment choice in patients but not in professionals.
No significant difference (p-value 0.145) was found for the acceptable failure rate of EA between the whole group of patients (56.7%) and professionals (53.6%). (Table 3).
Motivational differences in treatment preference between patients and professionals were seen. Professionals significantly prioritize the importance of reduced absenteeism and fewer risks with EA as preferred treatment compared to patients. (p-value < 0.001 and p-value 0.020 respectively).
Outpatient procedure, quick recovery and costs were significantly more important to professionals, whereas patients were significantly more neutral concerning these statements (all p-value <0.001)
Avoiding general anaesthetics (p-value 0.319) and not having a permanent visible scar (p-value 0.321) as reasons were not of significant importance (Figure 1).
Reasons for choosing UE as treatment only significantly differed for the idea that the uterus became unnecessary (p-value 0.012), with professionals more frequently disagreeing with this statement than the patients. Amenorrhoea (p-value 0.191), treating dysmenorrhea (p-value 0.123), general anaesthetics (p-value 0.268) and one-time treatment (p-value 0.087) seemed not to differ between patients and professionals. (Figure 2)
Discussion
There is extensive literature on the development of a (good) prediction model [1-3,6,7,14-21]. However, there is limited data regarding the clinical impact of prediction models on patient and professional treatment preferences, particularly in the field of benign gynaecology. What is more effective: conventional counselling that utilizes commonly known data about a treatment, or a personalised prediction model?
A Cochrane review by Légaré et al. found that decision aids increased knowledge, improved risk perceptions, and facilitated choices aligned with patient’s values [2]. Decision aids demonstrated positive impacts on effective patient-provider communication and patient satisfaction. There is an underutilised potential in the field of gynaecology to optimise shared decision-making in settings of clinical uncertainty, potentially influencing, and optimizing concordance in treatment decisions among gynaecologists [1,3,6,11,14-16].
A prediction model is considered clinically useful when it provides more personalised information which can lead to a change in treatment decision. However, the clinical utility of prediction relies on the availability of better treatment options [22]. This study investigated the clinical impact of a prediction model using a fictional case.
We calculated the percentage of both patients and professionals that changed their treatment preference (EA or UE). After knowing the personal failure rate, both changed their preferred treatment from EA to UE (both p-value < 0.001).
Significant motivational differences for treatment preferences in patients and doctors were found. This indicates the importance of not only the prediction model itself, but also the importance of the motives that need to be considered.
Strengths and limitations
The multi-centre and prospective design are strengths of this survey study. The inclusion of patients and professionals from various age groups, as well as professionals from different clinics and sub-specialisms, adds diversity to the study. The surveys used, were based on existing literature and our previously published prediction models, ensuring that all important items were addressed [8,15,23].
Moreover, another strength of the study lies in the ability to compare the various motives influencing the choices of both patients and professionals. This provides a clearer understanding of what holds significance for each group. Furthermore, only surveys with a minimum of 75% completion were included, to minimise missing data.
The recruitment method used may have contributed to the relatively low number of participating professionals, introducing a potential bias of underreporting, as highly motivated individuals might be more inclined to participate in research than less motivated or involved ones. Using both paper and online (open invitation) surveys, a response rate could not be calculated, potentially creating some selection bias in our web-based survey. Additionally, the international generalisability of our findings may be limited since this survey was distributed in the Flemish-speaking part of Belgium and The Netherlands [20,24,25].
Despite testing and adjusting our survey for comprehensibility with the help of independent (lay) female volunteers, during data processing, we noticed some respondents seemed to misunderstand or misinterpreted the question regarding the percentage of failure at which they would no longer choose EA. If necessary, we manually adjusted these percentages based on the provided motives and explanations.
Collecting additional baseline characteristics, such as gender in the professional group and race in the patient group, should be considered in future research to conduct extra sub-analyses. However, most important analyses could be performed with the current collected data.
With the use of (existing) prediction models, we can enhance shared decision-making [26], motives for choice of treatment should be kept in mind. Ideally, an (online) decision aid which can be used prior to a consultation should be developed [17]. This approach allows patients to consider the acceptable failure percentage for specific treatment options and reflect on their motives in advance. Making a well-informed decision together with their treating physician may be facilitated by taking these factors into account.
This study suggests that personalized prediction models influence treatment preferences of both patients and professionals in a hypothetical gynecological case. Further prospective research in clinical settings is needed to validate these findings and to assess the clinical relevance and utility of such models. Additionally, the underlying factors driving decision-making in both patients and professionals could be explored.
Conclusion
Clinical prediction models are increasingly used in healthcare to assist professionals in making well-informed decisions about patient treatment, thereby facilitating shared decision-making [7]. It has been shown to improve both patient satisfaction and health outcomes [1,2,17,22]. It is especially important in circumstances where there are multiple viable treatment options. The use of prediction models has the potential to improve the decision-making process, where personal information can be used to facilitate discussions with patients regarding the risks and benefits of various treatment options [17]. This study investigated how the outcomes of a prediction model impact the clinical decision-making process for both patients and professionals.
In this survey study, both patients and professionals gave their treatment preference (EA or UE) after being presented a general known failure percentage of EA in a fictive case and subsequently after getting a personal failure percentage generated by a clinical prediction model. Patients and professionals significantly changed their choice from EA to UE in respectively 48.3% and in 48.9% (p- value < 0.001). The average acceptable failure rate for EA showed no significant difference between patients (56.7%) and professionals (53.6%) (p-value 0.145). Motives for choice of treatment seemed to differ between patients and professionals, underscoring the importance of considering these differences in the decision-making process.
We can conclude that a personalised clinical prediction model has a notable impact on treatment choices compared to general counseling in a hypothetical gynecological case. The additional information, provided by such a model contributes to improved counselling and optimizes shared decision-making, potentially enhancing overall satisfaction.
Acknowledgments
The authors thank both the patients and professionals for completing the questionnaires and for consenting to participate in our study.
Authorship contribution statement
K.Y.R. Stevens: Conceptualization (lead), writing original draft (lead), formal analysis (lead), methodology (lead), Investigation (lead), writing review and editing (lead) , data curation (lead), E. Vander Donck: writing review and editing (equal), formal analysis (supporting)
- Houterman: formal analysis (supporting), M. Gelderblom: Investigation (supporting), writing review and editing (supporting) C.L.R. Jansen: writing review and editing (supporting) G.J.A. Knol: writing review and editing (supporting)
- Weyers: Conceptualization (supporting), Supervision (lead), writing review and editing (equal). B.C. Schoot: Conceptualization (lead), Supervision (lead), methodology (lead), writing review and editing (equal)
Authors’ disclosure: No disclosures to mention.
Funding statement: Not applicable.
References
- Tucker Edmonds B. Shared decision-making and decision support: their role in obstetrics and gynecology. Curr Opin Obstet Gynecol 26 (2014): 523-530.
- Légaré F, Adekpedjou R, Stacey D, et al. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane database Syst Rev 7 (2018): CD006732.
- Moons KGM, Kengne AP, Grobbee DE, et al. Risk prediction models: II. External validation, model updating, and impact assessment. Heart 98 (2012): 691-698.
- Sarkissian C, Noble M, Li J, Monga M. Patient decision making for asymptomatic renal calculi: balancing benefit and risk. Urology 81 (2013): 236-240.
- Omar M, Tarplin S, Brown R, et al. Shared decision making: why do patients choose ureteroscopy? Urolithiasis 44 (2016): 167-172.
- Van der Steeg JW, Steures P, Eijkemans MJC, et al. Do clinical prediction models improve concordance of treatment decisions in reproductive medicine? BJOG 113 (2006): 825-831.
- Dent THS, Wright CF, Stephan BCM, et al. Risk prediction models: a framework for assessment. Public Health Genomics 15 (2012): 98-105.
- Stevens KYR, Meulenbroeks D, Houterman S, et al. Prediction of unsuccessful endometrial ablation: a retrospective study. Gynecol Surg 16 (2019): 7.
- Bofill Rodriguez M, Lethaby A, Grigore M, et al. Endometrial resection and ablation techniques for heavy menstrual bleeding. Cochrane Database of Systematic Reviews (2019).
- El-Nashar SA, Hopkins MR, Creedon DJ, et al. Prediction of treatment outcomes after global endometrial ablation. Obstet Gynecol 113 (2009): 97-106.
- Stevens KYR, Muller I, Houterman S, et al. External Validation of Models to Predict Unsuccessful Endometrial Ablation: A Retrospective Study. J Surg Res 5 (2022): 385-399.
- Google Forms, online patient questionnaire (2019). Available from: https://goo.gl/forms/0gy1lGJrnJrjLFou2
- Google Forms, online professional questionnaire [Internet]. 2019. Available from: https://goo.gl/forms/XR1yXT9gIhkOVO1P2
- Kappen TH, Van Loon K, Kappen MAM, et al. Barriers and facilitators perceived by physicians when using prediction models in practice. J Clin Epidemiol 70 (2016): 136-145.
- Witteman HO, Maki KG, Vaisson G, et al. Systematic Development of Patient Decision Aids: An Update from the IPDAS Collaboration. Med Decis Making 41 (2021): 736-754.
- Yu CH, Ke C, Jovicic A, et al. Beyond pros and cons - developing a patient decision aid to cultivate dialog to build relationships: insights from a qualitative study and decision aid development. BMC Med Inform Decis Mak 19 (2019): 186.
- Reilly BM, Evans AT. Translating clinical research into clinical practice: impact of using prediction rules to make decisions. Ann Intern Med 144 (2006): 201-209.
- Gelderblom ME, Stevens KYR, Houterman S, et al. Prediction models in gynaecology: Transparent reporting needed for clinical application. Eur J Obstet Gynecol Reprod Biol 265 (2021): 190-202.
- Kappen TH, Van Klei WA, Van Wolfswinkel L, et al. Evaluating the impact of prediction models: lessons learned, challenges, and recommendations. Diagnostic Progn Res 2 (2018): 11.
- Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 6 (2004): e34.
- Woodhouse KD, Tremont K, Vachani A, et al. A Review of Shared Decision-Making and Patient Decision Aids in Radiation Oncology. J Cancer Educ 32 (2017): 238-245.
- Billheimer D, Gerner EW, McLaren CE, et al. Combined benefit of prediction and treatment: a criterion for evaluating clinical prediction models. Cancer Inform 13 (2014): 93-103.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 15 (2005): 1277-1288.
- Eysenbach G, Wyatt J. Using the Internet for surveys and health research. J Med Internet Res 4 (2002): E13.
- Schonlau M. Will web surveys ever become part of mainstream research? J Med Internet Res 6 (2004): e31.
- Martin GP, Mamas MA, Peek N, et al. Clinical prediction in defined populations: A simulation study investigating when and how to aggregate existing models. BMC Med Res Methodol 17 (2017): 1.
Appendix:
Appendix 1 : Survey Patients https://cdn.fortunejournals.com/supply/JSR12717app1.pdf
Appendix 2 : Survey Professionals https://cdn.fortunejournals.com/supply/JSR12717app2.pdf
Appendix 3: Estimated chances of success of different surgeries https://cdn.fortunejournals.com/supply/JSR12717app3.pdf


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 