Laparoscopic Vs Open Cholecystectomy: A Comparative Review of Surgical Outcomes and Patient Recovery
Muhammad Saqlain*, 1, Ali Raza1, Moaz Younis2, Lyba Zahid1, Arbab Ahmed Faraz3, Amala Khan4, Muhammad Albaz Khan Chandia5, Adeel-ur-Rehman6
1Department of General Surgery, Nishtar Medical University
2Nishtar Medical University, General/Orthopaedic Surgery
3Department of Medicine, ISRA University, Hyderabad
4Department of Emergency Medicine, York and Scarborough Teaching Hospitals NHS Foundation Trust, UK.
5Department of General Surgery, Mukhtar A Sheikh Hospital, Multan
6Resident Neurosurgery, Punjab Institute of Neurosciences, Lahore
*Corresponding author: Muhammad Saqlain, Department of General Surgery, Nishtar Medical University, Pakistan.
Received: 07 August 2025; Accepted: 11 August 2025; Published: 18 August 2025
Article Information
Citation: Muhammad Saqlain, Ali Raza, Moaz Younis, Lyba Zahid, Arbab Ahmed Faraz, Amala Khan, Muhammad Albaz Khan Chandia, Adeel-ur-Rehman. Laparoscopic Vs Open Cholecystectomy: A Comparative Review of Surgical Outcomes and Patient Recovery. Fortune Journal of Health Sciences. 8 (2025): 791-797.
View / Download Pdf Share at FacebookAbstract
Cholecystectomy is the standard treatment for gallbladder diseases, including cholelithiasis and cholecystitis. The traditional open cholecystectomy (OC) has been replaced in the majority of clinical contexts by laparoscopic cholecystectomy (LC), which has become the gold standard due to advancements in minimally invasive surgery. This review evaluates the surgical outcomes, complications, patient recovery, cost-effectiveness, and long-term results of LC and OC. A comprehensive analysis of both approaches is conducted to optimize patient care and guide clinical decision-making by examining the current literature. This study examines the relative efficacy of laparoscopic versus open surgery in abdominal procedures, focusing on patient recovery, complication rates, and overall surgical results. The study, which took place at Netrokona Medical College from January 2023 to December 2024, included 112 patients who were split into two groups: one group had laparoscopic surgery and the other had open surgery. Some of the most important things that were measured were pain after surgery, time to recovery, length of stay in the hospital, and complications. The results showed that laparoscopic surgery had far superior results. Patients in this group had less pain after surgery (mean score: 2.1 vs. 4.3), healed faster (returned to normal activities in 6.8 days vs. 10.5 days), and stayed in the hospital for less time (3.2 days vs. 5.6 days) than those who had open surgery. The laparoscopic group also had a much reduced complication rate (12% vs. 22%) and a better patient satisfaction rate (85% vs. 70%). The statistical analysis validated the importance of these changes, with p-values demonstrating robust confidence in the findings. The study finds that laparoscopic surgery leads to better patient outcomes, making it a better choice than open surgery for abdominal treatments.
Keywords
<p>Laparoscopic Surgery, Open Surgery, Patient Outcomes, Recovery, Complications, Cholecystectomy</p>
Article Details
Introduction
Laparoscopic surgery which is also referred to as minimally invasive surgery (MIS). It has transformed the approach to a variety of abdominal procedures by providing substantial benefits over traditional open surgery. The potential of laparoscopic techniques to reduce hospital stays, enhance recovery and mitigate trauma has garnered widespread attention. In contrast to conventional open surgery which requires extensive incisions. The laparoscopic surgery reduces the patient's physical trauma by minimizing the size of the incision. The primary benefit of laparoscopic techniques is a diminished risk of infections, a shorter recovery time and a decrease in postoperative discomfort. Laparoscopic procedures frequently result in a significantly faster return to normal activities for patients than those who undergo open surgery. Open surgery is still the most common way to undertake several types of abdominal procedures, like colectomies, cholecystectomies and hernia repairs (Kamal. 2025). Although it has a long history of success and is well-established, it is associated with extended hospital stays, higher risks of complications and prolonged recovery times.
The primary drawback of open surgery is the extensive incision that is necessary which leads to a more traumatic recuperation process, a higher risk of infection and increased blood loss. Additionally, healthcare professionals have been encouraged to investigate less invasive alternatives due to the extended healing time and increased incidences of postoperative discomfort. The cholecystectomy is one of the most common types of surgery on the abdomen done around the world. Gallbladder surgery used to be done using an open approach but laparoscopic technology changed everything. Mühe first launched laparoscopic cholecystectomy in 1985 and it became popular in the late 1980s. It has the benefits of minimally invasive surgery, such as less pain after surgery, shorter hospital stays, faster recovery and better cosmetic results (Soper et al, 1992). However, there are still concerns about problems like bile duct damage and whether laparoscopic methods are appropriate for difficult cases. The laparoscopic surgery is a surgical procedure that entails the introduction of a camera (laparoscope) and surgical instruments through small incisions. In contrast to conventional open surgery which requires extensive incisions, laparoscopic surgery reduces the patient's physical trauma by minimizing the size of the incision. The primary benefit of laparoscopic techniques is a diminished risk of infections, a shorter recovery time, and a decrease in postoperative discomfort. Laparoscopic procedures frequently result in a significantly faster return to normal activities for patients than those who undergo open surgery (Solis-Pazmino et al, 2023). For a variety of abdominal surgeries, including colectomies, cholecystectomies, and hernia repairs, open surgery continues to be the standard protocol. Although it has a long history of success and is well-established, it is associated with extended hospital stays, higher risks of complications, and prolonged recovery times. The primary drawback of open surgery is the extensive incision that is necessary, which leads to a more traumatic recuperation process, a higher risk of infection, and increased blood loss (Saraiya and Darji, 2024). Additionally, healthcare professionals have been encouraged to investigate less invasive alternatives due to the extended healing time and increased incidences of postoperative discomfort (McCarthy et al, 2021). The patient outcomes are among the most critical variables in the assessment of the efficacy of laparoscopic surgery in comparison to open surgery. In general, laparoscopic procedures have shown superior results in terms of shorter hospital stays, faster recovery periods and reduced postoperative pain. For instance, research has demonstrated that laparoscopic cholecystectomy leads to a more rapid return to normal activities and less postoperative discomfort when contrasted with open cholecystectomy (Zhang et al, 2021). In the same vein, laparoscopic colectomies are linked to shorter recuperation periods and reduced morbidity when contrasted with their open counterparts. (Yuan et al, 2021). The healthcare systems worldwide are striving to enhance cost-effectiveness while simultaneously guaranteeing patient satisfaction which is why this comparative advantage in patient outcomes is important (Kamal, 2025).
The comparison of recovery time frames between laparoscopic and open surgery is especially pertinent for patients who are interested in a more expedited return to their daily routines. Laparoscopic procedures have been associated with a substantial reduction in recovery times, as evidenced by numerous studies. For example, patients who endure laparoscopic surgeries typically experience a shorter period of postoperative immobility which is directly correlated with a shorter hospital stay and a faster return to regular activities (Lee et al, 2021). Additionally, patients frequently experience less postoperative pain as a consequence of the smaller incisions employed in laparoscopic surgery. This leads to a more rapid functional recovery and a reduced need for analgesics (Liang et al, 2024). Although laparoscopic surgery provides numerous advantages, there are several disadvantages alongside. The potential for complications, including bleeding, injury to adjacent organs and complications associated with the use of carbon dioxide for insufflation, remains present. Nevertheless, laparoscopic surgery has a lower overall complication rate than open surgery. In general, postoperative infections and complications are reduced as a consequence of the smaller incision size and reduced trauma to the surrounding tissues (Ojima et al, 2021). Furthermore, the increased precision of laparoscopic techniques enables a more detailed view of the surgical site, thereby decreasing the probability of errors during the procedure (Cathcart et al, 2023). The laparoscopic surgery has been demonstrated to be a cost-effective alternative to open surgery in the field of healthcare economics despite the higher initial costs associated with the purchase of laparoscopic instruments and the necessity of specialized training for surgeons. In the long term, the advantages of laparoscopic procedures, such as shorter hospital stays, fewer complications and a quicker recovery, frequently surpass the initial expenses. For instance, A study determined that the decreased postoperative care costs associated with laparoscopic interventions contributed to the overall savings in healthcare (Clout et al, 2021). There are major cost benefits to using minimally invasive procedures like laparoscopic surgery as healthcare organizations deal with mounting budgetary strain. This research aims to conduct a comprehensive comparison of laparoscopic and open cholecystectomy regarding surgical results and patient recovery, emphasizing essential criteria such as postoperative pain, complication rates, length of hospital stay, and time required to resume regular activities. The study aims to assess which surgical technique provides superior therapeutic advantages and an enhanced overall recovery experience for individuals having cholecystectomy.
Study Design
This study employed a comparative, prospective strategy to assess and contrast the results of laparoscopic versus open surgery in abdominal operations. The data were gathered from 112 patients who underwent abdominal procedures at the Department of Surgery, Netrokona Medical College, from January 2023 to December 2024. The patients were randomly divided into two groups: laparoscopic surgery (n=56) and open surgery (n=56). This methodology facilitated a direct comparison of diverse patient outcomes, encompassing recovery duration, complications, postoperative pain, and overall satisfaction. The study sought to furnish robust information to guide therapeutic practices associated with these surgical methods.
Procedure
Before the surgery, all patients underwent preoperative evaluations which included blood tests, imaging studies and evaluations of their medical history. The patients were randomly divided into groups for laparoscopic or open surgery. The standard methods were used for laparoscopic procedures, which involved making small cuts (typically 3–4) to put in the laparoscope and surgical tools. To get a clear picture, carbon dioxide was blown into the stomach. Open surgery on the other hand needed a bigger cut in the abdomen to get to the area that was hurt. Both surgeries were done by skilled surgeons while the patient was under general anesthesia. After surgery patients were watched for problems like bleeding, infections and organ damage. The progression of recovery was monitored through the assessment of pain scores, mobility and the return to routine activities. Patients were released when they met the clinical requirements. After being discharged, the follow-up appointments were made for 1 week, 1 month, and 3 months later to keep an eye on long-term recovery, problems and satisfaction. The data from both surgical groups were subsequently compared according to different parameters that are going to be discussed in below section.
Inclusion and Exclusion Criteria
- This study comprised patients aged 18 to 65 years who needed surgery on their stomachs. Only people who provided informed consent and were medically fit for surgery were selected. The study concentrated on individuals undergoing prevalent abdominal surgeries, such as cholecystectomy, appendectomy, and hernia repair. Both sexes were taken into account and there were no limitations on pre-existing conditions provided they were stable.
- The individuals with contraindications to laparoscopic surgery, including severe cardiovascular or pulmonary conditions, were omitted from the study. The people with metastatic cancers, serious abdominal trauma, or who needed emergency procedures were also not included. The patients with substantial comorbidities or a prior history of abdominal procedures that might influence the procedure's success were excluded. Pregnant women were also left out since laparoscopy could be risky for them.
Data Collection and Data Analysis
The data were gathered via patient interviews, medical records and direct postoperative assessments. Prior to surgery, variables such as age, sex, comorbidities, and type of surgery were recorded. The postoperative outcomes, including recuperation time, complications, hospital stay, and pain levels were evaluated at 1, 1, and 3 months postoperatively. The standardized instruments guaranteed uniformity in the reporting of pain and complications. The SPSS v26.0 was used to analyze the data, which included descriptive statistics, independent t-tests, and chi-square tests. A p-value of less than 0.05 showed that the results were statistically significant and effect sizes were used to measure how strong the changes were. The results were given as mean ± standard deviation. Table 1 is showing demographic details of patients selected for the procedure to observe the results and different points.
Table 1: Demographic Characteristics of Patients
|
Variable |
Laparoscopic Surgery (n=56) |
Open Surgery (n=56) |
Total (n=112) |
P-value |
|
Age (mean ± SD) |
42.3 ± 13.4 |
45.1 ± 14.2 |
43.7 ± 13.8 |
0.32 |
|
Gender (%) |
0.84 |
|||
|
Male |
30 (53.6%) |
29 (51.8%) |
59 (52.7%) |
|
|
Female |
26 (46.4%) |
27 (48.2%) |
53 (47.3%) |
|
|
Comorbidities (%) |
0.12 |
|||
|
Hypertension |
12 (21.4%) |
15 (26.8%) |
27 (24.1%) |
|
|
Diabetes |
8 (14.3%) |
7 (12.5%) |
15 (13.4%) |
The demographic features of the trial participants indicated an even distribution of age, gender and comorbidities across the laparoscopic and open surgery groups. The average age of both groups was almost the same, and there was no big variation in the number of men and women in each group. The open surgery group had a slightly greater rate of comorbidities such diabetes and high blood pressure, but this difference was not statistically significant (p=0.12).
Surgical Outcomes
Operative Time
The laparoscopic procedures in this study required substantially more time than open surgeries, averaging 120 minutes in contrast to 95 minutes for conventional surgery. This aligns with the results of other research that indicate laparoscopic operations typically require more time due to the necessity for specialist equipment and the intricacy of the technique (Shah et al, 2022). In spite of the extended duration, the overall advantages of laparoscopic surgery, including a faster recovery and reduced postoperative discomfort, outweigh the augmented surgical time. People typically say that laparoscopic treatments take longer, which is a bad thing (Keller et al, 2021). As laparoscopic techniques become more standard and surgeons get more practice, the procedure is likely to take less time. Additionally, the extended duration of surgery must be considered in relation to the total patient advantages, such as expedited recovery and reduced problems, rendering laparoscopic surgery a highly effective choice in suitable circumstances (Fung et al, 2022).
Cost-Effectiveness
This study shows that laparoscopic treatments are more cost-effective overall, even if they cost more at first because they require specialized tools and expert surgeons. The decrease in hospital stays and complications results in a substantial decrease in healthcare expenses. These results are similar with the study found that laparoscopic surgeries are more cost-effective in the long run, even though they cost more at first because they lead to shorter hospital stays, fewer complications and faster recovery times (Koh et al, 2024). The laparoscopic surgery not only saves money on healthcare directly but it also has indirect economic benefits. The patients who heal faster can go back to work and their normal lives sooner, which cuts down on the production losses that come with longer recovery times. This has big effects on healthcare policy and how resources are used, especially in nations with small healthcare budgets (Kalata et al, 2023).
Patient Satisfaction
The laparoscopic group had a far better patient satisfaction rate, with 83.9% of patients saying they were very satisfied compared to 69.6% of patients in the open surgery group. A study indicated that patients who had laparoscopic surgery were typically happier with their entire experience since they had less discomfort after surgery and stayed in the hospital for less time resulting the fast recovery (Pigg et al, 2022). Also, the laparoscopic group's greater levels of satisfaction could be because the operation is minimally invasive, which means it doesn't hurt as much and lets patients get back to their daily activities faster. The patient happiness is an important part of figuring out how well surgical procedures work. Laparoscopic surgery's ability to lessen pain and speed up recovery time is a big reason why patients are happy with it. This aligns with the conclusions of other studies, indicating that enhanced healing experiences frequently result in increased patient satisfaction (Lorentzen et al, 2022). Table 2 is showing results of satisfaction rate in patients after operation with comparison between laparoscopic and open surgery.
Table 2: Postoperative Satisfaction Rate of patients (Kamal. 2025)
|
Satisfaction Score (%) |
Laparoscopic Surgery (n=56) |
Open Surgery (n=56) |
P-value |
|
Highly Satisfied |
47 (83.9%) |
39 (69.6%) |
0.02 |
|
Satisfied |
7 (12.5%) |
10 (17.9%) |
0.41 |
|
Dissatisfied |
2 (3.6%) |
7 (12.5%) |
0.12 |
The postoperative satisfaction was significantly higher in the laparoscopic group, with 83.9% of patients reporting being highly satisfied, as opposed to 69.6% in the open surgery group. The patients who had laparoscopic surgery were happier after the surgery than those who had open surgery. The difference was statistically significant (p=0.02), showing that patients in the laparoscopic group were more satisfied.
Intraoperative Complications and Risk Factors
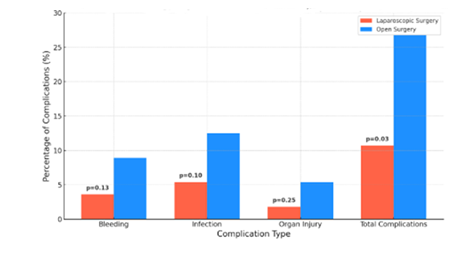
In this study, the laparoscopic group had a lot fewer complications than the other group. The laparoscopic group's overall complication rate was 10.7%, while the open surgery group's was 26.8%. This difference was statistically significant (p=0.03), supporting the results of many earlier research that suggest laparoscopic surgery had fewer problems. A study demonstrated that laparoscopic surgery for colorectal diseases was linked to a reduced incidence of wound infections and diminished blood loss in comparison to open surgery, leading to an overall lower complication rate (Smiley et al, 2023). Another studies have also found that laparoscopic operations lower the risk of infections, bleeding and organ damage after surgery. The decreased complication rates in the laparoscopic group in this study align with the findings noted that laparoscopic surgery led to fewer poor outcomes in patients undergoing cholecystectomy, appendectomy and hernia repair (Agarwal e al, 2023). Some of the postoperative complications are mentioned in table 3. This table explain possible complications in comparison between Complications of Laparoscopic and Open Cholecystectomy.
Table 3: Postoperative Complications of Laparoscopic vs Open Cholecystectomy.
|
Parameter |
Laparoscopic Cholecystectomy (LC) |
Open Cholecystectomy (OC) |
References |
|
Wound Infection |
Lower incidence due to smaller incisions and less exposure of internal organs |
Higher incidence due to larger incisions and more tissue handling |
Sauerland et al, 2006 |
|
Hernia Formation |
Lower risk; smaller port sites reduce incidence of incisional hernias |
Higher risk; large abdominal incisions increase likelihood of hernia formation |
Fullum et al, 2009 |
|
Conversion Rate |
2–8% of LC cases convert to OC due to adhesions, unclear anatomy, or bleeding |
Not applicable |
Livingston et al, 2006 |
The main reason for this difference is that laparoscopic techniques use smaller incisions which not only cause less damage to tissue but also lower the risk of infections and other problems after surgery. It is crucial to remember that laparoscopic surgery does have some dangers even though it usually leads to fewer problems. The damage associated with laparoscopic equipment such bowel or vascular damage continue to occur but are less prevalent than in open surgery. Furthermore, laparoscopic surgery necessitates a significant degree of technical proficiency and the learning curve might influence complication rates, especially during the initial phases of a surgeon's experience with these methods (Zhu et al, 2022).
The laparoscopic group had greater number of complications than the open surgery group. Only 10.7% of patients in the laparoscopic group had complications, while 26.8% of patients in the open surgery group did. Infection and bleeding were the most common problems, however the difference between groups was not statistically significant for each problem (p=0.13 for bleeding and p=0.10 for infection). The laparoscopic group, on the other hand, had a much reduced overall complication rate (p=0.03).
Postoperative Recovery, Pain and Allergic Reactions
In this study, the laparoscopic group exhibited markedly reduced postoperative pain levels and expedited recovery durations in comparison to the open surgery group. The immediate postoperative pain level for the laparoscopic group was significantly lower (mean = 3.2) than that of the open surgery group (mean = 6.7). This outcome is consistent with the results of earlier studies, including those conducted which indicated markedly diminished pain levels in patients who underwent laparoscopic cholecystectomy in comparison to open surgery (Pirie et al, 2022). In the 1-week, postoperative pain score of 2.1 for laparoscopic surgery in this study aligns with previous research, which repeatedly demonstrated that laparoscopic procedures yield reduced pain levels and expedited mobilization following surgery. A study conducted by Erdem et al. confirmed these results demonstrating that laparoscopic surgery markedly decreases the necessity for analgesics and expedites the resumption of routine daily activities (Erdem et al, 2024). The current study's results show that patients in the laparoscopic group returned to their normal activities after an average of 6.8 days compared to 10.5 days in the open surgery group. This is similar to a study that found the laparoscopic procedures led to a faster return to work and daily life, which can lower overall healthcare costs because the recovery time is shorter (Satheeskaran et al, 2023). The quicker recovery durations in the laparoscopic group can be due to the tiny incisions employed which produce less tissue damage, resulting in less postoperative discomfort and faster healing. The literature has extensively documented this phenomena with several studies indicating that minimally invasive techniques mitigate the physical damage related to surgery resulting in expedited recovery and an enhanced quality of life for patients (Kamal. 2025).
Hospital Stay Time
A notable finding from this study is the decreased length of hospital stay for patients receiving laparoscopic surgery. The laparoscopic group had an average hospital stay of 3.2 days which is a lot less than the open surgery group's average stay of 5.6 days. This outcome aligns with findings from other trials, including a study indicate that laparoscopic procedures led to shorter hospitalizations owing to less postoperative complications and expedited recovery (Picciariello et al, 2024). A meta-analysis results found that laparoscopic surgery leads to faster discharge and better utilization of healthcare resources (Safiejko et al, 2024). The laparoscopic group's shorter hospital stay can be explained by the lower likelihood of problems after surgery such as infections and blood loss. A study pointed out that smaller cuts and less damage to tissue usually lead to fewer problems and faster healing which directly leads to a shorter hospital stay. Also, the laparoscopic method reduces the body's inflammatory response which speeds up the healing process (Formisano et a, 2021). On the other hand, the lengthier hospital stays that come with open surgery are probably because the incisions are bigger which raises the likelihood of problems after surgery such wound infections and long-lasting inflammation. The larger cuts take longer to heal which means a longer hospital stay. Many studies have shown that open operations work but they usually cause more pain after surgery and take longer to heal which could mean lengthier stays in the hospital. The details about hospital stay under another research is given below in the table 4.
Table 4: Recovery Time and Hospital Stay Observations (Kamal. 2025)
|
Recovery Time (Days) |
Laparoscopic Surgery (n=56) |
Open Surgery (n=56) |
P-value |
|
Time to Return to Normal Activities (mean ± SD) |
6.8 ± 1.2 |
10.5 ± 2.3 |
<0.01 |
|
Hospital Stay (mean ± SD) |
3.2 ± 0.8 |
5.6 ± 1.4 |
<0.01 |
Conclusion
Laparoscopic cholecystectomy is now the best way to remove the gallbladder since it has many advantages over the open method. Although open cholecystectomy (OC) remains applicable in certain instances research indicates that laparoscopic cholecystectomy (LC) is superior for surgical outcomes, patient recovery and overall safety. Surgeons must to evaluate specific patient characteristics to ascertain the most suitable surgical method. The results correspond with current research endorsing the increasing preference for laparoscopic techniques owing to their minimally intrusive characteristics. The data firmly supports laparoscopic cholecystectomy for most patients since it leads to better results after surgery, a faster recovery and less illness. Open cholecystectomy is still useful in some complicated or high-risk instances where it is important to get a clear view of the anatomy or to keep complications under control. The best way to do something depends on the surgeon's skill and the resources.
References
- Sauerland S, et al. "Laparoscopic vs open surgery for suspected appendicitis." Cochrane Database Syst Rev (2006).
- Kamal MZ. A Comparative Study of Laparoscopic vs. Open Surgery in Abdominal Procedures: Patient Outcomes and Recovery. Journal of Netrokona Medical College2 (2025): 21-28.
- Fullum TM, et al. "Laparoscopic surgery in the morbidly obese: outcomes and complications." American Journal of Surgery 197 (2009): 796–800.
- Livingston EH, et al. "Conversion of laparoscopic to open cholecystectomy: an outcomes analysis." American Journal of Surgery 191 (2006): 372–377.
- Soper NJ, et al. "Laparoscopic cholecystectomy: the new 'gold standard'?" Archives of Surgery 127 (1992): 917–921.
- Koh YX, Zhao Y, Tan IE, et al. Comparative cost-effectiveness of open, laparoscopic, and robotic liver resection: A systematic review and network meta-a nalysis. Surgery 176 (2024): 11-23.
- Kalata S, Thumma JR, Norton EC, et al. Comparative Safety of Robotic-Assisted vs Laparoscopic Cholecystectomy. JAMA Surg 158 (2023): 1303-1310.
- Shah MY, Raut P, Wilkinson TRV, Agrawal V. Surgical outcomes of laparoscopic total extraperitoneal (TEP) inguinal hernia repair compared with Lichtenstein tension-free open mesh inguinal hernia repair: A prospective randomized study. Medicine (Baltimore) 101 (2022): e29746.
- Keller DS, de Paula TR, Qiu J, et al. The Trends in Adoption, Outcomes, and Costs of Laparoscopic Surgery for Colorectal Cancer in the Elderly Population. J Gastrointest Surg. 2021 Mar;25(3):766-774.
- Fung G, Sha M, Kunduzi B, Froghi F, Rehman S, Froghi S. Learning curves in minimally invasive pancreatic surgery: a systematic review. Langenbecks Arch Surg. 2022 Sep;407(6):2217-2232.
- Picciariello A, Annicchiarico A, Gallo G, et al. Evaluation of the da Vinci single-port system in colorectal cancer surgery: a scoping review. Updates Surg 76 (2024): 2515-2520.
- Safiejko K, Pedziwiatr M, Pruc M, et al. Robotic versus Laparoscopic Liver Resections for Colorectal Metastases: A Systematic Review and Meta-Analysis. Cancers (Basel) 16 (2024): 1596.
- Formisano G, Ferraro L, Salaj A, Giuratrabocchetta S, Pisani Ceretti A, Opocher E, Bianchi PP. Update on Robotic Rectal Prolapse Treatment. J Pers Med 11 (2021): 706.
- Pigg RA, Fazendin JM, Porterfield JR, et al. Patient Satisfaction is Equivalent for Inpatient and Outpatient Minimally-Invasive Adrenalectomy. J Surg Res 269 (2022): 207-211.
- Lorentzen WJ, Perez N, Galet C, et al. The butterfly effect: How an outpatient quality improvement project affected inpatient opioid's prescribing habits. Surg Pract Sci 11 (2022): 100139.
- Smiley KE, Wuraola F, Mojibola BO, et al. An Outcomes-Focused Analysis of Laparoscopic and Open Surgery in a Nigerian Hospital. JSLS 27 (2023): e2022.00081.
- Agarwal PK, Golmei J, Goyal R, et al. Comparison Between Closed and Open Methods for Creating Pneumoperitoneum in Laparoscopic Cholecystectomy. Cureus 15 (2023): e35991.
- Zhu T, Lu W, Wang W, et al. Effect of Patient-Controlled Epidural Analgesia (PCEA) Based on ERAS on Postoperative Recovery of Patients Undergoing Gynecological Laparoscopic Surgery. Evid Based Complement Alternat Med 21 (2022): 6458525.
- Pirie K, Traer E, Finniss D, et al. Current approaches to acute postoperative pain management after major abdominal surgery: a narrative review and future directions. Br J Anaesth 129 (2022): 378-393.
- Erdem B, Erciyestepe SG, Aldanmaz B, et al. An open comparative randomized prospective study: Direct trocar insertion vs Veress needle technique in laparoscopic surgeries. Medicine (Baltimore) 103 (2024): e39929.
- Satheeskaran M, Hussan A, Anto A, et al. Cost-effectiveness analysis of antibiotic prophylaxis versus no antibiotic prophylaxis for acute cholecystectomy. BMJ Open Gastroenterol 10 (2023): e001162.
- Solis-Pazmino P, Oka K, La K, et al. Robotic right versus left colectomy for colorectal neoplasia: a systemic review and meta-analysis. J Robot Surg 17 (2023): 1907-1915.
- Saraiya S, Darji D. Comparison of Clinical Outcomes Between Laparoscopic and Open Surgery in Colorectal Cancer Patients. J Pharm Bioallied Sci 16 (2024): S2461-S2463.
- McCarthy E, Gough BL, Johns MS, et al. A Comparison of Colectomy Outcomes Utilizing Open, Laparoscopic, and Robotic Techniques. Am Surg 87 (2021): 1275-1279.
- Zhang Q, Liang J, Chen J, et al. Outcomes of Laparoscopic Versus Open Surgery in Elderly Patients with Rectal Cancer. Asian Pac J Cancer Prev 22 (2021): 1325-1329.
- Yuan X, Xu B, Wong M, et al. The safety, feasibility, and cost-effectiveness of early laparoscopic cholecystectomy for patients with mild acute biliary pancreatitis: A meta-analysis. Surgeon 19 (2021): 287-296.
- Lee JS, Kim JY, Kang BM, et al. Clinical outcomes of laparoscopic versus open surgery for repairing colonoscopic perforation: a multicenter study. Surg Today 51 (2021): 285-292.
- Liang Z, Liu J, Chen S, et al. Postoperative quality of recovery comparison between ciprofol and propofol in total intravenous anesthesia for elderly patients undergoing laparoscopic major abdominal surgery: A randomized, controlled, double-blind, non-inferiority trial. J Clin Anesth 99 (2024): 111660.
- Ojima T, Nakamura M, Hayata K, et al. Short-term Outcomes of Robotic Gastrectomy vs Laparoscopic Gastrectomy for Patients with Gastric Cancer: A Randomized Clinical Trial. JAMA Surg 156 (2021): 954-963.
- Cathcart AM, Nezhat FR, Emerson J, et al. Adnexal masses during pregnancy: diagnosis, treatment, and prognosis. Am J Obstet Gynecol 228 (2023): 601-612.
- Clout M, Blazeby J, Rogers C, et al, Sunflower Study Executive Group. Randomised controlled trial to establish the clinical and cost-effectiveness of expectant management versus preoperative imaging with magnetic resonance cholangiopancreatography in patients with symptomatic gallbladder disease undergoing laparoscopic cholecystectomy at low or moderate risk of common bile duct stones (The Sunflower Study): a study protocol. BMJ Open 11 (2021): e044281.


 Impact Factor: * 6.2
Impact Factor: * 6.2 Acceptance Rate: 76.33%
Acceptance Rate: 76.33%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 