Clinical Profile of HIV/AIDS
Abdul Mumith Ruhan*1, Fazle Rabbi Chowdhury2, Shafiqul Bari3, MM Jahangir Alam4, Parash Ullah5, Bidrum Purkayastha6, Tasnim Mahmud7
1Medical Officer, Sylhet MAG Osmani Medical College Hospital.
2Associate Professor, Bangladesh Medical University.
3Professor, Dhaka Medical College.
4Professor, Sylhet MAG Osmani Medical College.
5Senior Clinical Pathologist, Shaheed Suhrawardy Medical College Hospital, Dhaka.
6Junior Consultant, Sylhet MAG Osmani Medical College Hospital.
7Department of Public Health, North South University.
*Corresponding Author: Abdul Mumith Ruhan, Medical Officer, Sylhet MAG Osmani Medical College Hospital, Bangladesh.
Received: 27 October 2025; Accepted: 31 October 2025; Published: 06 November 2025
Article Information
Citation: Abdul Mumith Ruhan, Fazle Rabbi Chowdhury, MD. Shafiqul Bari, MM Jahangir Alam, Parash Ullah, Bidrum Purkayastha, Tasnim Mahmud. Clinical profile of HIV/AIDS. Fortune Journal of Health Sciences. 8 (2025): 1030-1035.
View / Download Pdf Share at FacebookAbstract
Background: HIV infection continues to be a major public health challenge, particularly affecting individuals in their most productive years. A clear understanding of socio-demographic characteristics, clinical manifestations, and socio-economic factors is vital for effective management and prevention.
Objective: To assess the socio-demographic profile, clinical features, and socio-economic status of HIV-infected patients attending a tertiary care center.
Methods: A cross-sectional study was conducted among 30 HIV-positive patients. Data were collected using structured interviews and medical records, covering age, sex, education, marital status, occupation, income, and clinical presentations. Descriptive statistics, including frequencies and percentages, were used to summarize the data.
Results: The patients’ ages ranged from 20 to 62 years, with a mean of 40.36 ± 10.58 years. Most were male (63.3%), married (56.7%), and middle-income (76.7%), with 36.7% being illiterate. Occupationally, foreign employment (40%) and housewives (30%) predominated. The most frequent clinical manifestations were weight loss (40%), chronic fever (33.3%), and chronic diarrhea (30%). Other features included oral/anogenital ulcers, mucocutaneous lesions, candidiasis, myalgia/arthralgia, pulmonary tuberculosis, pneumonia, and generalized itching.
Conclusion: HIV primarily affects middle-aged, economically active adults with limited education. Clinical presentations are diverse, with weight loss, fever, and diarrhea being most common. Future strategies should focus on early diagnosis, treatment adherence, psychosocial support, and the incorporation of social and religious values. Additional research in the local context is recommended to guide culturally sensitive interventions and enhance the quality of life for people living with HIV.
Keywords
<p>HIV; clinical manifestations; socio-demographic profile; socio-economic status; prevention; quality of life</p>
Article Details
Introduction
Human immunodeficiency virus (HIV) is a lentivirus that targets CD4+ T lymphocytes, macrophages and dendritic cells and, if untreated, causes progressive immune dysfunction culminating in acquired immunodeficiency syndrome (AIDS). Transmission occurs through sexual contact, contaminated blood and instruments, and mother-to-child routes; the infection is characterized by viral persistence and the establishment of latent reservoirs that complicate eradication efforts. Contemporary global guidance stresses universal testing and early initiation of antiretroviral therapy (ART) because timely diagnosis and treatment prevent immune decline and onward transmission. [1,2]. The clinical course of HIV typically follows an acute (primary) phase—often a self-limited mononucleosis-like illness—then a prolonged clinically latent period during which nonspecific symptoms may be absent, and finally a stage of symptomatic immunodeficiency with opportunistic infections and HIV-related malignancies if untreated. Common presenting features across settings include fever, weight loss, chronic diarrhea, persistent lymphadenopathy and recurrent infections such as tuberculosis and Pneumocystis jirovecii pneumonia; the timing and severity vary by host factors, co-infections and access to care. Late presentation (diagnosis with advanced disease) remains common in many Asian settings and is linked to worse outcomes. [3,4]. Diagnosis is driven by a combination of antigen/antibody immunoassays, confirmatory differentiation tests and nucleic acid testing when early infection is suspected; baseline evaluation includes CD4 count, HIV viral load, screening for hepatitis B/C, tuberculosis and other sexually transmitted infections, and resistance testing where available. Treatment philosophy has shifted to a “test-and-treat” model with integrase-based regimens favored for efficacy and tolerability; management also requires prophylaxis for opportunistic infections, prompt treatment of co-infections (notably TB in South Asia), and routine monitoring of virologic suppression and drug toxicities. Programmatic WHO guidance and regionally adapted protocols underpin these approaches. [1,5,6]. Quality of life for people living with HIV (PLHIV) is shaped by clinical, psychological and social dimensions. Even when viral suppression is achieved, PLHIV faces a higher burden of non-AIDS comorbidities (cardiovascular, metabolic, renal and neurocognitive disorders) that accompany chronic inflammation, aging, and long-term ART exposure. Mental health problems, treatment side effects, and social determinants such as poverty and food insecurity further reduce health-related quality of life (HRQoL). Interventions that combine clinical care with mental-health support, adherence counseling and social services show measurable improvements in HRQoL. [7-10].
In South Asia, including Bangladesh, the HIV epidemic remains concentrated in key populations (people who inject drugs, men who have sex with men, sex workers, and migrant workers) while overall population prevalence is comparatively low. Nevertheless, late diagnosis, high TB coinfection risk, stigma, gender-based barriers and gaps in social protection create important obstacles to care. Recent regional and country reports document persistent late presentation, psychosocial distress, and internal and external stigma that discourage testing and retention in care. In Bangladesh specifically, studies show low population prevalence but concentrated epidemics, high levels of depressive symptoms among diagnosed individuals, and stigma-related barriers to disclosure and care; integrated clinical-social programs are needed to improve outcomes. Strengthening testing, expanding community-based services, integrating TB and mental-health care, and reducing stigma through policy and public engagement are priorities for the region. [4,5,11-16]. This clinical research was conducted to know the clinical profile of HIV/AIDS.
Methods
This cross-sectional descriptive study was held in Ashar Alo society, Sylhet (an NGO working on AIDS) from June 2016 to November 2016. Adult patients (>18 years) attending Ashar Alo society with HIV infected patients (HIV 1&2 positive laboratory test) were included in this clinical research. On the other hand, patients with long-standing diabetes mellitus, disseminated tuberculosis, chronic malabsorption, irritable bowel syndrome, interstitial lung disease, congenital anomalies or psychiatric disorders were excluded from this study. According to the criteria, 30 patients were enrolled over these 5 months. Purposive sampling was employed as sampling technique in this study. Data was collected in a pre-designed data collection sheet. A detailed history and thorough examination were done in each patient. Appropriate care was taken during clinical examination so that transmission of HIV infection from patient to examiner would not occur. Before attending Ashar Alo Society, the patients were primarily diagnosed to be HIV positive from any hospital or specialist centre on the basis of HIV 1&2 laboratory test. HIV infection was further established using a commercially available ELISA kit, a rapid test kit, Combaids RS Advantage from Span Diagnostics Ltd., Surat, India.
Laboratory measurements:
Prior to attending Ashar Alo Society, the patients were primarily diagnosed to be HIV positive from any hospital or specialist centre on the basis of HIV 1&2 laboratory test. HIV infection was further established using a commercially available ELISA kit, a rapid test kit, Combaids RS Advantage from Span Diagnostics Ltd., Surat, India. Combaids RS Advantage works on the principle of Enzyme Immuno Assays (EIA) that detects antibodies to HIV-1 & HIV-2 in Human whole blood / serum / plasma with inbuilt control dot. Recombinant antigens and synthetic peptides of immunodominant epitopes are used in this technique to make high accuracy. For this examination 3-4 ml of venous blood was collected in a sterile tube without anticoagulant and it was allowed to clot at room temperature. Then the serum sample was separated after centrifugation and stored in a labeled sterile container as soon as possible to avoid haemolysis. Four full drops (0.15-0.2 ml) of specimen without any air bubble were dropped into the test kit. Appearance of a clear pink control and a detectable test band indicate positive results.
Statistical Analysis:
Data was processed manually and analyzed with the help of SPSS (Statistical Package for Social Science) Version 16.0.
Quantitative data were expressed by mean and standard deviation.
Qualitative were expressed by frequency and percentage.
Ethical Consideration:
- • Informed written consent was taken from each of the patients before taking any interview; his/her attendant was the witness. The consent form clearly described the purpose and methods of the study, confidentiality of the interviews, risks and benefits of participating in the study, their rights to participate voluntarily and to refuse at any point in time without consequences.
- • All information was collected confidentially with complete respect to the patient’s wish and without any force or pressure.
Operational definition
HIV Infection:
Prior to attending Ashar Alo Society, the patients are primarily diagnosed to be HIV positive from any hospital or specialist centre on the basis of HIV 1&2 laboratory test (sensitivity and specificity 97%). HIV infection was further established using a commercially available ELISA kit, a rapid test kit, Combaids RS Advantage from Span Diagnostics Ltd., Surat, India (sensitivity and specificity >99%) [17].
Weight loss:
>10% loss of body weight [18].
Mucocutaneous manifestations:
Any kind of lesion in the skin or mucous membrane e.g. maculopapular rash, papular pruritic eruption, fungal infection, ulceration, dry skin/icthyosis, angular cheilitis, seborrheic dermatitis, etc [19].
Oral and/or anogenital ulceration:
Any sort of ulceration in and around the oral cavity or anogenital area.
Oesophageal and/or oral candidiasis:
Fungal infections in the oral cavity and/or oesophagus presenting with pain, difficulty in chewing or swallowing.
Pharyngitis:
Infection or inflammation in the pharynx with symptoms of sore throat, pain, cough.
Pneumonia:
It includes Pneumocystis jirovecii pneumonia, bacterial pneumonia and pneumonia caused by other typical and atypical organisms.
Pulmonary tuberculosis:
Diagnosis is established on the basis of clinical presentation, biochemical and radiological findings and sputum examination [20].
Result
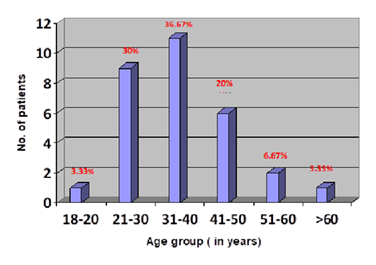
Figure 1 shows distribution of the patients regarding age group. The age of the patients with HIV infection ranged from 20 to 62 years with the mean age of 40.36 ± 10.58 years. It is evident that 11 (36.67%) patients were in the age group of 31-40 years, 9 (30.0%) patients in 21-30 years, 6 (20.0%) patients in 41-50 years, 2 (6.67%) patients were in 51-60 years. Only 1 patient each belonged to the both age groups of 18 to 20 years and above 60 years.
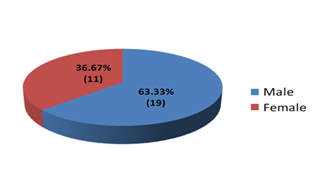
Figure 2 resembles distribution of the patients according to sex. Among the 30 patients with HIV infection majority were male. There were 19 (63.33%) male and 11 (36.67%) female with a ratio of male to female 1.73:1.
Table 1: Distribution of patients according to socio-economic status (n=30)
|
Distribution of patients according to educational status (n=30) |
||
|
Educational status |
Frequency (n) |
Percentage (%) |
|
Illiterate |
11 |
36.7 |
|
Primary |
9 |
30 |
|
Secondary |
4 |
13.3 |
|
SSC |
3 |
10 |
|
HSC |
2 |
6.7 |
|
Graduate |
1 |
3.3 |
|
Postgraduate |
0 |
0 |
|
Distribution of patients according to their marital status (n=30) |
||
|
Marital Status |
Frequency (n) |
Percentage (%) |
|
Married |
17 |
56.7 |
|
Unmarried |
13.3 |
4 |
|
Widow/er |
16.7 |
5 |
|
Divorced |
10 |
3 |
|
Separated |
3.3 |
1 |
|
Distribution of patients according to occupation (n=30) |
||
|
Occupation |
Frequency (n) |
Percentage (%) |
|
Foreign employee |
12 |
40 |
|
House wife |
9 |
30 |
|
Businessman |
2 |
6.67 |
|
Unemployed |
2 |
6.67 |
|
Commercial sex worker |
2 |
6.67 |
|
Service holder |
1 |
3.33 |
|
Student |
1 |
3.33 |
|
Day laborer |
1 |
3.33 |
|
Farmer |
0 |
0 |
|
Distribution of income group of the patients (n=30) |
||
|
Class |
Frequency (n) |
Percentage (%) |
|
Upper class |
2 |
6.7 |
|
Middle class |
23 |
76.7 |
|
Lower class |
5 |
16.7 |
Table 1 shows distribution of patients according to socio-economic status. Among the 30 patients, most were illiterate (36.7%) and had low educational attainment. Over half were married (56.7%), while others were unmarried, widowed, divorced, or separated. In terms of occupation, the majority were foreign employees (40%), followed by housewives (30%), with smaller numbers in business, unemployment, and other jobs. Most participants belonged to the middle-income group (76.7%), indicating that the study population primarily consisted of middle-class, married individuals with limited education and diverse occupational backgrounds.
Table 2: Clinical manifestations of HIV infected patients (n=30)
|
Clinical presentations |
No. of events (n) |
Percentage (%) |
|
Weight loss |
12 |
40 |
|
Mucocutaneous manifestation |
7 |
23.3 |
|
Oral and/or anogenital ulceration |
8 |
26.7 |
|
Oesophageal and/or oral candidiasis |
5 |
16.7 |
|
Pharyngitis |
2 |
6.7 |
|
Pneumonia |
1 |
3.3 |
|
Pulmonary tuberculosis |
6 |
20 |
|
Chronic diarrhoea |
9 |
30 |
|
Chronic fever |
10 |
33.3 |
|
Myalgia and/or arthralgia |
3 |
10 |
|
Generalized lymphadenopathy |
2 |
6.7 |
|
Others (generelized itching) |
4 |
13.3 |
Table 2 illustrates clinical manifestations of HIV infected patients. The most frequently occurring clinical presentation was weight loss with 12 events (40.0%). Second and third most frequent presentations were chronic fever and chronic diarrhea with number of events and percentage 10 (33.3%) and 9 (30.0%) respectively. Oral and/or anogenital ulceration was presenting feature in 8 (26.7%) patients, mucocutaneous manifestation in 7 (23.3%) patients, Oesophageal and/or oral candidiasis in 5 (16.67%) patients, myalgia and/or arthralgia in 3 (10.0%) patients. Both the generalized lymphadenopathy and pharyngitis were present in 2 (6.7%) patients. Six patients presented with pulmonary tuberculosis and 1 presented with pneumonia which were 20.0% and 3.33% of total number of patients respectively. Four (13.3%) of the patients interviewed answered about other feature, all of which were generalized itching.
Discussion
This cross-sectional descriptive clinical study over 30 adult patients attending Ashar Alo society explored the clinical profile of patients living with HIV/AIDS, aiming to identify their demographic, clinical, and socio-economic characteristics. Moreover, the variation in clinical manifestations, from asymptomatic infection to advanced immunodeficiency with opportunistic infections, underscores the diverse presentations of HIV/AIDS across different populations. In this study, the age of patients living with HIV infection ranged from 20 to 62 years, with a mean age of 40.36 ± 10.58 years. The majority of patients (36.7%) were between 31 and 40 years, followed by 30.0% in the 21–30 years group and 20.0% in the 41–50 years group. A smaller proportion (6.7%) were aged 51–60 years, while only one patient each belonged to the below 20 years and above 60 years categories. This finding is consistent with several previous studies from South Asia, which have reported that most people living with HIV are within the economically productive age group of 20–50 years, particularly concentrated between 31–40 years [21–23]. This pattern reflects increased exposure to risk behaviors among sexually active adults, emphasizing the need for targeted prevention in this age group. Moreover, majority were male (63.33%), while females accounted for 36.67%, giving a male-to-female ratio of 1.73:1 and strong evidence of male predominance in this clinical study. This male predominance is consistent with findings from several previous studies conducted in South Asia, where higher infection rates among men have been attributed to greater mobility, occupational exposure, and engagement in high-risk sexual behaviors [21-23]. However, the rising proportion of female patients observed in more recent studies indicates a gradual shift toward increased heterosexual transmission and emphasizes the need for gender-focused prevention strategies [24]. It is a matter of great disappointment that, according to this study, most of the patients had low educational attainment (36.7%). This aligns with findings from other studies in India, where illiteracy rates among HIV patients ranged from 25% to 40%, indicating a consistent trend of low educational levels in this population [25].
Regarding marital status, over half of the patients (56.7%) were married, while the remaining were unmarried, widowed, divorced, or separated. This distribution mirrors patterns observed in other clinical settings, where marriage rates among HIV patients often reflect broader societal norms [23]. In terms of occupation, the majority were foreign employees (40%), followed by housewives (30%), with smaller numbers engaged in business, unemployment, and other jobs. This occupational distribution is consistent with studies from similar settings, highlighting the diverse employment backgrounds of individuals living with HIV. Most participants (76.7%) belonged to the middle-income group, suggesting that the study population primarily consisted of middle-class, married individuals with limited education and diverse occupational backgrounds. This socio-economic profile is in line with findings from other regions, where middle-income status is prevalent among people living with HIV [21]. In this study, the most frequently reported clinical manifestation among the 30 HIV-infected patients was weight loss, observed in 12 patients (40.0%). This aligns with findings from other studies, where weight loss is commonly reported among HIV patients, often due to factors like malnutrition and opportunistic infections [26]. Chronic fever was the second most common symptom, affecting 10 patients (33.3%), followed by chronic diarrhea in 9 patients (30.0%). These symptoms are consistent with those reported in other studies, where fever and diarrhea are prevalent among HIV patients and are often associated with opportunistic infections [22]. Oral and/or anogenital ulcerations were noted in 8 patients (26.7%), and mucocutaneous manifestations were present in 7 patients (23.3%). These findings are in line with studies that highlight the occurrence of mucocutaneous lesions in HIV-infected individuals [27]. Oesophageal and/or oral candidiasis was observed in 5 patients (16.7%), which is consistent with other studies reporting oral candidiasis as a common opportunistic infection in HIV patients [28]. Pulmonary tuberculosis was diagnosed in 6 patients (20.0%), and pneumonia was identified in 1 patient (3.3%). Tuberculosis remains a leading opportunistic infection among HIV patients, as corroborated by other studies [22].
Limitation:
This study has certain limitations that should be considered. The relatively small sample size of 30 patients limits the generalizability of the findings to the broader population of individuals living with HIV. Since the study was carried out at a single healthcare facility, the results may not accurately represent patients from other regions or socio-economic backgrounds. The cross-sectional nature of the study provides only a snapshot of clinical and socio-demographic characteristics, preventing the determination of causal relationships or monitoring changes over time. Moreover, some of the data, including symptoms and socio-economic information, were self-reported, which could introduce recall or reporting bias.
Conclusion
Combating HIV requires forward-looking strategies that enhance the quality of life of affected individuals through early diagnosis, consistent treatment, and strong psychosocial support. Incorporating social and religious values can further strengthen prevention efforts by encouraging safe practices, reducing stigma, and fostering community engagement. In addition, more studies of this type should be undertaken in our country to gain a deeper understanding of the clinical and socio-demographic characteristics of HIV patients, which can inform effective and culturally appropriate interventions. A comprehensive approach that integrates medical, social, and cultural strategies is vital to curb transmission and improve overall health and well-being for people living with HIV.
References
- Dr Tedros Adhanom Ghebreyesus. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring. Recommendations for a Public Health Approach (2021).
- Helena M Swinkels, Andrew D, Nguyen Gulick et al. StatPearls. HIV and AIDS. StatPearls [Internet]. 2024.
- Chan CWH, et al. HIV Late Presenters in Asia: Management and Public Health Implications. HIV/AIDS (Auckl) 14 (2023): 9488051
- Asia and the Pacific regional profile -2024 UNAIDS Global AIDS Update (2024).
- Asia and the Pacific -2023 regional factsheet (2023)
- Jin J, Pan S, Chen J, et al. Prevalence, Risk Factors, and Clinical Outcomes with Advanced HIV Disease Among People with Newly Diagnosed HIV During the “Treat-All” Era: A Retrospective Cohort Study from Xi’an City, China. Infection and Drug Resistance 31 (2025): 2427-2438.
- Gadodia T, et al. A retrospective cross-sectional study of the clinical profile of PLWH at tertiary centres, India 16 (2024): e71954
- Arbune M, et al. Cardiovascular risk in people living with HIV - review. Heart Lung Circ (2023).
- Systematic review: Health-Related Quality of Life in People with Advanced HIV Disease. PubMed 28 (2024): 1978-1998.
- Hoang VT, Pham HT, Nguyen LT, et al. The relationship between HIV-related stigma and quality of life among HIV infected outpatients: a cross-sectional study in Vietnam. Journal of Public Health Research 13 (2024): 22799036241238667.
- Mbuagbaw L, Hajizadeh A, Wang A, et al. Overview of systematic reviews on strategies to improve treatment initiation, adherence to antiretroviral therapy and retention in care for people living with HIV: part 1. BMJ open 10 (2020): e034793.
- Global HIV guidelines and programme resources. WHO website. 2021-2024.
- UNAIDS & regional analyses: late presentation and programmatic gaps in Asia-Pacific. 2023-2024.
- Rabeya R, Alam N, Sonia ZF,et al. Depressive symptoms and their sociodemographic determinants among people living with HIV/AIDS in Bangladesh: a cross-sectional study. F1000Research 17 (2023): 239.
- Index of Stigma and Discrimination in Bangladesh. AIDS Data Hub. (Bangladesh country reports).
- Bhowmik A, Hasan M, Saha M, Saha G. Trends, Challenges, and Socioeconomic Impacts of HIV in Bangladesh (2000–2024). Sexes 6 (2025): 34.
- Boadu R, Darko G, Nortey P, Akweongo P, Sarfo B. Assessing the sensitivity and specificity of First Response HIV-1-2 test kit with whole blood and serum samples: a cross-sectional study. AIDS research and therapy 13 (2016): 9.
- Ryan DH, Yockey SR. Weight loss and improvement in comorbidity: differences at 5%, 10%, 15%, and over. Current obesity reports 6 (2017): 187-194.
- Nnoruka EN, Chukwuka JC, Anisuiba B. Correlation of mucocutaneous manifestations of HIV/AIDS infection with CD4 counts and disease progression. International journal of dermatology 46 (2007): 14-18.
- Rajendra Santosh AB, Muddana K, Bakki SR. Fungal infections of oral cavity: diagnosis, management, and association with COVID-19. SN comprehensive clinical medicine 3 (2021): 1373-1384.
- Mir MA, Ahmad PM, Siddeque MA, et al. Clinical and demographic profile of HIV/AIDS patients diagnosed at a tertiary care centre in Kashmir. J Pak Med Assoc 60 (2010): 428-431.
- Agarwal AK, Kushwah A, Verma P, et al. A cross-sectional study of demographic and clinical profile of HIV patients at ART center of tertiary care hospital. Asian J Med Sci 13 (2022): 172-179.
- Desikan P, Rangnekar A, Tiwari K, et al. Sociodemographic profile of patients attending the integrated counseling and testing center at a government super-specialty hospital in Central India. Indian J Sex Transm Dis AIDS 41 (2020): 68-72.
- Mehta SH, Gupta A, Sahay S, et al. High HIV prevalence among female sex workers and clients remains unchanged after a decade in Pune, India. J Acquir Immune Defic Syndr 69 (2015): 23-31.
- David JK, et al. The relationship between educational attainment and HIV risk among Indian women. Indian J Public Health 64 (2020): 312-318.
- Gadodia T, Sharma S, Sharma S, et al. A retrospective cross-sectional study of clinical profile of HIV patients at a tertiary care hospital in North India. Indian J Sex Transm Dis AIDS 45 (2024): 1-6.
- Pohan HT, et al. Clinical manifestation of HIV/AIDS patients in Jakarta, Indonesia. Med J Indones 13 (2004): 232-236.
- Kumar A, Chidambaram Y, Dhas CJ, et al. Clinical profile and outcomes analysis of HIV infection. HIV AIDS Rev 23 (2024): 282-289.


 Impact Factor: * 6.2
Impact Factor: * 6.2 Acceptance Rate: 76.33%
Acceptance Rate: 76.33%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 