Assessing Preoperative Anxiety: Comparison of three simple Anxiety Scales
Roya Yumula,b, Ofelia Loani Elvir-Lazoa*, Paul F. Whitea,c, Xiao Zhangd, Waguih William IsHaka,e, David Chernobylskya, Omar Durraa,f, Hamed Sadeghipoura,g
aDepartment of Anesthesiology, Cedars-Sinai Medical Center, Los Angeles, CA, USA
bDavid Geffen School of Medicine-UCLA, Charles R, Drew University of Medicine and Science, Los Angeles, CA, USA
cWhite Mountain Institute, The Sea Ranch, CA, USA (a not-for-profit private foundation)
dDepartment of Mathematical Sciences, Michigan Technological University. Houghton, MI USA
eDepartment of Psychiatry, Cedars-Sinai Medical Center, Los Angeles, CA, USA
fDepartment of Anesthesiology, Keck School of Medicine. Los Angeles, CA, USA
gDepartment of Anesthesiology and Critical Care, Saint Louis University School of medicine. Saint Louis, MO, USA
*Corresponding Author: Ofelia Loani Elvir-Lazo, Department of Anesthesiology, Cedars-Sinai Medical Center, Los Angeles, CA, USA
Received: 02 July 2024; Accepted: 15 July 2024; Published: 30 August 2024
Article Information
Citation: Roya Yumul, Ofelia Loani Elvir-Lazo, Paul F. White, Xiao Zhang, Waguih William IsHak, David Chernobylsky, Omar Durra, Hamed Sadeghipour. Assessing Preoperative Anxiety: Comparison of three simple Anxiety Scales. Journal of Surgery and Research. 7 (2024): 386-394
View / Download Pdf Share at FacebookAbstract
Background: Preoperative anxiety is a significant concern for many patients undergoing elective surgery as it can negatively impact many aspects of anesthesia. Perioperative anxiety is associated with increased autonomic variability, higher anesthetic and analgesic requirements, and a greater incidence of nausea, vomiting, and pain during the early postoperative period. This prospective study was designed to compare the assessment of acute preoperative (state) anxiety using a visual analog scale (VAS), the Categorical Anxiety Scale (CAS) and a novel emoji-based Visual Facial Anxiety Scale (VFAS).
Methods: 293 adult patients undergoing elective surgical procedures were enrolled in this observational, prospective cohort study. In the preoperative evaluation area, anesthesia providers were questioned about their methods for assessing preoperative anxiety. After the anesthesiologists completed their evaluations and left the area, a co-investigator administered three anxiety assessment tools to the patients in a random order in the preoperative holding area before they entered the operating room.
Results: There was a significant correlation (p<0.0001) among the anxiety scores of the three simplified scales [VFAS vs VAS (r=0.738), VFAS vs CAS (r=0.759), and VAS vs CAS (r=0.861)]. The means and standard deviations of the score values for each of anxiety scales were: VFAS 2.02±0.94, VAS 3.39±2.5, and CAS 2.41±1.29. The times to perform the VFAS (7.3 ± 1.6 sec), VAS (7.2 ± 1.6 sec), and CAS (7.3 ± 1.9 sec) assessments were similar for the three scales. The patient’s top-ranked assessment scale was the VFAS (73%), followed by the VAS (15.6%) and the CAS (11%). The anesthesiologists’ top ratings were given to the VFAS (64%), followed by the VAS (22%), and the CAS (14%).
Conclusions: All three of the simple analog-based scales were highly correlated for assessing acute (state) anxiety and required only a short time to complete (<15 sec). The emoji-based scale was rated most highly by the patients.
Keywords
<p>Assessing preoperative anxiety, Simplified anxiety scales, Visual analog scale, Categorical anxiety scale, Visual facial anxiety scale</p>
Article Details
Introduction
During the immediate preoperative period, patients commonly experience significant anxiety [1,2]. Optimizing the management of preoperative anxiety has the potential to mitigate common perioperative complications and enhance recovery processes [3-11]. However, conducting an anxiety assessment can be time-consuming in busy preoperative holding areas. Therefore, it is crucial to employ a tool for measuring acute (state) anxiety that is both sensitive and can be administered rapidly in busy preoperative environment. Excessive preoperative anxiety levels has been correlated with higher requirements for anesthetic and analgesic medications, increased occurrences of nausea, vomiting, severe pain, and extended discharge times [11-15]. Furthermore, anxiety has been linked to a higher incidence of bronchospasm among asthmatic patients, elevated mortality rates post cardiac surgery, and delayed wound healing following surgery [16-19]. Anxiety often stems from concerns related to past surgical or anesthetic experiences [20-26].
Several tools have been used to assess preoperative anxiety including the ‘gold standard’ state-trait anxiety inventory (STAI), the Beck anxiety inventory (BAI), hospital anxiety and depression scale-anxiety (HADS-A), the Amsterdam preoperative anxiety and information scale (APAIS), Perioperative Anxiety Scale-7 (PAS-7), and the Yale preoperative anxiety scale (YPAS) [27-33]. Although highly accurate, mostly of these assessment tools are very time consuming to complete and therefore, impractical in a busy preoperative holding area [34,35]. Alternative evaluation tools which are less time consuming to administer include the visual analog scale (VAS), Visual Facial Anxiety Scale (VFAS), and categorical anxiety scale (CAS) [36-38].
The primary objective of this study was to compare the novel simplified VFAS to the VAS, and the CAS for assessing a patient’s level of acute preoperative anxiety in the preoperative holding area. The secondary objective was to assess the causes of preoperative anxiety reported by this elective surgery population.
Methods
This observational, prospective cohort study (IRB # Pro00043383) was approved by the Institutional Review Board (IRB) at Cedars-Sinai Medical Center in Los Angeles, CA on [8/10/2016]. Of the 302 patients who met the study entrance criteria, 293 gave written-informed consent to participate in the study and all successfully completed the study. Inclusion criteria of the study population consisted of 293 ASA I-III patients (>18 yo), scheduled to undergo elective surgery (e.g., general, orthopedic, and OB/GYN procedures). Exclusion criteria included patients with Alzheimer’s disease, dementia, any psychiatric diseases, or mental retardation, as well as patients taking chronic anti-anxiety, antidepressant, or sedative medications.
The attending anesthesiologists met with patients after they were admitted to the preoperative evaluation area and explained that the purpose of the study and obtained a signed written consent form from each patient. The investigator was present to observe the routine perioperative evaluations by the attending anesthesiologists and to record the method, if any, used to evaluate the patient’s level of preoperative anxiety. When the preoperative evaluation by the attending anesthesiologist was concluded they left the area while a co-investigator performed the three anxiety assessments tools in the preoperative holding area. Patient demographics were obtained from the medical records and medical history provided by the patients including age, gender, ethnicity, psychiatric history, co-morbidities, smoking and substance abuse history. Additional demographic information included marital status, education level, current living situation, health insurance coverage, chronic anxiety and pain medication, type of elective surgery, anesthesia and surgical history, as well as any previous surgery and anesthesia-related complications.
2.1. Study procedure
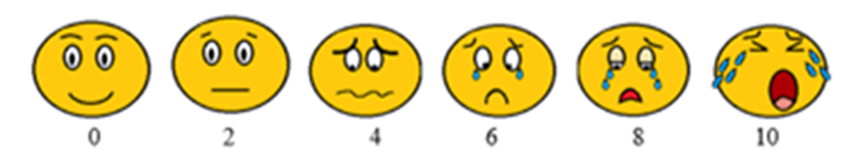
Upon enrollment in the clinical trial, patients were administered the three anxiety measurement scales namely the VFAS (Figure 1a), VAS (Figure 1b), CAS (Figure 1c). All tools were administered in a random order to reduce bias associated with fixed-sequence testing administration. While patients completed the evaluation tools, a study staff member, not involved in administering the evaluations recorded the time it took patients to complete each of the 3 anxiety evaluation tools using a hand-held stopwatch. Time measurements were performed discreetly to minimize the ‘Hawthorne’ effect bias’ [39]. All study evaluations were completed in the preoperative evaluation area prior to entering the operating room (OR). Participants did not receive any sedative-anxiolytic premedication prior to the completion of their anxiety evaluation tests.
Following completion of the three anxiety evaluation tools, patients were asked to rank their preferred evaluation tool (i.e., the assessment tool which most accurately reflected their level of anxiety), and the cause(s) of any preoperative anxiety. The specific causes of anxiety were selected by the patients from a list provided by the study personnel and included: (1) fear of death, (2) waiting to enter the operating room (OR), (3) insufficient information regarding surgery/anesthesia, (4) fear of the operation or anesthesia (e.g., being awake during operation), (5) fear of needles and other interventions, (6) postoperative pain, sedation and/or postoperative nausea and vomiting, (7) need for a blood transfusion, (8) physical and mental harm, (9) lack of medical insurance coverage, (10) concerns about family and friends, potential financial loss due to time away from work, and being at the mercy of medical staff.
All surgical and anesthesia protocols followed the prescribed standard of care at Cedars-Sinai Medical Center in Los Angeles. Preoperative sedative, intraoperative and postoperative anesthetic and analgesic drugs were recorded. Data on anesthesia time, surgery time, and PACU stay time were also recorded. On admission to the PACU, the patients pain score was evaluated on a 10-point visual analog scale.
2.2. Explanations of the three assessment tools (Figure 1)
(1) VFAS (1a.): face one (zero/no anxiety), face two (1-2/mild anxiety), face three (3-4/ mild-moderate anxiety), face four (5-6/moderate anxiety), face five (7-8/ moderate-high anxiety), face six (9-10/ high anxiety).
(2) VAS (1b.): zero (no anxiety), 1-2 (mild anxiety), 3-4(mild-moderate anxiety), 5-6 (moderate anxiety), 7-8 (moderate-high anxiety), 9-10 (high anxiety).
(3) CAS (1c.): zero (no anxiety), 1-2 (mild anxiety), 3-4 (mild-moderate anxiety), 5-6 (moderate anxiety), 7-8 (moderate-high anxiety), and 9-10 (high anxiety).
2.3. Statistical analysis
A sample size of 293 patients was compared via means based on the type of anxiety assessment tool. Means were meant to be compared by power analysis based on the assumption that the time, preference of the VFAS test were similar among the groups. The correlation analysis between VFAS, VAS, and CAS were conducted via Spearman’s rank correlation analysis utilizing ranked data, in order to draw comparisons similar to correlations to VAS, the Amsterdam Preoperative Anxiety and Information Scale, and STAI in the literature.32 From the studies described in the literature, the coefficient alphas of VAS, and STAI (Cα1) were determined to be 0.80 and the coefficient alphas of VAS and STAI (Cα2) was determined to be 0.70. The sample size to achieve 80% statistical power to detect a difference between the alpha coefficients of each group was determined to be 293 participants.
The analysis was performed using SAS 9.4 for Windows (SAS Institute, Cary, NC, USA) and R. 3.0.1. Our dataset contained both categorical and continuous measurements. For categorical measures, we presented total numbers (n) with the percentages (%) and used Chi-squared test to conduct comparisons of the groups. For continuous measurements, mean values and standard deviations were presented for comparison. For comparisons among continuous and ordinal measures, the Kruskal-Wallis Test was conducted. Data are presented as mean ± SD, numbers (n), and percentages (%), with p-values less than or equal to 0.05 considered statistically significant.
Results
A total of 293 patients (53% females and 47% males) were recruited to participate in the study. 17% of the patients took an antianxiety medication on the night before surgery and 33% took a non-opioid analgesic medication on the night prior to surgery. Demographic and clinical characteristics of the study population are summarized in table 1.
The demographic variables which were associated with significantly-different mean preoperative anxiety scores on one or more of the three anxiety scales were: (1) Gender (female > male): (p<.0001), (2) Age (< 40 yo > 40-60 yo and >60 yo): (p=0.001), (3) Marital status (married > single): (p=0.032), (4) Patients who did not take anxiety medication on the night before surgery had higher anxiety scores than those who took an anxiety medication on the night prior to the operation (p=0.018), (5) Previous surgery had higher anxiety scores than those undergoing their first operation (p=0.0006), (6) Previous anesthetic complication (vs. no previous anesthetic complications) (p=0.035), and (7) Patients who had 3-5 previous surgical procedures (vs. none, 1-2 or > 5 previous surgical procedures) (p=0.026) (Table 1).
|
Variables/ p values |
VFAS |
VAS |
CAS |
|
Gender: female* (53%)/male (47%) |
0.0022* |
<.0001* |
<.0001* |
|
Age: <40 *(21%)/ >40 <60 (32%)/ >60 (47%) |
0.857 |
0.775 |
0.461 |
|
ASA: 1 (15%) /2 (50%) /3 (35%) |
0.128 |
0.184 |
0.225 |
|
Marital status: married* (57%)/single (43%) |
0.0328* |
0.503 |
0.742 |
|
Living condition: alone (79.2%)/ with others (20.8) |
0.213 |
0.646 |
0.555 |
|
Educational status (years) |
0.667 |
0.202 |
0.65 |
|
<10y (0.3%)/ 10-15y (15.7%)/ >15 (84%) |
|||
|
Tobacco user: current (1%)/former (4.4%), nonsmoker (94.6%) |
0.287 |
0.21 |
0.725 |
|
Patients who took anxiety meds before preadmission (17.41%) |
0.277 |
0.0314* |
0.0185* |
|
Patients who took pain medications before preadmission (32.76%) |
0.085 |
0.352 |
0.077 |
|
Type of surgery: general (46%), orthopedic (27%) NeuroSpine (16%), cardiothoracic (5%), vascular (3%), OB/GYN (3%) |
0.52 |
0.259 |
0.419 |
|
Type of anesthesia: |
0.619 |
0.775 |
0.256 |
|
general anesthesia (76%), MAC sedation (24%) |
|||
|
Current Surgery Sequence: |
0.123 |
0.663 |
0.67 |
|
None (10%), 1-2 (34%), 3-5* (33%), >5 (22%), No answer (1%) |
|||
|
Patients with prior Surgery (89%) |
0.556 |
0.072 |
0.125 |
|
Patients with prior Surgery with complications (9%) |
0.791 |
0.968 |
0.864 |
|
Patients with prior anesthesia (92%) |
0.518 |
0.613 |
0.653 |
|
Patients with prior anesthesia with complications (7%) |
0.06 |
0.1 |
0.155 |
Percentages (%), p value <0.05*
Table 1: Demographic, clinical characteristics, and types of surgery of adult patients undergoing elective surgery and Spearman’s correlation between preoperative anxiety scores using the Visual Facial Anxiety Scale (VFAS), the Visual Analog Scale (VAS), and the Categorical Anxiety Scale (CAS) as anxiety assessment tools.
The preferred preoperative anxiety scale (using a 4-point rating scale) by patients was the VFAS scale (73%), followed by the CAS (15.6%) and the VAS (11.4%). The means and standard deviations of the score values for each of anxiety scales were: VFAS 2.02±0.94, VAS 3.39±2.5, and CAS 2.41±1.29 (Table 2). The times required for performing each of the anxiety evaluations were comparable: VFAS (7.3 ± 1.6 sec), VAS (7.2 ± 1.6 sec), and CAS (7.3 ± 1.9 sec) (Table 2). There was a significant Spearman’s Correlation (SC) among the anxiety scores of the three simplified scales [VFAS vs VAS (r=0.738), VFAS vs CAS (r=0.759), and VAS vs CAS (r=0.861)], with p-values <0.0001) (Table 3).
|
Anxiety scale scores (minimum-maximum scores) |
Means value (± SD) |
Median -Range values |
|
VFAS (1-6) |
2.02 ± 0.94 |
2 (1-5) |
|
VAS (0-10) |
3.39 ± 2.50 |
3 (0-10) |
|
CAS (1-6) |
2.41 ± 1.29 |
2 (1-6) |
|
Evaluation Times (sec) |
||
|
VFAS |
7.29 ± 1.61 |
7 (1-13) |
|
VAS |
7.23 ± 1.60 |
7 (4-14) |
|
CAS |
7.29 ± 1.99 |
7 (1-13) |
Values are presented in Mean ± Standard Deviation (SD)
Table 2: Preoperative Anxiety scale scores using the Visual Facial Anxiety Scale (VFAS), the Visual Analog Scale (VAS), and the Categorical Anxiety Scale (CAS) as anxiety assessment tools.
|
Preoperative Anxiety Scales |
Correlation Coefficient (r) |
p-value |
|
VFAS vs VAS |
0.738* |
p<0.0001 |
|
VFAS vs CAS |
0.759* |
p<0.0001 |
|
VAS vs CAS |
0.861* |
p<0.0001 |
Significant p value <0.0001*
Table 3: Spearman’s correlation coefficients among the anxiety scores of the Visual Facial Anxiety Scale (VFAS), the Visual Analog Scale (VAS), and the Categorical Anxiety Scale (CAS) as anxiety assessment tools.
No significant correlations were found between the scales based on the patient’s preoperative anxiety score with respect to preoperative waiting time, surgery/anesthesia time, surgery-anesthesia start time, PACU stay, patients with and without preoperative pain, or pain score at PACU or during discharge PACU and PACU analgesic requirement in morphine equivalents (Table 4).
Furthermore, there was a significant correlation between the preoperative anxiety score and the maximum pain score in the PACU for the VFAS scale (p= 0.0359). In addition, there was a correlation between the preoperative anxiety score and the maximum pain score prior to discharge for all three scales: VFAS (p=0.0008), VAS (p=0.008), and CAS (p=0.0063), (Table 4).
The most frequent causes of preoperative anxiety reported were: (1) waiting in pre-operation area 165 (56%), (2) pain 125 (43%), (3) concern about their family 119 (41%), (4) lack of information about the operation, 117 (40%), (5) lack of information regarding anesthesia 92 (31%), (6) needles/catheters 87 (30%), (7) fear of the operation 81 (28%), (8) not awakening from anesthesia 77 (26%), (9) loss of control 72 (25%), (10) “awareness” during anesthesia 69 (24%), (11) postoperative nausea and vomiting 64 (22%), (12) fear of anesthesia 58 (20%), (13) physical and mental harm 53 (18%), (14) financial loss 49 (17%), (15) inadequate insurance coverage 49 (17%), (16) being at the mercy of the medical staff 47 (16%), (17) requiring blood transfusion 46 (16%), (18) miscellaneous reason 30 (10.5%).
|
Variables |
VFAS |
VAS |
CAS |
|
Preoperative |
|||
|
Preoperative pain score |
p=0.469 |
p=0.533 |
p= 0.645 |
|
Waiting time (preoperative area) |
p=0.278 |
p=0.653 |
p=0.421 |
|
≤120min/ ≥121 min |
|||
|
Anesthesia start time: |
|||
|
7-11AM |
|||
|
11AM-3PM |
p=0.798 |
p=0.359 |
p=0.307 |
|
3-7PM |
|||
|
Intraoperative medications |
|||
|
IV propofol |
p= 0.596 |
p= 0.57 |
p= 0.879 |
|
Total IV Morphine Eq |
p=0.0171* |
p= 0.0292* |
p= 0.0269* |
|
Surgery Time ≤120 min/ ≥ 121 min |
p=0.729 |
p=0.457 |
p=0.42 |
|
Anesthesia Time ≤120 min/ ≥ 121 min |
p=0.314 |
p=0.245 |
p=0.183 |
|
PACU Variables |
|||
|
Duration of PACU stay |
p=0.639 |
p=0.5005 |
p=0.6497 |
|
Pain scores upon admission to the PACU |
p=0.149 |
p= 0.388 |
p= 0.4042 |
|
Maximum pain score in the PACU |
p= 0.0359* |
p= 0.13 |
p=0.1225 |
|
Pain score at discharge PACU |
p=0.0008* |
p=0.008* |
p=0.006* |
|
Opioid analgesics (IV morphine equivalents) |
p=0.293 |
p=0.451 |
p=0.4244 |
Significant p value <0.05*
Table 4: Preoperative, intraoperative and postoperative assessments of adult patients undergoing elective surgery and their preoperative anxiety scores correlations between the Visual Facial Anxiety Scale (VFAS), the Visual Analog Scale (VAS), and the Categorical Anxiety Scale (CAS) as anxiety assessment tool.
Discussion
The study focused on the comparison of the VFAS to the VAS and CAS for assessing preoperative anxiety. Results indicated high correlations among all three tools for evaluating anxiety during the immediate preoperative period, each requiring less than one minute to complete. According to published studies [40-42] the incidence of perioperative anxiety ranges from 40-95%, consistent with the finding in our current study.
Considering the significant impact of preoperative anxiety on perioperative outcomes, it remains unclear why many anesthesia practitioners do not routinely assess preoperative anxiety levels as part of their standard preoperative evaluation protocol. We would speculate that possible contributing factors include time constraints, lack of knowledge regarding simple validated assessment tools, and/or a focus on more pressing issues in the preoperative evaluation period.
A simple, rapidly administered anxiety scale as the ones we studied could easily be incorporated into anesthesia providers’ routine preoperative evaluation protocol. Implementing this practice would assure that patients with significant anxiety receive appropriate premedication, while those without acute anxiety would avoid unnecessary medications and their potential adverse effects. However, it is noteworthy that some anesthesia providers refrain from administering anxiolytic premedication, even to anxious patients, due to concerns about potential delays in discharge times [43]. Consistent with findings from other studies, [31,44,45] perioperative anxiety was observed more frequently in female patients compared to males. In contrast to earlier studies [46,47] that suggested ASA physical status influenced preoperative anxiety levels, our study did not identify any correlation between anxiety levels and ASA physical status. (Table 1). While previous authors have posited that anxiety levels may be higher in individuals with higher education levels, [48,49] our study did not observe significant differences in anxiety levels across varying educational backgrounds. It is noteworthy that a substantial majority of our study participants (84%) had more than 15 years of formal education.
Consistent with our findings, previous studies reported that patients under 40 years of age experience a notably higher incidence of preoperative anxiety compared to older age groups [21,50]. However, a conflicting study did not find a significant difference between younger and older populations [51]. Additionally, it has been documented that patients scheduled to undergo general anesthesia tend to exhibit higher preoperative anxiety levels compared to those scheduled for local or regional anesthesia [1,36]. Interestingly, our study did not identify any statistically significant association between preoperative anxiety and the proposed anesthesia technique.
Patients with a history of prior surgery reported higher preoperative anxiety levels [52,53] Interestingly, other authors have reported a higher prevalence of preoperative anxiety in patients without a history of prior surgery [54]. Our study failed to find significant differences in anxiety levels related to the type of surgery in contrast to earlier studies reporting that the type and the severity of the surgical procedure has also been alleged to be a factor associated with higher levels of preoperative anxiety [52]. Consistent with an earlier study [54] the estimated surgical time did not have a significant influence on the level of preoperative anxiety. Our study also failed to confirm earlier findings that patients receiving anesthesia for the first time have higher levels of anxiety than those with previous anesthetic experiences [54].
It has been suggested that there is a correlation between preoperative anxiety and postoperative pain [55,56]. More accurate knowledge of the patient’s level of preoperative anxiety could facilitate the anesthesiologist’s ability to predict their patient’s anesthetic and analgesic requirements [57,58]. Consistent with our results, previous studies [44,45,59-61] have reported that the most common causes of preoperative anxiety were fear of postoperative pain, awareness during surgery, complications of anesthesia and surgery, loss of control, fear about being “at the mercy” of healthcare professionals during the surgery and physical and mental harm. Future studies should examine the impact of administering anxiolytic medications to patients expressing high levels of acute anxiety on clinical outcomes.
None of the previously reported approaches to evaluating preoperative anxiety have attempted to correlate a visual (emoji-type) representation of a patient’s anxiety level with a simple numeric anxiety scale like the VFAS. In this study, the patients preferred the VFAS for evaluating preoperative anxiety level, consistent with the earlier findings of Wong and Baker using a similar visual faces scale to evaluate postoperative pain [62]. These investigators reported that while no single pain assessment scale demonstrated superiority with respect to validity and reliability; however, the facial-based pain scale was preferred by the patients. This emoji-based scale has become a commonly used pain scale in clinical practice [62,63]. In a future study, we plan to evaluate preoperative anxiety by combining the VFAS, VAS and CAS scales into a single scale called the faces anxiety scale (Figure 1d).
Where 0 indicates no anxiety and 10 indicates high level of anxiety
Where zero indicates no anxiety and 10 the highest level of anxiety
Where None indicates no anxiety and High indicates highest level of anxiety.
Study limitations
This study was performed at a single academic medical center with a limited number of anesthesiologists (89) participating. A multicenter study with a larger and more diverse population of patients and healthcare providers would have provided more generalizable results. Despite these limitations, the current study will hopefully encourage anesthesiologists and perioperative nurses to begin routinely evaluating preoperative anxiety in the preoperative period and utilize this information to optimize the use of anxiolytic premedicant drugs.
Conclusion
All three of the simple anxiety assessment tools (e.g., the VFAS, CAS and VAS) were highly correlated for assessing anxiety in the immediate preoperative period and required less than one minute to complete (~15 sec). Finally, incorporating a simple assessment anxiety tool as part of the routine preoperative evaluation process could potentially improve overall patient care by avoiding both over- and under-treatment of surgical patients with sedative-anxiolytic premedicant drugs.
References
- Celik F, Edipoglu IS. Evaluation of preoperative anxiety and fear of anesthesia using APAIS score. Eur J Med Res 23 (2018): 41.
- Buonanno P, Laiola A, Palumbo C, et al. Italian validation of the Amsterdam Preoperative Anxiety and Information Scale. Minerva Anestesiol 83 (2017): 705-711.
- Oteri V, Martinelli A, Crivellaro E, et al. The impact of preoperative anxiety on patients undergoing brain surgery: a systematic review. Neurosurg Rev 44 (2021): 3047-3057.
- Jayawardane M, Gankanda W, Gunathilake M. Prevalence of pre-operative anxiety and associated factors among a group of women undergoing gynaecological surgeries at a single unit in a tertiary care hospital in Sri Lanka 10 (2021): 74.
- Salzmann S, Rienmüller S, Kampmann S, et al. Preoperative anxiety and its association with patients' desire for support - an observational study in adults. BMC Anesthesiol 21 (2021): 149.
- Bedaso A, Ayalew M. Preoperative anxiety among adult patients undergoing elective surgery: a prospective survey at a general hospital in Ethiopia. Patient Saf Surg 13 (2019): 18.
- Jlala HA, French J, Foxall GL, et al. Effect of preoperative multimedia information on perioperative anxiety in patients undergoing procedures under regional anaesthesia. Br J Anaesth 104 (2010): 369-374.
- Ruis C, Wajer IH, Robe P, et al. Anxiety in the preoperative phase of awake brain tumor surgery. Clin Neurol Neurosurg 157 (2017): 7-10.
- Hellstadius Y, Lagergren J, Zylstra J, et al. Prevalence and predictors of anxiety and depression among esophageal cancer patients prior to surgery. Dis Esophagus 29 (2016): 1128-1134.
- Tosun B, Yava A, Acikel C. Evaluating the effects of preoperative fasting and fluid limitation. Int J Nurs Pract 21 (2015): 156-65.
- Maranets I, Kain ZN. Preoperative anxiety and intraoperative anesthetic requirements. Anesth Analg 89 (1999): 1346-1351.
- Pokharel K, Bhattarai B, Tripathi M, et al. Nepalese patients’ anxiety and concerns before surgery. J Clin Anesth 23 (2011): 372-378.
- Van Den Bosch JE, Moons KG, Bonsel GJ, et al. Does measurement of preoperative anxiety have added value for predicting postoperative nausea and vomiting? Anesth Analg 100 (2005): 1525-1532.
- Carr E, Brockbank K, Allen S, et al. Patterns and frequency of anxiety in women undergoing gynaecological surgery. J Clin Nurs 15 (2006): 341-352.
- Ocañez KLS, Kathryn McHugh R, Otto MW. A meta-analytic review of the association between anxiety sensitivity and pain. Depression and Anxiety 27 (2010): 760-767.
- Kocaturk O, Oguz E. The effect of preoperative anxiety on the incidence of perioperative bronchospasm: a prospective observational study. Medicine Science International Medical Journal 6 (2017): 746-749.
- Muire PJ, Mangum LH, Wenke JC. Time course of immune response and immunomodulation during normal and delayed healing of musculoskeletal wounds. Front Immunol 11 (2020): 10-56.
- Takagi H, Ando T, Umemoto T. ALICE (All-Literature Investigation of Cardiovascular Evidence) Group. Perioperative depression or anxiety and postoperative mortality in cardiac surgery: A systematic review and meta-analysis. Heart Vessels 32 (2017): 1458-1468.
- Hernández-Palazón J, Fuentes-García D, Falcón-Araña L, et al. Assessment of Preoperative Anxiety in Cardiac Surgery Patients Lacking a History of Anxiety: Contributing Factors and Postoperative Morbidity. J Cardiothorac Vasc Anesth 32 (2018): 236-244.
- Kelmanson IA. High anxiety in clinically healthy patients and increased QT dispersion: a meta-analysis. Eur J Prev Cardiol 21 (2014): 1568-1574.
- Kim WS, Byeon GJ, Song BJ, et al. Availability of preoperative anxiety scale as a predictive factor for hemodynamic changes during induction of anesthesia. Korean J Anesthesiol 58 (2010): 328-333.
- Gras S, Servin F, Bedairia E, et al. The effect of preoperative heart rate and anxiety on the propofol dose required for loss of consciousness. Anesth Analg 110 (2010): 89-93.
- Herd JA, Hoogwerf BJ, Barton F, et al. Heart rate and blood pressure responses to mental stress and clinical cardiovascular events in men and women after coronary artery bypass grafting: the Post Coronary Artery Bypass Graft (Post-CABG) biobehavioral study. Am Heart J 146 (2003): 273-279.
- Bayrak A, Sagiroglu G, Copuroglu E. Effects of Preoperative Anxiety on Intraoperative Hemodynamics and Postoperative Pain. J Coll Physicians Surg Pak 29 (2019): 868-873.
- Ahmetovic-Djug J, Hasukic S, Djug H, et al. Impact of Preoperative Anxiety in Patients on Hemodynamic Changes and a Dose of Anesthetic During Induction of Anesthesia. Med Arch 71 (2017): 330-333.
- Balasubramaniyan N, Rayapati DK, Puttiah RH, et al. Evaluation of Anxiety Induced Cardiovascular Response in known Hypertensive Patients Undergoing Exodontia - A Prospective Study. J Clin Diagn Res 10 (2016): ZC123-127.
- Spielberger CD, Lushene RE, Jacobs GA. Manual for the State-Trait Anxiety Inventory, STAI (Form Y) Palo Alto, Consulting Psychologists Press (1983).
- Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care & Research 63 (2011): 467-472.
- Jenkins BN, Fortier MA, Kaplan SH, et al. Development of a Short Version of the Modified Yale Preoperative Anxiety Scale. Anesth Analg 119 (2014): 643-650.
- Kain ZN, Mayes LC, Cicchetti DV, et al. The Yale Preoperative Anxiety Scale: How does it compare with a "gold standard"? Anesth Analg 85 (1997): 783-788.
- Moerman N, Van Dam FSAM, Muller MJ, et al. The Amsterdam Preoperative Anxiety and Information Scale (APAIS). Anesth Analg 82 (1996): 445-451.
- Boker A, Brownell L, Donen N. The Amsterdam preoperative anxiety and information scale provides a simple and reliable measure of preoperative anxiety. Can J Anaesth 49 (2002): 792-798.
- Zhang C, Liu X, Hu T, et al. Development and psychometric validity of the perioperative anxiety scale-7 (PAS-7). BMC Psychiatry 21 (2021): 358.
- Guerrier G, Pisanu G, Baillard C. Assessing Preoperative Anxiety: Nurses Versus Health Care Assistants. J Perianesth Nurs 36 (2021): 514-517.
- Hatipoglu Z, Kirdök O, Özcengiz D. Validity and reliability of the Turkish version of the modified Yale Preoperative Anxiety Scale. Turk J Med Sci 49 (2019): 730-737.
- Kindler CH, Harms C, Amsler F, et al. The visual analog scale allows effective measurement of preoperative anxiety and detection of patients' anesthetic concerns. Anesth Analg 90 (2000): 706-712.
- Cao X, Yumul R, Elvir Lazo OL, et al. A novel visual facial anxiety scale for assessing preoperative anxiety. Plos one 12 (2017): e0171233.
- Yumul R, Ahdout J, Goodman, et al. Assessment of Preoperative Anxiety Using Visual Facial Anxiety Scale: An Alternative to The Verbal Rating Scale? KEI Journal-Medical Research Archives 4 (2015): 1-14.
- McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol 67 (2014): 267-277.
- Rajput SK, Tiwari T, Chaudhary AK. Effect of preoperative multimedia based video information on perioperative anxiety and hemodynamic stability in patients undergoing surgery under spinal anesthesia. J Family Med Prim Care 10 (2021): 237-242.
- Erkilic E, Kesimci E, Soykut C, et al. Factors associated with preoperative anxiety levels of Turkish surgical patients: From a single center in Ankara. Patient Prefer Adherence 11 (2017): 291-296.
- Abate SM, Chekol YA, Basu B. Global prevalence and determinants of preoperative anxiety among surgical patients: A systematic review and meta-analysis. Int J Surg Open 25 (2020): 6-16.
- Walker KJ, Smith AF. Premedication for anxiety in adult day surgery. Cochrane Database Syst Rev 4 (2009): CD002192.
- Mulugeta H, Ayana M, Sintayehu M, et al. Preoperative anxiety and associated factors among adult surgical patients in Debre Markos and Felege Hiwot referral hospitals, Northwest Ethiopia. BMC Anesthesiol 18 (2018): 155.
- Li XR, Zhang WH, Williams JP, et al. A multicenter survey of perioperative anxiety in China: Pre- and postoperative associations. J Psychosom Res 147 (2021): 110528.
- Carroll JK, Cullinan E, Clarke L, et al. The role of anxiolytic premedication in reducing preoperative anxiety. Br J Nurs 21 (2012): 479-483.
- Caumo W, Schmidt AP, Schneider CN, et al. Risk factors for postoperative anxiety in adults. Anaesthesia 56 (2001): 720-728.
- Mingir T, Ervatan Z, Turgut N. Spinal Anaesthesia and Perioperative Anxiety. Turk J Anaesthesiol Reanim 42 (2014): 190-195.
- Mackenzie JW. Daycase anaesthesia and anxiety: A study of anxiety profiles amongst patients attending a day bed unit. Anaesthesia 44 (1991): 437.
- Sun GC, Hsu MC, Chia YY, et al. Effects of age and gender on intravenous midazolam premedication: a randomized double-blind study. Br J Anaesth 101 (2008): 632-639.
- Tulloch I, Rubin JS. Assessment and Management of Preoperative Anxiety. J Voice 33 (2019): 691-696.
- Badner NH, Nielson WR, Munk S, et al. Preoperative anxiety: detection and contributing factors. Can J Anaesth 37 (1990): 444-447.
- Caumo W, Schmidt AP, Schneider CN, et al. Risk factors for preoperative anxiety in adults. Acta Anaesthesiol Scand 45 (2001): 298-307.
- Yu J, Zhang Y, Yu T, et al. Preoperative Anxiety in Chinese Adult Patients Undergoing Elective Surgeries: A Multicenter Cross-Sectional Study. World J Surg 46 (2022): 2927-2938.
- Ali A, Altun D, Oguz BH, et al. The effect of preoperative anxiety on postoperative analgesia and anesthesia recovery in patients undergoing laparoscopic cholecystectomy. J Anesth 28 (2014): 222-227.
- Raichle KA, Osborne TL, Jensen MP, et al. Preoperative state anxiety, acute postoperative pain, and analgesic use in persons undergoing lower limb amputation. Clin J Pain 31 (2015): 699-706.
- Lai YL, Van Heuven A, Borire A, et al. The provision of written information and its effect on levels of pain and anxiety during electrodiagnostic studies: A randomised controlled trial. Plos one 13 (2018): e0196917.
- Sugai DY, Deptula PL, Parsa AA, et al. The importance of communication in the management of postoperative pain. Hawaii J Med Public Health 72 (2013): 180-184.
- Eberhart L, Aust H, Schuster M, et al. Preoperative anxiety in adults - A crosssectional study on specific fears and risk factors. BMC Psychiatry 20 (2020): 140.
- Sigdel S. Perioperative anxiety: a short review. Global Anesthesia and Perioperative Medicine 1 (2015): 107-108.
- Ruiz Hernández C, Gómez-Urquiza JL, Pradas-Hernández L, et al. Effectiveness of nursing interventions for preoperative anxiety in adults: A systematic review with meta-analysis. Journal of advanced nursing 77 (2021): 3274-3285.
- Wong D, Baker C. Pain in Children: Comparison of Assessment Scales. Pediatric Nursing 14 (1988): 9-17.
- Ware LJ, Epps CD, Herr K, et al. Evaluation of the Revised Faces Pain Scale, Verbal Descriptor Scale, Numeric Rating Scale, and Iowa Pain Thermometer in Older Minority Adults. Pain Management Nursing 7 (2006): 117-125.





 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 