Erie Shores HealthCare’s Experiences and Perceptions of the Critical Care Outreach Team
Angela Ciotoli1, Nadia Pedri2, Michael Riley Jackson Jakob1,3, Neelu Sehgal1, Jaefer Mohamad4, Nima Andre Malakoti-Negad4, Alexandrea Gow1, Tazmeen Yekinni5 and Munira Sultana*,1,5
1Erie Shores HealthCare, 194 Talbot St. W. Leamington, Ontario N8H 1N9
2University of Windsor, 401 Sunset Ave, Windsor, ON N9B 3P4
3Windsor Regional Hospital, Ouellette Campus, 1030 Ouellette Ave, Windsor Ontario N9A 1E1
4Schulich School of Medicine & Dentistry, London, Ontario, Canada, N6A 3K7
5WE SPARK HEALTH Institute, 401 Sunset Ave, Windsor, ON N9B 3P4
*Corresponding author: Dr. Munira Sultana, WE SPARK HEALTH Institute, 401 Sunset Ave, Windsor, ON N9B 3P4
Received: 21 June 2025; Accepted: 06 July 2025; Published: 12 August 2025
Article Information
Citation: Angela Ciotoli, Nadia Pedri, Michael Riley Jackson Jakob, Neelu Sehgal, Jaefer Mohamad, Nima Andre Malakoti-Negad, Alexandrea Gow, Tazmeen Yekinni and Munira Sultana. Erie Shores HealthCare’s Experiences and Perceptions of the Critical Care Outreach Team. Fortune Journal of Health Sciences. 8 (2025): 774-777.
View / Download Pdf Share at FacebookAbstract
Critical Care Outreach Teams (CCOT) have been implemented globally to recognize early signs of patient deterioration and enhance critical care management. Erie Shores Healthcare (ESHC), a rural 72-bed hospital located in Leamington, Ontario, has faced challenges in managing an increasing volume of complex patients, particularly in identifying clinical deterioration in a timely manner. In response, the research team developed a daytime intensivist-led and nighttime RN-led CCOT program to improve early recognition and timely interventions. Data from a NoMAD questionnaire and a retrospective chart audit revealed a positive perception of CCOT among nursing staff, especially in preventing unnecessary ICU transfers. The intervention also significantly reduced the time from initial deterioration signs to key care points, with the nighttime RN-led program demonstrating greater efficiency. These encouraging results, coupled with a forthcoming quantitative study, indicate a strong need to extend CCOT services to 24/7 coverage at ESHC.
Keywords
<p>Critical care, hospital, rural, ICU transfer, Canada</p>
Article Details
Background
Clinical deterioration is defined as a prolonged period of instability from a patient’s baseline physiological status, with warning signs appearing approximately 6.5 hours prior to a major clinical event. If not addressed, a patient’s deterioration may result in admission to a hospital’s intensive care unit (ICU), increased hospital length of stay, and unnecessary costs to the healthcare system [1]. Considering the interval time between the initial first warning sign and an event of advanced deterioration, Critical Care Outreach Teams (CCOT) were developed in England, UK, in the 1990s to provide timely critical care [2]. CCOTs have been replicated worldwide, with the development of Rapid Response Teams (RRTs) or Medical Emergency Teams (METs) in the USA and Australia, respectively [3]. CCOT is a group of trained critical care practitioners who work collaboratively with hospital staff to recognize decompensating patients and mobilize critical care resources for at- risk patients in adult and pediatric settings [3]. The objectives of a CCOT are to 1) reduce admissions to critical care areas, 2) expedite transfers from ICU, 3) educate staff to enable effective recognition and management of deteriorating patients, and 4) ensure transfer of patients to appropriate clinical units best suited for the level of care required [4,5]. CCOT is on alert when a patient shows clinical signs of early deterioration. A Registered Nurse (RN) or physician identify patient deterioration physically observing the changes in vital signs, and/or utilization of a clinical tool such as a National Early Warning Score (NEWS2) which allows risk stratification for at risk for subsequent deterioration and guides reassessments [6].
Given the increasing costs of ICU resources and the limited availability of critical care beds, it is crucial to evaluate the appropriateness of patient admission to an ICU. The CCOT services have thus been adapted to address these challenges, with a significant role in preventing inappropriate ICU admission and help expedite transfer of deteriorating patients to a critical care bed by intervening on signs of deterioration [6]. A recent study revealed that approximately 41% of ICU admissions were avoidable if NEWS2 scores are utilized [5]. In addition, a large, multi-center cohort study by Escobar and colleagues [7] revealed that 17.7% of hospitalized patients who received RRT services were admitted to the ICU compared to 20.9% of patients who did not receive those critical services. A Canadian study by Tillmann and colleagues [8] examined the relationship between a delay in activation of CCOT and patient outcomes. They reported that a delay in CCOT activation of more than or equal to 60 minutes after a patient presents with a high-risk Early Warning Score (EWS) is associated with a 30% increase in the odds of mortality, thus demonstrating that timely CCOT intervention leads to better patient outcomes [8]. Additionally, introduction of CCOT reduced the incidence of unexpected cardiac arrests in the hospital by approximately half, as well as reduced mortality from 77% to 55% after this system was established [9]. Therefore, we conclude that the use of CCOT services in recognizing early warning signs of deterioration and prompting the mobilization of critical care resources to at-risk patients is supported in the literature. Despite the lack of definitive research on the effectiveness of CCOT in improving mortality and morbidity, the main advantages of CCOT program are 1) enhanced collaboration among healthcare professionals, 2) increased efficiency of hospital resource mobilization, and 3) improved quality of care provided [10].
Although CCOT is globally recognized as beneficial, evidence supporting its use in rural Ontario hospitals is nonexistent. Ontario introduced CCOT in 2006 and invested $29.4 million into a new “Critical Care Strategy” initiative [11]. The CCOT was introduced into 26 urban Ontario hospitals, leaving rural hospitals without the funding to implement such an initiative [11]. Thus, the need for an evaluation of CCOT services in rural hospitals is crucial to support that idea.
Erie Shores HealthCare (ESHC), a rural 72-bed hospital in Leamington, Ontario, faces a critical challenge as its inpatient services are utilized at a staggering 130% capacity [12]. The hospital is being pushed to its limits, causing the staff to witness and experience obstacles while trying to care for their at-risk patients, including the critically ill and older populations, who routinely exhibit early signs of deterioration. Failure to rescue these patients may be caused by 1) inadequate clinical assessment due to heavy workloads, 2) insufficient training and resources, 3) delay in notifying the physician, and 4) absence of a clear care pathway. Therefore, this study aims to evaluate the CCOT service at ESHC through a retrospective chart review of several metrics of ICU-admitted patients pre- and post-CCOT intervention. Our goal is to identify if CCOT is improving response times, optimizing resources, and enhancing patient outcomes based on staff perceptions of CCOT activities using a NoMAD questionnaire, ultimately supporting a care model for extending CCOT coverage to 24/7 in line with CCSO guidelines [11].
Methods
Our research question was to identify if the implementation of a CCOT program improves response times, optimize resources, and enhance patient outcomes at ESHC. The study was approved by the University of Windsor’s Research Ethics Board (REB). Each participant's survey responses remained confidential, and no identifying information was collected. The hospital records used for the retrospective chart review were de-identified. The target population in this study was the staff at ESHC. Starting six months prior to the CCOT service roll-out, all part-time and full-time bedside RNs working in inpatient areas received training during their scheduled annual education sessions. New hires to the organization also received education through the hospital-wide orientation sessions. Apart from RNs, allied health providers, including physiotherapists, occupational therapists, speech-language pathologists, and respiratory therapists were educated on CCOT. Physician education was disseminated through presentations at senior leadership and departmental meetings. Additionally, ESHC introduced a dedicated CCOT RN position. Additional experienced RNs (N=5) from the ICU and emergency department (ED) were chosen through expression of interests to be cross trained in CCOT response. This training consisted of a two-day course, one day of didactic learning and one day of simulation training in St. Clair College’s simulation labs in Windsor, Ontario. Furthermore, each trainee underwent two training shifts, termed “buddy shifts,” with experienced CCOT teams at our partner organizations Windsor Regional Hospital and Chatham-Kent Health Alliance (CKHA). Lastly, the trainees completed two in-house orientation shifts at ESHC with either a Critical Care Nurse Practitioner or a Regional Critical Care educator.
CCOT activations were initiated when a patient meets a trigger corresponding with significant variation in a normal vital sign parameter, any clinical sign of distress such as threatened airway or altered level of consciousness from baseline. In addition to these typical standard triggers, we included an elevated NEWS2 score [13] of equal or greater than seven as an independent trigger for CCOT activation. The team intervened in events involving concerns for all inpatients areas or those in the ED awaiting transfer to inpatient beds. Following the initial consultation, the CCOT monitored these patients for 48 hours to ensure their stability and provide ongoing support. Additionally, the CCOT continued to follow patients after their transfer from the ICU to monitor their recovery, prevent unnecessary ICU readmissions, and mitigate the risk of clinical deterioration.
Data Collection
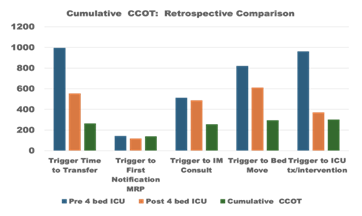
The data (chart review) collection period for RN-led nighttime CCOT (7:00 p.m. to 7:00 a.m., seven days a week) was from April 2024 to January 2025. As for the daytime CCOT (8:00 am to 4:00 pm, Monday through Friday which were supported by virtual consultations from Intensivists at Windsor Regional Hospital (WRH) privileged at our organization), the data collection period was from July 2024 to January 2025. To evaluate staff experiences and perceptions of CCOT, an online Normalization Measure Development (NoMAD) questionnaire [14] was conducted three months after the initial role out of the program. The NoMAD questionnaire was emailed out to inpatient and ED bedside nursing staff. This questionnaire consisted of questions to assess the understanding and attitudes of the CCOT program in general and their thoughts on the day and nighttime processes. Moreover, two independent retrospective chart audits of all ICU admissions before and after the expansion of ESHC’s ICU in 2023 were conducted. This data was analyzed separately to avoid any bias introduced by the expansion of critical care beds (initially two, then four) likely enhancing critical care access independent from the CCOT services. Specific data metrics were analyzed during chart audits, focusing on comparing the time when a patient first showed signs of deterioration (“trigger”) with various metrics along the continuum of response. These metrics included 1) the time stamp of the patient’s primary physician/Most Responsible Physician (MRP) was informed of the signs of deterioration, 2) time stamp of the internal medicine (IM) consult was requested, 3) the timing of the patient’s transfer to the ICU, and 4) the time it took to physically move the patient to the ICU bed and subsequent receipt of ICU treatment.
Results
The NoMAD questionnaire was completed by 49 participants, reporting a good understanding of the CCOT program (88.1%). Around 82% of participants recognized the program's value and how it positively affected their work. Moreover, 90% felt that the program was worthwhile, and 10% disagreed or were neutral. In addition, the overall satisfaction rate of the CCOT program was collected from each participant (mean score = 7.48 (± 1.97), with a maximum rating of 10 and a minimum rating of three. A few participants also provided barriers
Discussion
The failure to recognize and to act upon early warning signs of deterioration leads to devastating results. CCOT services have thus been introduced worldwide to detect these signs and prompt mobilization of critical care resources for at-risk patients. Multiple studies have demonstrated the value of utilizing CCOT in caring for critically ill and deteriorating patients and supporting the collaboration of healthcare professionals [5-8]. However, there is a lack of evidence of the use of CCOT in rural Ontario hospitals. Our study examined the perceptions of hospital staff, prevention of unwarranted ICU transfers, and reduction in several trigger metrics following the implementation of daytime virtual intensivist-led and nighttime RN-led CCOT programs. The NoMAD questionnaire revealed a generally positive perception of the use and benefit of the CCOT program at ESHC by the hospital staff, indicating the need for such initiative at rural settings. Similarly, survey responses from CCOT-RNs suggested that their involvement helped to avert unnecessary transfers to the ICU, an important observation, suggesting a reduced workload of ICU staff limiting the number of patients admitted to the ICU.
Moreover, a retrospective chart review revealed significant reductions in the time it takes to place a transfer order to the ICU (49.5%), move a patient to a critical care bed (61.9%), and receive the first intervention in the ICU (37.3%). These reductions directly demonstrate the effectiveness of CCOT services in expediting patient orders and ultimately improving the quality of care provided to deteriorating patients echoing contemporary studies [7,8]. This study had several limitations. For example, 97 ICU transfers did not involve CCOT from July 2024 to December 2024, undermining the impact of CCOT on trigger matrix. We believe the impact would have been higher if the program ran seamlessly. This interruption was due to a nursing staff shortage for the night shifts and weekend hours for the day shifts. Due to the staffing issue with recruiting a straight nighttime position and coverage for vacant nights, there may have been missed opportunities to assess the impact of CCOT. Another limitation expressed by participants is that the CCOT-RNs were not trained in specific areas, such as the obstetrics, therefore their involvement in obstetric emergencies was perceived to be limited to providing only basic support. Additionally, ESHC implemented a slightly different trigger, the NEWS2 score, compared to CCOTs at other institutions. Thus, full adaptation to this trigger was difficult and may have contributed to skewed data. Nevertheless, further training in critical care skills for specific populations and NEWS2 scores may help mitigate these issues.
Conclusion
It is clear that CCOT in our facility had a positive impact on staff in terms of their perceptions in trigger response times and improved patient care through identifying early warning signs of deterioration. This pilot study in a rural Ontario hospital exemplifies the need to implement a 24/7 program at ESHC. Additional research on similar settings or a longer implementation period may contribute new knowledge to healthcare research.
References
- Albutt A, O'Hara J, Conner M, et al. Involving patients in recognising clinical deterioration in hospital using the Patient Wellness Questionnaire: A mixed-methods study. J Res Nurs 25 (2020): 68-86.
- Chen J, Bellomo R, Flabouris A, et al. Delayed emergency team calls and Associated Hospital Mortality: A Multicenter Study. Crit Care Med 43 (2015): 2059-2065.
- National Guideline Centre (UK). Emergency and acute medical care in over 16s: service delivery and organisation. London: National Institute for Health and Care Excellence (NICE); March (2018).
- Riley B, Faleiro R. Critical care outreach: Rationale and development. British J Anaesth 1 (2001).
- Fernando SM, Fox-Robichaud AE, Rochwerg B, et al. Prognostic accuracy of the Hamilton Early Warning Score (HEWS) and the National Early Warning Score 2 (NEWS2) among hospitalized patients assessed by a rapid response team. Crit Care 23 (2019): 60.
- Brown A, Ballal A, Al-Haddad M. Recognition of the critically ill patient and escalation of therapy. Science Direct 22 (2021): 671-675.
- Escobar GJ, Liu VX, Schuler A, et al. Automated Identification of Adults at Risk for In-Hospital Clinical Deterioration. N Engl J Med 383 (2020): 1951-1960.
- Tillmann BW, Klingel ML, McLeod SL, et al. The impact of delayed critical care outreach team activation on in-hospital mortality and other patient outcomes: a historical cohort study. Can J Anaesth 65 (2018): 1210-1217.
- Buist MD, Moore GE, Bernard SA, et al. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ 324 (2002): 387-390.
- Cuthbertson BH. The impact of critical care outreach: Is there one? Crit Care 11 (2007): 179.
- Critical Care Services Ontario. Ontario critical care plan: 2018-2021 (2018).
- BIG Healthcare. Erie Shores HealthCare Benchmarking (2015).
- Smith GB, Prytherch DR, Meredith P, et al. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 84 (2013): 465–70.
- May C, Rapley T, Mair FS, et al. Normalization Process Theory On-line Users’ Manual, Toolkit and NoMAD instrument (2015).


 Impact Factor: * 6.2
Impact Factor: * 6.2 Acceptance Rate: 76.33%
Acceptance Rate: 76.33%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 