Myths of surgery and ‘The Pandemic’: A Surgeons Dilemma
Abdul Rehman*, Muhammad Fahd Shah, Muhammad Toqeer Zahid, Hamza Shahid, Verda Baig, Masood Ur Rehman, Shahid Khattak, Aamir Ali Syed
Department of Surgical Oncology, Shaukat Khanum Memorial Cancer Hospital and Research Centre, Johar town, Lahore, Pakistan
*Corresponding Author: Dr. Abdul Rehman, Department of Surgical Oncology, Shaukat Khanum Memorial Cancer Hospital and Research Centre, Johar town, Lahore, Pakistan
Received: 22 April 2021; Accepted: 29 April 2021; Published: 07 May 2021
Article Information
Citation: Abdul Rehman, Muhammad Fahd Shah, Muhammad Toqeer Zahid, Hamza Shahid, Verda Baig, Masood Ur Rehman, Shahid Khattak, Aamir Ali Syed. Myths of surgery and ‘The Pandemic’: A Surgeons Dilemma. Journal of Surgery and Research 4 (2021): 263-269.
View / Download Pdf Share at FacebookAbstract
Objective: To study the outcomes of patients who underwent surgery for malignancies during the COVID 19 Pandemic.
Method: Patients who underwent oncological surgery from March to July 2020 were studied. COVID-PCR was done in all patients preoperatively. Those who tested positive were postponed for 2 weeks. Patients were followed for type of surgery, need of ICU admission, presence of COVID symptoms post operatively and development of complications. Total length of hospital stay was also recorded.
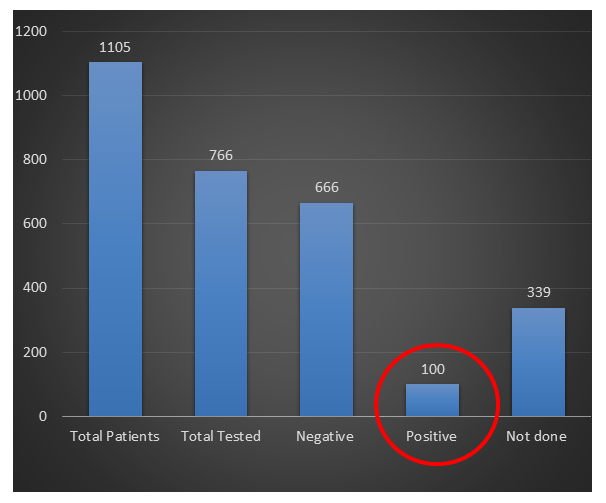
Results: A total of 1105 patients were operated from March to July 2020 for GI, HBP, Head & Neck, Urology, Gynaecological, Orthopaedics, Neurosurgical, Plastic Surgery and Cardio-thoracic cancers. Of these 339 patients were operated without any COVID testing. From April 2020, new hospital policies came into effect and every patient was required to undergo testing 48 hours before surgery. 766 patients underwent testing for COVID. 666 patients were negative and proceeded with surgery. 92 patients tested positive on routine screening and had their operation delayed for a period of 2 weeks. 8 patients who were operated in emergency had COVID infection but surgery was not delayed due to emergent nature of the procedure. When analysing the hospital stay of these 100 patients who tested positive there were only 10 patients who were admitted to COVID facility and there were only 3 mortalities that were attributable to COVID.
Conclusions: Operating on patients who are COVID positive didn’t lead to any additional morbidity and mortality. We recommend that all hospitals should resume their elective surgical lists.
Keywords
COVID-19, Safety of surgery, Laparoscopic Surgery
Article Details
1. Introduction
The 2020 Pandemic of COVID-19 has markedly affected the rules of play in every field even as minute as the interaction of human beings. Since the time the virus has gone blitz, every possible human to human interaction is brought to a minimum. The major brunt of which was faced by oncological patients needing surgical interventions. Specifically, the vast majority of the centres in the areas more severely hit by the pandemic had limited their surgical activities, according to specific recommendations for patient triage from international societies and independent research group [1-3].
Since the surgeons are the most exposed to the droplet infection contributing to its relentless spread. Severe acute respiratory syndrome (SARS)-Cov-2 has caused 63,641,374 infections worldwide as of December 1, 2020 results in severe or critical illness in 20-30% of cases and has a case-fatality rate ranging from 1.4% to 7.2% [4]. Indeed, the case-fatality rate of individuals >70 years of age has ranged from 8.0% to 22.5% [5,6]. A recent article published by our Chinese colleagues suggests that patients with cancer are more likely to be infected by the virus because of their immune-depressed state induced by their cancer, chemotherapy and surgery [7]. While dealing with such high probability of being affected with the virus; the health of patients as well as the professionals was at risk. Thus elective surgery in all forms was disbanded across the board in all surgical fraternity. But this came at a price. Oncology patients who were in dire need of surgery were deferred indefinitely. Contrary to the prevailing popular belief that undertaking surgical intervention carried more risk than benefits our institute devised a strategy to mitigate the risks. As we made progress in understanding the disease better, an attempt was made to make surgery possible again. We aimed at segregating the high risk and affected population by this scourge; re-scheduling of surgery at such a time that reduced the risk of infection and enabled to operate upon with-out causing unnecessary delay in treatment. This came with a high level of personal protection. It did had some amount of risk to it nonetheless a scheme to perform safe practice of surgery in the pandemic was designed. At Shaukat Khanum Memorial Cancer Hospital and Research Centre (SKMCH&RC) like the rest of the world all surgeries were stopped in the last week of March 2020. However since all our patients were cancer patients and we had referrals from all over the country it wasn’t acceptable that we stop our service for long. We devised special protocols, PPEs were procured and services were resumed in the 1st week of April. Here we share our experience of conducting surgery in the pandemic at Shaukat Khanum Memorial Cancer Hospital in Lahore.
3. Methodology
2.1 Patient Selection
Operations during the COVID outbreak were resumed in the 1st week of April. All the patients who underwent surgery during the period of March to July 2020 were included in the study. This included patients in the divisions of GI and Hepatobiliary, Urology, Head and Neck, Gynaecology, Neurosurgery, Orthopaedics, Plastic Surgery and Cardio-thoracic Surgery were included. The procedures were performed as elective or emergency for oncological reasons and performed as open, laparoscopic or endoscopically. All patients who underwent procedures under local anaesthesia were excluded. Initially surgery was resumed with the use of Personal Protective Equipment (PPEs) but universal covid testing wasn’t adopted for every patient as it wasn’t available. However as the tests became available all patients were required to get tested before surgery. This was a retrospective study with convenient sampling.
2.2 Data analysis and statistical methods
Calculations were performed with Statistical Package for the Social Sciences (SPSS 20) for Windows version 20 statistical software. Data was described using mean with minimum and maximum value for skewly distributed quantitative variables. For categorical variables, number of observations and percentages were reported. The study was complied with the SKMCH&RC guidelines on research involving human subjects.
2.3 Variables
Data was collected through hospital information system (HIS), electronic database of SKMCH&RC. Variables recorded were status of COVID-19 pre- and post-operatively, duration of surgery, post-operative ICU/HDU admission, post-operative development of COVID related symptoms, duration of admission in the hospital.
3. Results
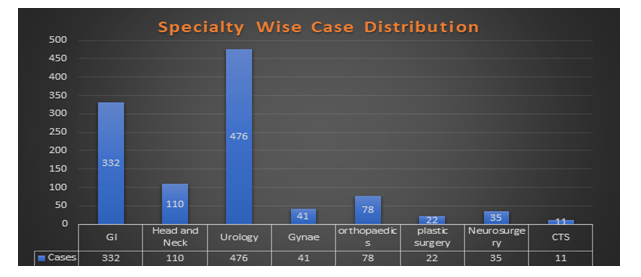
A total of 1105 patients who qualified for our selection criteria were operated between the months of March to July 2020. Among these patients 928 (84%) were operated electively while 177 (16%) were treated on emergent basis. The age ranged from 18-93 years with a mean age of 48 years with a SD of +16 years. The quantum of cases by each department included in the study is depicted in figure 1. There were 754 (68.2%) male and 351 (31.8%) female patients. These patients underwent a spectrum of operative modalities. 407 (36.8%) patients had planned open surgery, 448 (40.5%) were treated endoscopically, laparoscopy was employed in 239 (21.6%) patients. 3 (1%) patients had arthroscopy and 8 (1%) patients underwent Video- Assisted Thoracoscopy (VATS). Among the 239 patients in which laparoscope was used; 213 (89%) had a procedure that was successfully completed either laparoscopically or assisted with a laparoscope. Only 26 (11%) surgeries were converted to open due to procedural needs. 921 (83.3%) patients had a procedure less than 4 hours in duration while in 184 (16.7%) patients the procedure lasted for more than 4 hours. Out of 1105 patients, there were 339 (30%) who did not undergo COVID testing. These patients were operated before the implementation of hospital policy. However after the implementation of hospital policy, COVID testing was done for all patients prior to surgery. 100 patients tested positive for COVID for a total of 766 tests done. 92 patients tested positive on routine screening and had their operation delayed for a period of 2 weeks. 8 patients who were operated in emergency had COVID infection but surgery was not delayed due to emergent nature of the procedure as shown in figure 2. When analysing the hospital stay of these 100 patients who tested positive there were only 10 patients who were admitted to COVID facility and there were only 3 mortalities that were attributable to COVID as shown in table 1.
|
Diagnosis |
Procedure |
Post-OP Course |
Outcome |
|
Carcinoma cervix Pancytopenia secondary to hypocellular marrow |
Laproscopic splenectomy |
Admitted in covid icu for routine monitoring |
Discharged on home isolation |
|
Obstructed rectal cancer |
Laproscopic defunctioning colostomy (emergent) |
COVID Isolation Facility |
Discharged home |
|
Vocal cord cancer |
Tracheostomy |
COVID ICU on invasive ventilation with ventilator support- step down in isolation |
Discharged |
|
Renal cell carcinoma |
Left nephrectomy |
COVID Isolation Facility |
Discharged |
|
Carcinoma breast |
Arthroscopy lavage |
COVID Isolation Facility |
Discharged |
|
Acute lymphoid leukemia |
Incision drainage |
COVID Isolation Facility |
Discharged |
|
Perforated Sigmoid colon |
Hartman Procedure |
COVID Isolation Facility |
Discharged |
|
Pancreatic Adenocarcinoma |
Whipple’s Procedure |
COVID ICU |
Dead |
|
Advanced laryngeal carcinoma |
Tracheostomy |
COVID ICU with ventilatory support |
Dead |
|
Distal Pancreatic NET |
Laparoscopic Distal Pancreatectomy |
Remained on Invasive airway post-operaitvely due to atypical pneumonia |
Dead |
Table 1: Outcomes of patients admitted in COVID FACILITY from March 2020- July 2020
4. Discussion
The first case of novel corona virus was report on 26th February 2020 in Pakistan [8]. After this day, the rampant spread put a halt to all spheres of life. The mode of spread demanded that strict barrier methods and social distancing must be practised in true letter and spirit. Defying which, meant an accelerated and exponential rise in cases. Amidst the increasing deaths in patients having COVID- related pneumonia; all surgical procedures were suspended throughout the world. This included patients who had to undergo oncological surgery as well. After a vigorous effort to mitigate the contagion there was still a dilemma whether to declare surgery safe at all or not. A virus creating havoc for healthy individuals would surely prove to be disastrous for cancer stricken population. Our institute is a tertiary care level centre for cancer related treatment across Pakistan and has a catchment area as far as Afghanistan. A wide range of procedures were conducted at our centre from a wide array of specialties. Each procedure had a unique requirement and posed a greater challenge. Our centre continued to be at the forefront of providing surgical care during the pandemic. It helped averting the unnecessary delay in the care of oncologic patients. This not only helped the poor and needy patients but also guided us in devising an adept scheme for the future. A comprehensive standard of procedures were designed at our institute to continue the oncological service in a safe manner both for the patients as well as doctors who were at risk of contracting the infection. All patients who were planned for surgery had to undergo COVID testing via nasopharyngeal swab at least 48 hours before surgery. All those who tested positive were advised to observe home quarantine for 14 days. After successful completion of home quarantine they were called for surgery provided asymptomatic. Strict barrier methods including the use of an N-95 mask along with a surgical mask, provision of Personal Protective Kits for surgeons who were operating and anesthesia team were deemed mandatory [9]. The number of health care personals were reduced per shift to reduce the number of people exposed. Strict hand hygiene policy was observed at the bedside as well as at other places of physical contact with the patient. Seretis et al have recently published data of 100 patients operated in emergency for general surgery ailments and have reported that there is no additional morbidity in patients [10]. There were only 5 patients who developed respiratory infection in post-operative period out of which 2 were swab positive for COVID. In our study out of 176 patients undergoing emergency operations, 8 patients were admitted to COVID isolation and were discharged uneventfully later on. The safety of the laparoscopic procedures was also dubious due to the aerosol transmission of the virus. Surgical smoke was also considered as the carrier harbouring this scourge. Thus posing a great threat to the safety of surgeons and operation theatre attendees. In our study laparoscopy was used in 239 patients. There was only one patient who developed post-operative respiratory complications and died. Thus, the safety of laparoscopy can be established emphatically but additional evidence is still required. In our study there were two sets of population, those who underwent COVID pre-operatively and those who didn’t but were still operated. While comparing both these groups on the basis of their clinical outcome there was only 1 patient (out of 339 patients) in the NO-COVID testing done group who required admission in COVID facility and tested positive for COVID post-operatively. These results indicate that there was no statistically significant morbidity was seen in patients who tested positive in the peri-operative time. Only a limited studies are available to assess the post-operative morbidity and mortality post-operatively in COVID confirmed or suspected patients. To the best of our knowledge this is the first comprehensive database from Pakistan to assess the safety of surgery during COVID pandemic.
5. Conclusion
In the end we conclude that surgery can be undertaken in patients during COVID era by implementation of a standardized policy. The patients who test positive should be operated once their PCR is negative. Strict barrier and protective measures should be instituted. Patients should not be deferred unnecessarily with the fear of contracting COVID infection. Although there is a risk of acquiring COVID but the risk outweighs the benefits of delaying the surgery.
Conflict of interest
There are no conflict of interest to declare.
References
- Centres for Disease Control and Prevention. Interim guidance for healthcare facilities: preparing for community transmission of COVID-19 in the United States (2020).
- American College of Surgeons. COVID-19: guidance for triage of non-emergent surgical procedures (2020).
- Royal College of Surgeons. COVID-19: good practice for surgeons and surgical teams (2020).
- Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect Dis (2020).
- Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA (2020).
- Liang W, Guan W, Chen R, et al. Cancer patients in SARS- CoV-2 infection: a nationwide analysis in China. Lancet Oncol 21 (2020): 335-337.
- ‘Two corona virus cases confirmed in Pakistan- Pakistan Today’ (2019).
- Dhanani R, Wasif M, Pasha HA, et al. COVID-19: Implications, Reactions and Future Directions. Turkish archives of otorhinolaryngology 58 (2020): 122- 126.
- Seretis C, Archer L, Lalou L, et al. Minimal impact of COVID-19 outbreak on the postoperative morbidity and mortality following emergency general surgery procedures: results from a 3-month observational period. Medicinski glasnik : official publication of the Medical Association of Zenica-Doboj Canton, Bosnia and Herzegovina 17 (2020): 275-278.
- Pavan N, Crestani A, Abrate A, et al. Risk of Virus Contamination Through Surgical Smoke During Minimally Invasive Surgery: A Systematic Review of the Literature on a Neglected Issue Revived in the COVID-19 Pandemic Era. European urology focus 6 (2020): 1058-1069.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 