Laparoscopic approach for Diaphragmatic Hernia Repair in Adult - A 7-year Review of Single Center Experience
Taewook Yoo1, Duyeong Hwang1,2, Yun kyung Kang3, Yonghae Baik1,2*
1Department of Surgery, Dongguk University Ilsan Hospital, Goyang, Korea
2Department of Surgery, Dongguk University College of Medicine, Gyeongju, Korea
3Department of Pathology, Dongguk University College of Medicine, Gyeongju, Korea
*Corresponding Author: YongHae Baik, Department of Surgery, Dongguk University Ilsan Hospital, Siksa-dong, Ilsandong-gu, Goyang 10326, Korea
Received: 28 August 2025; Accepted: 09 September 2025; Published: 14 October 2025
Article Information
Citation: Taewook Yoo, Duyeong Hwang, Yun kyung Kang, Yonghae Baik. Laparoscopic approach for Diaphragmatic Hernia Repair in Adult - A 7-year Review of Single Center Experience. Journal of Surgery and Research. 8 (2025): 501-506.
View / Download Pdf Share at FacebookAbstract
Purpose: Diaphragmatic hernia in adults is a rare but potentially lifethreatening condition that often presents diagnostic and surgical challenges. With the increasing adoption of minimally invasive techniques, laparoscopic repair has emerged as a promising approach, yet evidence- particularly in elderly patients and in rare hernia subtypes- remains limited. This study aimed to evaluate the safety, feasibility, and outcomes of laparoscopic diaphragmatic hernia repair performed by a single experienced surgeon at a single center over a seven-year period.
Methods: A retrospective review was conducted of adult patients who underwent laparoscopic repair of diaphragmatic hernia at Dongguk University Ilsan Hospital between November 2017 and September 2023. Clinical data, including demographics, presenting symptoms, hernia characteristics, operative details, postoperative outcomes, and follow-up findings, were analyzed.
Results: Eleven patients (10 females; mean age, 73.8 ± 14.4 years) underwent laparoscopic repair. Hernia types included hiatal hernia (n=6, 54.5%), Morgagni hernia (n=4, 36.4%), and Bochdalek hernia (n=1, 9.1%). One patient (9.1%) required conversion to open surgery due to intraoperative pneumothorax. The mean operative time was 242.4 ± 109.6 minutes, and the mean hospital stay was 16.2 ± 11.3 days. Postoperative complications occurred in 2 patients (18.1%), all minor (Clavien–Dindo grade ≤ IIIa), and resolved with conservative management. There were no major complications, no 30-day mortalities, and no clinical or radiological recurrences during a mean follow-up of 16.3 ± 7 months.
Conclusion: Laparoscopic repair of adult diaphragmatic hernias is safe and feasible, even in elderly patients, and is associated with low morbidity and no mid-term recurrences.
Keywords
<p>Diaphragmatic hernia, Hiatal hernia, Morgagni hernia, Bochdalek hernia, Hernia, Laparoscopic surgery</p>
Article Details
Introduction
A diaphragmatic hernia (DH) is defined as the herniation of abdominal contents into the thoracic cavity through a defect in the diaphragm [1]. While DH in adults is rare, it can present as a surgical emergency and is associated with considerable morbidity and potential postoperative complications [2]. Despite its clinical relevance, standardized guidelines for the management of adult DH are lacking [3]. Regardless of etiology, adult DH frequently presents as a diagnostic and therapeutic challenge, with symptoms ranging from vague gastrointestinal discomfort or respiratory complaints to life-threatening emergencies such as strangulation, perforation, or bowel obstruction [4].
Historically, the standard surgical approach for adult DH repair has been open thoracotomy or laparotomy [5]. Although these techniques provide excellent operative exposure, they are associated with considerable postoperative pain, prolonged hospitalization, and delayed functional recovery, particularly in elderly patients or those with significant comorbidities. With the rapid evolution of minimally invasive techniques, laparoscopic repair has emerged as an attractive alternative, offering superior visualization, reduced surgical morbidity, and faster postoperative recovery [6]. However, the rarity of this condition and the anatomical variability of diaphragmatic defects—including hiatal, Morgagni, and Bochdalek hernias—have precluded the establishment of standardized surgical strategies or evidence-based clinical guidelines [7].
Despite the increasing proportion of elderly patients diagnosed with diaphragmatic hernia, studies focusing on this population remain limited. Older patients often present with multiple comorbidities and a generally diminished physical condition, which makes surgical planning and perioperative management more complex [8]. Minimally invasive approaches, including laparoscopic repair, may offer significant benefits in these patients by reducing postoperative pain, shortening recovery time, and minimizing pulmonary complications [9]. However, evidence specifically addressing the outcomes of laparoscopic repair in elderly patients is scarce, and surgical techniques remain heterogeneous across institutions and surgeons. This lack of standardization highlights the need for more robust data to establish safe, reproducible, and evidence-based strategies for managing diaphragmatic hernias in this growing patient population [10].
This study analyzes the clinical outcomes of laparoscopic DH repair performed by a single surgeon at a single institution over a seven-year period. This experience provides valuable insights into the safety, feasibility, and potential advantages of a laparoscopic approach across different hernia types, contributing to the evidence base required for developing standardized management strategies.
Methods
A retrospective review was conducted of adult patients who underwent laparoscopic repair of diaphragmatic hernia at the department of surgery, Dongguk University Ilsan Hospital, between Nov 2017 and Sep 2023. All procedures were performed by a single surgeon with over 20 years of experience in advanced laparoscopic and gastric cancer surgery. During this period, a total of 11 adult patients underwent laparoscopic repair and were included in this review. Clinical data collected and analyzed included demographic characteristics, presenting symptoms, preoperative imaging findings, intraoperative details, postoperative outcomes, and follow-up results.
Surgical technique
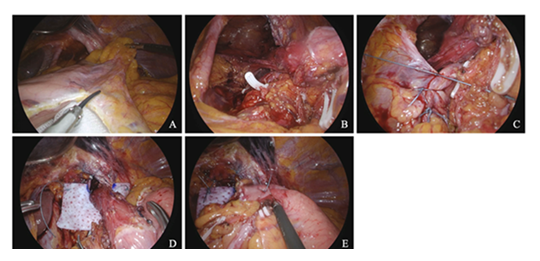
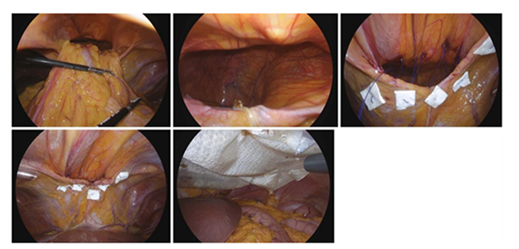
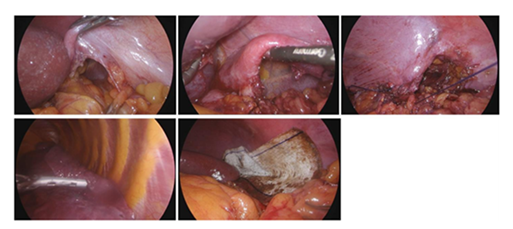
For hiatal and Morgagni hernias, patients were placed in the lithotomy position with reverse Trendelenburg. For Bochdalek hernia, the procedure was performed with the patient in the lateral decubitus position. The operation surgeon stood on the right side of patient, with the first assistant on the left and the scopist positioned between the legs. Herniated abdominal contents were carefully reduced to the abdominal cavity to fully expose the diaphragmatic defect. When indicated, the hernia sac was excised. The defect was closed using interrupted non-absorbable sutures, and, when reinforcement was deemed necessary, a prosthetic mesh was applied and secured with sutures and permanent tacks. The key intraoperative steps are illustrated (figures 1-3).
- Herniation of the stomach and omentum through the hiatus (stomach, omentum)
- Intraoperative view inside the hiatal defect
- Intracorporeal suture closer of the defect
- Mesh fixation with non-absorbable suture and permanent tacks
- Completion of Nissen fundoplication
- Herniation of the colon and omentum into the anterior mediastinum
- Intraoperative view inside the Bochdalek defect
- Placement of transfascial sutures for defect closure
- Interior aspect demonstrating secure suture placement
- Double-layer mesh reinforcement with sutures and permanent tacks
- Herniation of abdominal viscera through the posterior diaphragmatic defectBochdalek hernia with the abdominal contents
- Intraoperative view of the Bochdalek defect
- Intracorporeal suture closure of the defect
- Placement of a chest tube when indicated to manage pneumothorax or pleural effusion
- Mesh reinforcement with sutures and permanent tacks
Result
Patient characteristics
Between November 2017 and September 2023, 11 patients underwent laparoscopic diaphragmatic hernia repair. 10 patients (90.9%) were female. The mean age was 73.8 years, and the mean BMI was 25.3 kg/m² (range, 19.5–31.5). By ASA class, 10 (90.9%) were class II and 1 (9.1%) was class III. Hernia side was left in 6 (54.5%) and right in 5 (45.5%) (Table 1).
|
Variables |
|
|
Average age (years) |
73.8 ± 14.4 (range 34-88) |
|
Sex |
|
|
Male |
1 (9.1%) |
|
Female |
10 (90.9%) |
|
Height (cm) |
150.0 ± 10.9 (range 138-176.2) |
|
Weight (kg) |
57.9 ± 15.2 (range 37.1-97.8) |
|
BMI (kg/m2) |
25.3 ± 3.26 (range 19.5-31.5) |
|
ASA classification, n (%) |
|
|
II |
10 (90.9%) |
|
III |
1 (9.1%) |
|
Hernia side, n (%) |
|
|
Right |
5 (45.5%) |
|
Left |
6 (54.5%) |
Table 1: Patients demographics.
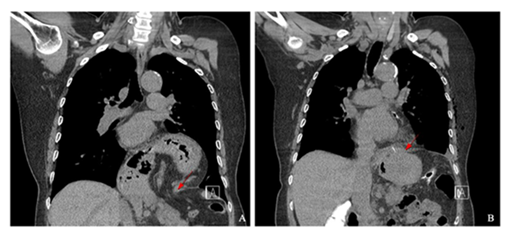
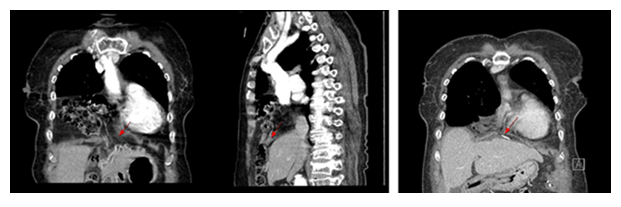
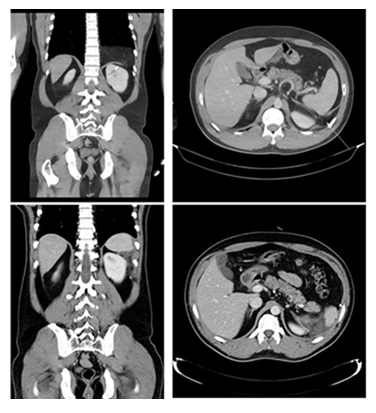
The most common presenting symptom was gastrointestinal discomfort (5/11, 45.5%), followed by chest pain (2/11, 18.2%), respiratory distress (2/11, 18.2%), and back pain (2/11, 18.2%); three patients (27.3%) were asymptomatic at diagnosis (Table 2). Computed tomography (CT) established the preoperative diagnosis in all patients, and routine postoperative CT was obtained on postoperative day (POD) 5 (POD 6 for the Bochdalek case) (Figures 4-6).
|
Variables |
Number of patients, n (%) |
|
Asymptomatic |
3 (27.3) |
|
Chest pain |
2 (18.2) |
|
Respiratory distress |
2 (18.2) |
|
Gastrointestinal discomfort (vomiting, GERD, dysphagia) |
5 (45.5) |
|
Back pain |
2 (18.2) |
Table 2: Major symptoms of the patients.
- Hiatal hernia; Pre-OP CT
- Post-OP CT (POD #5)
- Morgagni hernia ; Pre-OP CT
- Post-OP CT (POD#5)
- Bochdalek hernia ; Pre-OP CT
- Post-OP CT (POD #6)
Hernia types and procedures
Hernia types included hiatal hernia in 6 patients (54.5%), Morgagni hernia in 4 patients (36.4%), and Bochdalek hernia in 1 patients (9.1%). One case required conversion to open surgery for intraoperative pneumothorax. In one hiatal hernia patients with concomitant gastric ulcer perforation, laparoscopic distal gastrectomy was additionally performed.
Repair methods included primary suture repair in 2 patients and mesh reinforcement in 9 patients. The most frequently herniated organs were the stomach and omentum; the colon was involved in 2 cases. Intraoperative chest tube were placed in 2 patients (18.1%).
The mean operative time was 242. 4 ± 109.6 minutes, and the mean length of hospital stay was 16.2 ± 11.3 days (Table 3).
|
Patients number |
Type of hernia |
Repair of defect |
Sac contents |
Chest tube |
Operation time (min) |
Hospital day (days) |
|
1 |
Hiatal |
mesh |
colon, stomach |
No |
220 |
23 |
|
2 |
Hiatal |
mesh |
stomach |
Yes |
214 |
22 |
|
3 |
Hiatal |
suture |
stomach |
No |
250 |
36 |
|
4 |
Hiatal |
mesh |
stomach |
No |
233 |
8 |
|
5 |
Morgagni |
mesh |
colon |
No |
169 |
7 |
|
6 |
Hiatal |
mesh |
stomach |
No |
375 |
10 |
|
7 |
Morgagni |
mesh |
omentum |
No |
100 |
7 |
|
8 |
Bochdalek |
mesh |
omentum |
Yes |
320 |
10 |
|
9 |
Morgagni |
mesh |
omentum |
No |
150 |
9 |
|
10 |
Hiatal |
suture |
stomach, omentum |
No |
475 |
36 |
|
11 |
Morgagni |
mesh |
colon, omentum |
No |
160 |
10 |
Table 3: Operative data.
The mean operative time for the cohort was 242.4 ± 109.6 minutes. The mean hospital stay was 16.2 ± 11.3 days. Postoperative complications occurred in 2 of 11 patients (18.1%). However, there were no major complications (Clavien–Dindo grade ≥ IIIA) reported. All observed complications were minor, managed conservatively, and did not necessitate reoperation or invasive intervention. There were no 30-day mortalities and no hernia recurrences during the follow-up period. The mean follow-up duration was 16.3 ± 7 months (range, 3-24 months), during which no cases of radiologic or clinical recurrence were detected.
|
Variables Category |
|
|
Mean operation time (minutes) |
242.4 ± 109.6 |
|
Hospital day (days) |
16.2 ± 11.30 |
|
Overall complication, n (%) |
2 (18.1%) |
|
Complication ≥ Gr. IIIA, n (%) |
0 (0 %) |
|
30-day mortality, n |
0 |
|
Mean follow-up (month) |
16.3 ± 7 (range 3 – 24) |
|
Recurrence, n (%) |
0 (0 %) |
Table 4: Postoperative complication and follow-up Surgical outcomes.
Discussion
Through this study, our findings suggest that surgical repair of adult diaphragmatic hernias can be safely performed in elderly patients. The mean patient age of 73.8 years underscores the increasing trend of delayed or incidental diagnoses in older adults, a demographic shift driven by the widespread availability of advanced imaging modalities and longer life expectancy [8,11]. In our series, minimally invasive repair was feasible in all patients, with only one conversion to open surgery due to intraoperative pneumothorax, reflecting the technical adaptability and safety of the laparoscopic approach.
No Clavien–Dindo grade IIIA or higher complications were observed, and there were no surgery-related mortalities. Postoperative complications occurred in 18.1% of patients, but all were grade IIIa or lower and resolved with conservative management. During the follow-up period (mean, 16.3 months), there were no clinical or radiological recurrences. This study included four cases of Morgagni hernia and one case of Bochdalek hernia. Historically, these hernia types have often been managed with thoracotomy or laparotomy due to their anatomical complexity and associated cardiopulmonary risks. However, our findings suggest that, in the hands of a highly experienced surgeon, laparoscopic repair can be safely and effectively applied even to these rare hernias [5,12]. Furthermore, the minimally invasive approach offers additional advantages, such as reduced postoperative pain, faster recovery, and better cosmetic outcomes [2,6].
This study also included four Morgagni hernias and one Bochdalek hernia. Historically, these rare types have often been managed with thoracotomy or laparotomy due to their anatomical complexity and associated cardiopulmonary risks [1]. However, our findings, together with contemporary reviews and case series, suggest that laparoscopic repair can be safely and effectively applied even to these rare hernias when performed by experienced surgeons [13,14]. In addition to safety and effectiveness, the minimally invasive approach offers advantages such as reduced postoperative pain, faster recovery, and superior cosmetic outcomes. Furthermore, our technique aligns with guideline recommendations for concomitant fundoplication in type II–IV hiatal hernia repair, supporting a standardized and evidence-based approach [15].
The predominance of elderly patients in our cohort highlights the clinical importance of minimally invasive surgery in this population. Previous studies have shown that open repair in older patients is associated with higher morbidity and mortality [3]. In contrast, laparoscopic repair reduces surgical trauma and pulmonary complications, and facilitates faster recovery, making it particularly advantageous for elderly or comorbid patients [13,16]. One of the major strengths of this study is that all procedures were performed by a single surgeon with over 20 years of experience in advanced laparoscopic surgery for upper gastrointestinal conditions. This likely minimized technical variability and contributed to consistent outcomes.
However, several limitations must be acknowledged. The retrospective design, small sample size, and relatively short follow-up period limit the generalizability of these findings. Additionally, the single-surgeon nature of this study means that similar outcomes may be more difficult to reproduce by less experienced surgeons or at other institutions.
Future large-scale, multicenter prospective studies with longer follow-up are warranted to further clarify the safety and durability of laparoscopic repair. Establishing standardized criteria for patient selection, operative technique, and postoperative management will also help strengthen the evidence base and support the development of optimized treatment protocols for adult diaphragmatic hernia repair.
Conclusion
Laparoscopic repair of diaphragmatic hernia in adults, including rare subtypes such as Morgagni and Bochdalek hernias, is safe, feasible, and durable, even in elderly patients with comorbidities. The procedure is associated with low morbidity, no major complications, and no recurrences during mid-term follow-up. With growing experience and refinement of minimally invasive techniques, laparoscopic repair should be considered the preferred approach for most adult diaphragmatic hernias. Future multicenter, prospective studies with larger cohorts and longer follow-up are needed to establish evidence-based protocols and to further validate these encouraging results.
Acknowledgements
Not applicable.
Authors’ contributions
Study conception and design: TY and YB. Acquisition of data: TY. Analysis and interpretation of data: TY and YH. Drafting of manuscript: TY. Critical revision of manuscript and editing: TY and YB.
Funding
Not applicable.
Availability of data and materials
The datasets of the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
All procedures were conducted in accordance with the principles of the Declaration of Helsinki, and the study protocol was reviewed and approved by the Ethics Committee of Dongguk University Hospital. This study was based on retrospectively collected clinical data and did not involve any prospective enrollment of human participants. The requirement for informed consent was waived by our institutional ethics committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- Losanoff JE, Sauter ER. Congenital posterolateral diaphragmatic hernia in an adult. Hernia 8 (2004): 83-85.
- Testini M, Girardi A, Isernia RM, et al. Emergency surgery due to diaphragmatic hernia: case series and review. World J Emerg Surg 12 (2017): 23.
- Hanna WC, Ferri LE, Fata P, et al. The current status of traumatic diaphragmatic injury: lessons learned from 105 patients over 13 years. Ann Thorac Surg 85 (2008): 1044-1048.
- Brown SR, Horton JD, Trivette E, et al. Bochdalek hernia in the adult: demographics, presentation, and surgical management. Hernia 15 (2011): 23-30.
- Machado NO. Laparoscopic Repair of Bochdalek Diaphragmatic Hernia in Adults. N Am J Med Sci 8 (2016): 65-74.
- Palanivelu C, Rangarajan M, Rajapandian S, et al. Laparoscopic repair of adult diaphragmatic hernias and eventration with primary sutured closure and prosthetic reinforcement: a retrospective study. Surg Endosc 23 (2009): 978-85.
- Gedik E, Tuncer MC, Onat S, et al. A review of Morgagni and Bochdalek hernias in adults. Folia Morphol (Warsz) 70 (2011): 5-12.
- Kumar SS, Rama M, Koeneman S, et al. Morbidity and mortality following hiatal hernia repair in geriatric patients: a multicenter research network study. Surg Endosc 38 (2024): 3999-4005.
- Oh S, Lim SK, Cho JH, et al. Surgery for Diaphragmatic Hernia Repair: A Longitudinal Single-Institutional Experience. J Chest Surg 56 (2023): 171-176.
- Saroj SK, Kumar S, Afaque Y, et al. Laparoscopic Repair of Congenital Diaphragmatic Hernia in Adults. Minim Invasive Surg 16 (2016): 9032380.
- Thoman DS, Hui T, Phillips EH. Laparoscopic diaphragmatic hernia repair. Surg Endosc 16 (2002): 1345-1349.
- Ağalar C, Atila K, Arslan N, et al. Adult morgagni hernia: a single center experience of 5 cases and review of literature. Turk J Surg 35 (2019): 321-324.
- Amprayil MA, Irvine T, Thompson SK, et al. Safety and Early Clinical Outcomes Following Repair of Very Large Hiatus Hernia in Octogenarians. World J Surg 49 (2025): 1237-1245.
- Oelschlager BK, Pellegrini CA, Hunter J, et al. Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg 244 (2006): 481-490.
- Oelschlager BK, Pellegrini CA, Hunter JG, et al. Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg 213 (2011): 461-468.
- Collins ML, Mack SJ, Till BM, et al. Defining risk factors for mortality after emergent hiatal hernia repair in the era of minimally invasive surgery. Am J Surg 225 (2023): 1056-1061.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 