Efficacy of Intervention Towards Blood Donation to Increase Voluntary Blood Donation
Dr. Fatema Easmin*1, Dr. Md. Ashadul Islam2, Dr. Shariful Islam3
1Medical Officer, Department of Transfusion Medicine, Bangladesh Medical University, Dhaka, Bangladesh
2Ex-Chairman & Head, Department of Transfusion Medicine, Bangladesh Medical University, Dhaka, Bangladesh
3Ex-Dean, Department of Public Health & Informatics, Bangladesh Medical University, Dhaka, Bangladesh
*Corresponding author: Dr. Fatema Easmin, Medical Officer, Department of Transfusion Medicine, Bangladesh Medical University, Dhaka, Bangladesh.
Received: 23 June 2025; Accepted: 30 June 2025; Published: 15 July 2025
Article Information
Citation: Dr. Fatema Easmin, Dr. Md. Ashadul Islam, Dr. Shariful Islam. Efficacy of Intervention Towards Blood Donation to Increase Voluntary Blood Donation. Fortune Journal of Health Sciences. 8 (2025): 688-694.
View / Download Pdf Share at FacebookAbstract
Introduction: Blood is essential for medical treatments, emergencies, and surgeries, yet many countries, including China, struggle with maintaining a stable and sufficient blood supply. One significant challenge is the low retention rate of blood donors. There is a need to increase blood donations from safe and voluntary blood donors.
Aim of the study: The aim of this study was to examine the intervention towards blood donation to increase voluntary blood donation.
Methods: This randomized-controlled trial study at the Imam Training Academy of the Islamic Foundation, Bangladesh, included 200 participants in two groups 100 of each and aged 18 above. Conducted from January 2022 to January 2025, data on before and after intervention toward voluntary blood donation were collected through face-to-face interviews using a semi-structured questionnaire. Statistical analysis was performed with SPSS Version 26, considering a P-value of <0.05 as significant. Ethical clearance was obtained from the Institutional Review Board (IRB).
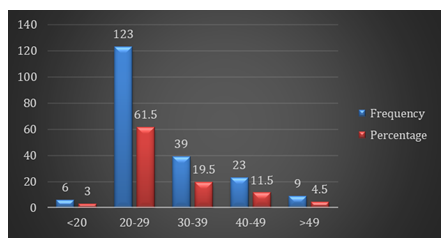
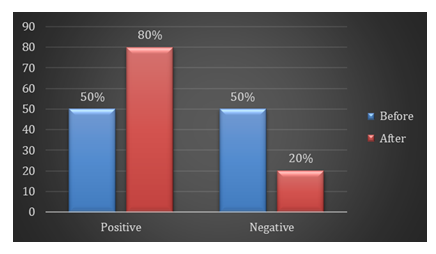
Result: The study found that the majority (61.5%) of participants were aged between 20-29 years, with 19.5% aged 30-39 years. Awareness of blood group and Rh-factor increased from 42% before to 65% after the intervention, though this change was not statistically significant (p = 0.086). We found, before intervention, the respondents were 50% exhibiting a positive attitude and 50% and after intervention, the proportion of respondents with a positive attitude increased to 80%. We also found that before intervention, 45% of respondents had donated blood, which increased to 70% after intervention. Regarding the feelings after donating blood, there was a significant increase in positive feelings from 30% before to 70% after the intervention, with the percentage of indifferent feelings dropping from 15% to 0%.
Conclusion: Regular blood donation counseling sessions could be beneficial for institutions that interact with a large number of people every day. Establishing mobile counseling, campaigns, and educational motivation units could encourage voluntary blood donation. Maintaining voluntary blood donors requires both self-identification as a blood donor and incentive changes.
Keywords
<p>Intervention, Counseling, Voluntary blood donation</p>
Article Details
Introduction
Blood is one of the most valuable donations since it is the essence of life. There is a global blood scarcity that affects blood transfusion services. The current level of blood donation is not keeping up with the daily rise in demand for blood.1 There was a 27.3 lakh unit gap in blood collection in India during 2011–2012, with 72.7 lakh units collected compared to the expected requirement of 100 lakh units.2 Studies on knowledge, attitude, and behavior towards blood donation have been conducted in many countries. Despite demographic and cultural differences, common findings include misinformation about blood donation, fear, a willingness to donate only for family or friends, concerns about selling blood, and a failure to translate positive attitudes into actual donations.3 Most of these studies were conducted outside of India.4,5 Human blood is essential for life, with no available substitutes for its components.6 Blood transfusion, the process of donating blood or blood products from a donor to a recipient, is a crucial life-saving procedure. It is used in both routine and emergency situations to replace blood cells or products lost due to bleeding from injuries, surgeries, malignancies, pregnancy complications, and other medical conditions.7 Despite an estimated 60% of the population in developing countries having sufficient knowledge about blood donation, the donation rate remains significantly lower than in middle- and high-income countries.8,9 This low rate is primarily due to misconceptions, poor knowledge, and unfavorable attitudes toward donation.10,11 Additionally, age, sex, and educational status are key predictors of voluntary blood donation.12,13
Members of the Ethiopian Jewish community have shown a very limited intention to donate blood.14 Annually, 25%–40% of safe blood availability is crucial for those suffering from serious traumas, surgical procedures, civil conflicts, and military operations. Additionally, severe anemia patients often require blood transfusions.15 The shortage of blood supply critically impacts Ethiopian pregnant mothers, leading to preventable maternal deaths.16 Ensuring safe blood availability at all health facilities could significantly reduce maternal deaths and protect lives in emergencies. Despite an annual demand of 250,000 units, only 88,000 units were collected from donors by 2014 in Ethiopia. The country faces major challenges in developing an integrated strategy for voluntary blood donation and recruiting sufficient safe donors, often due to low student knowledge, discouraging attitudes, and poor donation practices. Blood banks and transfusion centers must organize more frequent blood drives and adopt strategies to enhance new donor recruitment to maintain a regular blood supply. One of the four components of the World Health Organization's basic strategy to enhance global blood safety and minimize transfusion risks is to collect blood exclusively from voluntary donors.9,16 The young population is a crucial segment, representing the present and future source of a safe blood supply.17,18
Many young Imams, who are students at Health Science Universities, are emerging as influential advocates for voluntary blood donation. These individuals are typically healthy, active, and well-informed about health issues, making them ideal candidates for regular blood donation. By leveraging their unique position, they can inspire and motivate others to donate blood voluntarily [19]. Encouraging these Health Science Imams to donate blood not only contributes directly to the blood supply but also sets a powerful example for their communities.20 Their involvement in blood donation can be further enhanced by targeted educational campaigns and motivational programs designed to improve their knowledge and attitudes towards blood donation. As future healthcare professionals, these Imams have the potential to become key figures in promoting the importance of voluntary blood donation, serving as role models and motivators within their communities [21]. Despite their potential, there is a notable lack of research focusing specifically on the knowledge, attitudes, and practices of these young Imams regarding blood donation in Bangladesh. This gap underscores the crucial need for developing effective strategies to increase voluntary blood donations. The aim of the study was to examine the intervention towards blood donation to increase voluntary blood donation.
Objectives
The objective of this study was to examine the intervention towards blood donation to increase voluntary blood donation in Bangladesh.
Methodology & Materials
This randomized-controlled trial study was to participate in voluntary blood donation activities through imams. The primary participants were imams and through them blood donors came from different parts of Bangladesh, and the study was conducted at the Imam Training Academy of the Islamic Foundation in Agargaon, Bangladesh, from January 2022 to January 2025. A total of 200 blood donors who were at least 18 years old and who participated in the study before and after the intervention were included. Each of the two groups of 100 participants was randomly assigned. Following the intervention, the group was given motivation, rewards, and counseling. A standardized semi-structured data collection sheet and face-to-face interviews were utilized to gather the necessary information from blood donors. Data collection was conducted using the paper-pencil technique. The semi-structured questionnaire, developed in English, was based on selected variables aligned with the specific objectives. It included questions on knowledge, attitudes, and practices regarding voluntary blood donation. Data were reviewed immediately after each interview and relevant investigations. All pertinent information was collected from each respondent using an interview schedule and predesigned format. Participants had full autonomy to participate in the study, and informed written consent was obtained.
Statistical Analysis: All data were recorded systematically in preformed data collection form and quantitative data was expressed as mean and standard deviation and qualitative data was expressed as frequency distribution and percentage. Statistical analysis was carried out by using Statistical analysis was done by using SPSS (Statistical Package for Social Science) Version 26 for windows 10. P value <0.05 was considered as statistically significant. Ethical clearance was obtained from the local ethical committee to perform the investigation and study.
Result
Figure 1 shows that the majority (61.5%) of our participants were 20-29 years old, followed by 19.5% aged 30-39. Among all participants, 11.5% were aged 40-49 years, 4.5% were over 49 years, and 3% were under 20 years old. The mean age was 30.34±9.83 years.
Table 1: Distribution of study subjects on the basis of their sociodemographic profile
|
Socio-demographic Characteristics |
Frequency |
Percentage |
|
Age |
30.34±9.83 |
|
|
Marital status |
||
|
Married |
126 |
63 |
|
Unmarried |
74 |
37 |
|
Education |
||
|
Primary |
15 |
7.5 |
|
SSC |
38 |
19 |
|
HSC |
65 |
32.5 |
|
Graduate |
40 |
20 |
|
Post Graduate |
34 |
17 |
|
Don't know |
8 |
4 |
|
Occupation |
||
|
Housewife |
1 |
0.5 |
|
Service |
116 |
58 |
|
Student |
49 |
24.5 |
|
Daily labor |
4 |
2 |
|
Business |
5 |
2.5 |
|
Other |
12 |
6 |
Table 1 shows the sociodemographic profile of the respondents. Among the participants, 37% were unmarried, while 63% were married. The highest percentage had completed a Higher Secondary Certificate (HSC) (32.5%), followed by graduates (20%), and those with Secondary School Certificates (SSC) (19%). A smaller portion had only completed primary education (7.5%) or had post-graduate degrees (17%), and 4% were unsure about their educational background. Regarding occupation, the majority worked in service (58%), followed by students (24.5%), with smaller groups in business (2.5%), daily labor (2%), other occupations (6%), and housewives (0.5%).
Table 2: Item wise distribution of response of subjects regarding knowledge of blood donation
|
Items |
Before |
After |
P-value |
|||
|
Frequency |
P (%) |
Frequency |
P (%) |
|||
|
Are you aware of your blood group and Rh-factor? |
yes |
42 |
42 |
65 |
65 |
0.086 |
|
no |
58 |
58 |
35 |
35 |
||
|
Can be a person acquired diseases by receiving infected blood |
yes |
57 |
57 |
76 |
76 |
0.09 |
|
no |
43 |
43 |
24 |
24 |
||
|
How often blood can be safely donated by a person? |
after 3-4 months |
40 |
40 |
74 |
74 |
0.001 |
|
after 5-6 months |
60 |
60 |
26 |
26 |
||
|
Which age group can donate blood? |
18-50 |
57 |
57 |
77 |
77 |
0.085 |
|
20-60 |
43 |
43 |
23 |
23 |
||
|
Best source of donor blood? |
voluntary donor |
58 |
58 |
76 |
76 |
0.001 |
|
relative donor |
42 |
42 |
24 |
24 |
||
Table 2 shows that the awareness and knowledge regarding blood donation among participants before and after an educational intervention. Awareness of blood group and Rh-factor increased from 42% before to 65% after the intervention, though this change was not statistically significant (p = 0.086). Knowledge that diseases can be transmitted through infected blood improved from 57% to 76% (p = 0.090). Significant improvements were observed in the understanding of the safe frequency for blood donation; awareness that blood can be safely donated every 3-4 months rose from 40% to 74% post-intervention (p = 0.001). Additionally, the recognition that the optimal age group for blood donation is 18-50 years increased from 57% to 77% (p = 0.085). Regarding the best source of donor blood, the preference for voluntary donors increased significantly from 58% to 76% (p = 0.001).
Figure 2 shows that the distribution of respondents' attitudes towards voluntary blood donation before and after an intervention. Before the intervention, the respondents were 50% exhibiting a positive attitude and 50% a negative attitude towards voluntary blood donation. However, following the intervention, there was a significant shift in attitudes. The proportion of respondents with a positive attitude increased to 80%, while those with a negative attitude decreased to 20%. This change indicates a substantial improvement in respondents' attitudes towards voluntary blood donation after the educational intervention.
Table 3: Distribution of blood donors according to their practice toward voluntary blood donation
|
Practice related blood donation |
Before |
After |
P-value |
|||
|
Frequency |
P (%) |
Frequency |
P (%) |
|||
|
Have you ever donated blood? |
yes |
45 |
45 |
70 |
70 |
0.013 |
|
no |
55 |
55 |
30 |
30 |
||
|
When was the last time you donated blood? |
<6 months |
22 |
22 |
50 |
50 |
|
|
6-12 months |
8 |
8 |
18 |
18 |
0.051 |
|
|
>12 months |
15 |
15 |
2 |
2 |
||
|
How did you feel after donating blood? |
positive feeling |
30 |
30 |
70 |
70 |
0.001 |
|
indifferent |
15 |
15 |
0 |
0 |
||
|
Reason for Donation |
replacement |
3 |
3 |
1 |
1 |
0.001 |
|
voluntary |
42 |
42 |
69 |
69 |
||
Table 5 shows blood donors according to their practice toward voluntary blood donation. Before the intervention, 45% of respondents had donated blood, which increased to 70% after the intervention (p = 0.013). When asked about the timing of their last blood donation, 22% had donated within the past 6 months before the intervention, compared to 50% afterward (p = 0.051). Additionally, 8% had donated 6-12 months prior before the intervention, increasing to 18% afterward, while those who had donated more than 12 months ago decreased from 15% to 2%. Regarding the feelings after donating blood, there was a significant increase in positive feelings from 30% before to 70% after the intervention (p = 0.001), with the percentage of indifferent feelings dropping from 15% to 0%. The reasons for blood donation also shifted, with voluntary donations increasing from 42% to 69% and replacement donations slightly decreasing from 3% to 1% (p = 0.001).
Discussion
Blood donation is a critical procedure because blood is essential for numerous medical treatments and emergencies, and no artificial substitute currently exists. Blood donations are typically collected through organized blood donation camps, which are set up in various venues such as educational institutions, businesses, and industries. Despite these organized efforts, the demand for blood often exceeds the supply, leading to significant shortages. One major issue is the lack of awareness and knowledge about blood donation among potential donors. Many people are unaware of the simple yet impactful nature of donating blood and may have misconceptions or fears that prevent them from participating. For instance, some may believe that donating blood requires a medical degree or that it is a complex procedure, when in fact, it is a straightforward process that can be performed by almost anyone who meets the basic health criteria. Educating the public about the importance of blood donation and the simplicity of the process is crucial. It’s essential to communicate that donating blood is a simple act that can have a profound impact. One donation can save up to three lives because the collected blood is separated into different components (such as red blood cells, plasma, and platelets), each of which can be used to treat different conditions.22,23 In other study, we found by Wilkinson and Gupta (2016) and Chauhan et al. (2018) provides valuable insights into how interventions can impact community perceptions and awareness regarding blood donation. These studies assessed changes in knowledge and attitudes towards blood donation both before and after specific interventions. Such interventions might include campaigns, awareness programs, or motivational drives aimed at increasing donor participation. Wilkinson and Gupta (2016) focused on understanding how targeted educational efforts could alter perceptions and behaviors related to blood donation. They found that structured interventions led to an improvement in the community's awareness and willingness to donate blood. Similarly, Chauhan et al. (2018) examined the effects of awareness campaigns on different communities, noting that post-intervention data showed increased knowledge and more positive attitudes towards blood donation.24,25 The present study we found, before intervention, the respondents were 50% exhibiting a positive attitude and 50% a negative attitude towards voluntary blood donation and after intervention, the proportion of respondents with a positive attitude increased to 80%, while those with a negative attitude decreased to 20%. In other study findings, conducted in Ambo town, Ethiopia, 47.4% of study participants had a positive attitude towards blood donation,26 which is significantly higher compared to the study conducted in Harar, Eastern Ethiopia, where only 32.9% of participants held a positive attitude towards voluntary blood donation.27 In our study we found that, before the intervention, 45% of respondents had donated blood, which increased to 70% after the intervention. Regarding the feelings after donating blood, there was a significant increase in positive feelings from 30% before to 70% after the intervention, with the percentage of indifferent feelings dropping from 15% to 0%. The reasons for blood donation also shifted, with voluntary donations increasing from 42% to 69% and replacement donations slightly decreasing from 3% to 1%. For instance, another study conducted in the Kingdom of Saudi Arabia (KSA) reported that 14.8% of blood donors were voluntary, while 48.7% were replacement donors and 36.5% were statutory donors.28 We also found, previous studies by Wiwanitkit et al. Mousavi et al. Shenga N et al. and Sabu et al.29-32 A statistically significant improvement in the level of knowledge and awareness was observed when the responses of participants before and after the intervention were analyzed.
Limitations of the study
In our study, the small sample size and short duration of the study period were limitations. Additionally, being questionnaire-based, the study faced potential biases, such as participant bias or memory bias, which may have influenced the responses and led to misleading results.
Conclusion and recommendations
The present study revealed a substantial knowledge gap amongst participants regarding blood donation. Most study subjects had not donated blood and were unaware of the concept of blood donation. Despite efforts by governmental and non-governmental organizations (NGOs) and student groups to conduct blood donation camps and motivational lectures, the country still faces life-threatening conditions due to blood shortages in blood banks. The positive impact of motivational intervention in the current study highlights the need for an approach that includes knowledge dissemination, motivational messages, facts, and figures to change participants’ perceptions and intentions regarding blood donation. This emphasizes the importance of health education and promotion. There is a pressing need to educate and motivate people to become regular volunteer blood donors and to leverage these volunteers to encourage additional youth to participate in blood donation regularly. Blood donation is an urgent necessity, and immediate action is required to disseminate information about its importance to save lives. Raising awareness and motivation for blood donation can significantly influence individuals' willingness to donate blood, ultimately increasing the number of voluntary blood donors. In order to maintain a steady and adequate blood supply and ultimately contribute to the WHO's 2020 target of 100% voluntary blood donation, it is imperative to increase the rate of voluntary and frequent blood donation.
References
- Horton R. Blood supply and demand. Lancet 365 (2005): 2151.
- Blood safety and availability (2014).
- Lownik E, Riley E, Konstenius T, et al. Knowledge, attitudes and practices surveys of blood donation in developing countries. Vox sanguinis 103 (2012): 64-74.
- Sampath S, Ramsaran V, Parasram S, et al. Attitudes towards blood donation in Trinidad and Tobago. Transfusion Medicine 17 (2007): 83-87.
- Mousavi F, Tavabi AA, Golestan B, et al. Knowledge, attitude and practice towards blood donation in Iranian population. Transfusion Medicine 21 (2011): 308-317.
- Action Plan for blood safety. National AIDS Control Organization, Ministry of Health and Family Welfare, Government of India, New Delhi (2007).
- Safety WB, Availability-Fact sheet N. 279 (2014).
- Karim AM, Admassu K, Schellenberg J, et al. Effect of Ethiopia’s health extension program on maternal and newborn health care practices in 101 rural districts: a dose-response study. PloS one 8 (2013):
- Ethiopia Commences World Blood Donor Day 2014 Celebrations. Geneva, Switzerland: WHO (2014).
- Abolfotouh MA, Al-Assiri MH, Al-Omani M, et al. Public awareness of blood donation in Central Saudi Arabia. International journal of general medicine 7 (2014): 401-410.
- Ingale L, Gessesse S and Miruts G. Magnitude and factors associated with voluntary blood donation practice among adult Mekelle population, north Ethiopia: a community-based cross-sectional study. Research & Reviews: Journal of Oncology and Hematology 4 (2019): 5-13.
- Melku M, Terefe B, Asrie F, et al. Knowledge, attitude, and practice of adult population towards blood donation in Gondar Town, Northwest Ethiopia: a community based cross-sectional study. Journal of blood transfusion (2016).
- Alfouzan N. Knowledge, attitudes, and motivations towards blood donation among King Abdulaziz Medical City population. International journal of family medicine (2014).
- Merav BN and Lena G. Investigating the factors affecting blood donation among Israelis. International Emergency Nursing 19 (2010): 37-43.
- Al-Drees AM. Attitude, belief and knowledge about blood donation and transfusion in Saudi population. Pakistan Journal of Medical Sciences 24 (2008): 74.
- About 40% of Ethiopian Mothers Die because of Lack of Enough Blood Donors. Cantabria, Spain: ENSA (2014).
- Amatya M. Study on knowledge, attitude and practice of blood donation among students of different colleges of Kathmandu, Nepal. International Journal of Pharmaceutical and Biological Archives 4 (2013): 424-428.
- Yerpude PN and Jordan KS. A cross-section study on KAP on blood donation Among medical students South India. Int J Med health Sci 2 (2013): 382-5.
- Voluntary blood donation: foundation of a safe and sufficient blood supply. Genève, Switzerland: World Health Organization (2010).
- Melku M, Asrie F, Shiferaw E, et al. Knowledge, attitude and practice regarding blood donation among graduating undergraduate health science students at the University of Gondar, Northwest Ethiopia. Ethiopian journal of health sciences 28 (2018).
- Khan MS, Islam KN, Rana S, et al. Knowledge, attitude, and practice of blood donation: A cross-sectional survey in Khulna city, Bangladesh. Public Health in Practice 7 (2024): 100488.
- Marwaha N: Voluntary blood donation in India: achievements, expectations and challenges. Asian J Transfus Sci 9 (2015): S1-S2.
- Unnikrishnan B, Rao P, Kumar N, et al.: Profile of blood donors and reasons for deferral in coastal South India. Australas Med J 4 (2011): 379-385.
- Wilkinson A, Gupta RS: Perceptions of blood donation amongst the youth. Panacea J Med Sci 6 (2016): 79-82.
- Chauhan R, Kumar R, Thakur S: A study to assess the knowledge, attitude, and practices about blood donation among medical students of a medical college in North India. J Fam Med Prim Care 7 (2018): 693-697.
- Nigatu A, Demissie DB. Knowledge, attitude and practice on voluntary blood donation and associated factors among Ambo University regular students, Ambo Town, Ethiopia. J Community Med Health Educ 4 (2014): 315
- Urgesa K, Hassen N, Seyoum A. Knowledge, attitude, and practice regarding voluntary blood donation among adult residents of Harar town, Eastern Ethiopia: a community-based study. J Blood Med 8 (2017): 13–20.
- Bashawri LA. Pattern of blood procurement, ordering and utilization in a University Hospital in Eastern Saudi Arabia. Saudi Med J 23 (2002): 555-561.
- Shenga N, Pal R, Sengupta S. Behavior disparities towards blood donation in Sikkim, India. Asian J Transfus Sci 2 (2008): 56-60.
- Mousavi F, Tavabi AA, Golestan B, et al. Knowledge, attitude and practice towards blood donation in Iranian population. Transfus Med 21 (2011): 308-317.
- Wiwanitkit V. Knowledge about blood donation among a sample of Thai university students. Vox Sang 83 (2002): 97-99.
- Sabu KM, Remya A, Binu VS, et al. Knowledge, attitude and practice on blood donation among health science students in a university campus, South India. Online J Health Allied Sci 10 (2011): 6.


 Impact Factor: * 6.2
Impact Factor: * 6.2 Acceptance Rate: 76.33%
Acceptance Rate: 76.33%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 