Diaphragmatic Hernia an Uncommon Complication of Left Hemicolectomy for Colonic Adenocarcinoma
Dallas E Kramer1, Marcus Eby2*, Andrew Arndt2
1Rush Medical College, Rush University Medical Center, Illinois, United States
2Department of Cardiovascular and Thoracic Surgery, Rush University Medical Center, Illinois, United States
*Corresponding Author: Marcus Eby, Department of Cardiovascular and Thoracic Surgery, Rush University Medical Center, 1725 West Harrison Street, Suite 774, Chicago, IL, 60612, United States
Received: 06 July 2020; Accepted: 22 July 2020; Published: 09 April 2021
Article Information
Citation:
Dallas E Kramer, Marcus Eby, Andrew Arndt. Diaphragmatic Hernia an Uncommon Complication of Left Hemicolectomy for Colonic Adenocarcinoma. Journal of Surgery and Research 4 (2021): 197-201.
View / Download Pdf Share at FacebookAbstract
Background: Acquired diaphragmatic hernia is a rare complication of surgery. Treatment is surgical repair of the defect, which may be accomplished by an abdominal or thoracic approach. We report the second case of iatrogenic diaphragmatic hernia following left hemicolectomy, and the first case managed with a thoracic approach.
Case presentation: An 89-year-old male who underwent left hemicolectomy for colonic adenocarcinoma and presented to the emergency department on postoperative day (POD) 44 with repeated emesis and obstipation. Abdominal CT demonstrated a left anterior diaphragm defect with associated small bowel herniation and obstruction. The patient underwent left muscle-sparing thoracotomy with successful reduction of the herniated bowel and repair of the diaphragmatic defect.
Conclusions: Acquired diaphragmatic hernia is a rare complication of surgery. A thoracic approach may be preferred when there exists concern for extensive abdominal adhesions, such as in cases of delayed time to presentation.
Keywords
<p>Diaphragmatic hernia, Iatrogenic, Small bowel obstruction, Hemicolectomy, Thoracotomy, Thoracoscopic</p>
Article Details
Abbreviations:
CT- computed tomography; POD- post-operative day; VATS- video-assisted thoracoscopy
1. Introduction
Acquired diaphragmatic hernias may occur secondary to blunt or penetrating trauma, or iatrogenic as a complication of abdominal or thoracic surgery. There are reports of diaphragmatic hernias following colectomy, cholecystectomy, esophagectomy, gastrectomy, nephrectomy, splenectomy, trauma, and liver cyst fenestration [1-8]. We report a case of iatrogenic diaphragmatic hernia after a left hemicolectomy for colonic adenocarcinoma; the second reported case1 in our literature review and the first repaired via a thoracic approach.
2. Case Presentation
An 89-year-old male with history of atrial fibrillation, congestive heart failure, hypertension, and remote surgical history of inguinal hernia repair (>30 years ago) was diagnosed with colonic adenocarcinoma T4N0Mx of the left colic flexure. He had been admitted for flu and pneumonia and found to be anemic, which prompted colonoscopy showing a splenic flexure mass. CT confirmed a non-obstructing 6cm splenic flexure lesion and pathology demonstrated poorly differentiated adenocarcinoma. A da Vinci robot-assisted left hemicolectomy was planned. Intraoperatively the mass appeared adherent to the anterior abdominal wall and adhesions were visualized between the left colon to the sigmoid colon and left anterior abdominal wall. Adhesiolysis was performed between the sigmoid colon and abdominal wall, and the left colon was mobilized to the splenic flexure following the white line of Toldt. The lesser sac was difficult to access due to adhesions from the transverse colon to the anterior gastric body, and the procedure was converted to open to remove the specimen and successfully complete the procedure. Bleeding was present at the site of resection on the anterior abdominal wall just inferior to the diaphragm. There was no thermal injury visualized or evidence of diaphragm entry after checking with anesthesia. Fibrin sealant was placed over the site of bleeding before closure. X-ray obtained due to concern for a missing instrument showed a small right apical pneumothorax but otherwise no radiographic concerns. The post-operative course was complicated by acute kidney injury, pneumonia (treated with vancomycin), and anemia associated with painless large-volume bloody bowel movements with resolution prior to discharge on postoperative day (POD) 15. POD 44 the patient presented to the emergency department with 1 day of vomiting and lower abdominal pain. He reported 8 episodes of non-bilious, non-bloody vomiting, constipation with last bowel movement 5 days ago, and inability to pass flatus. Abdominal CT with oral contrast (Figure 1) showed a left anterior diaphragmatic hernia with associated small bowel obstruction suspicious of a closed loop morphology. He was brought to the operating room for planned flexible bronchoscopy and left video-assisted thoracoscopy (VATS) reduction and repair. Thoracoscopic access was obtained with visualization of the herniated bowel and diaphragmatic defect. Due to extensive bowel herniation, a decision was made to extend the incision and convert to a muscle-sparing thoracotomy. The bowel was determined to be viable and fully reduced into the abdomen with closure of the defect (Figure 2) and chest tube placement.
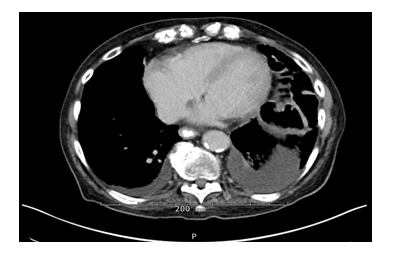
Figure 1: Chest CT with contrast POD 44 (hospital day 1) open left hemicolectomy, demonstrating left anterior diaphragmatic hernia with herniation of several loops of bowel.
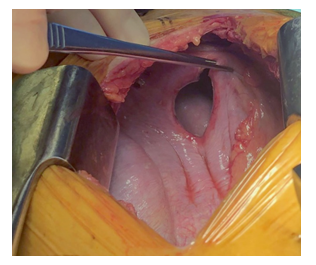
Figure 2: Surgical finding with thoracoctomy (superior at left). The diaphragmatic defect can be visualized following assessment of viability and subsequent reduction of incarcerated small bowel.
3. Discussion
The clinical presentations of diaphragmic hernias vary depending of which organs are involved. Patients may be asymptomatic or present with systemic signs, chest pain, epigastric pain, nausea, vomiting, bowel obstruction, or respiratory distress. The hernia may become symptomatic in the near post-operative period or several years after the primary injury with the longest time to presentation reported as 35 years [9]. The exact pathogenesis of this case remains unknown, as no defect in the diaphragm was observed during the initial surgery for left hemicolectomy. However, previous cases of iatrogenic diaphragmatic hernias have implicated electrocautery or ultrasonic scalpel as the likely culprit [1-3]. Pathogenesis of this delayed diaphragmatic hernia is unclear. Incidental electrocautery injury to the diaphragm may have occurred during mobilization of the large mass at the splenic flexure and adhesiolysis along the anterior abdominal wall while in close proximity to the diaphragm. Thermal injury may have weakened and created an area of vulnerability which was not easily identified by thermal injury or obvious defect. Postoperative positive end-expiratory pressure ventilation likely prevented immediate progression of a defect due to an increased intrathoracic pressure. Following extubation, increased intrabdominal pressure applied to a point of weakness likely lead to progressive enlargement of a diaphragmatic defect and eventual herniation. Surgery is the definitive treatment once a diaphragmatic hernia is identified, and repair may be accomplished via an abdominal or thoracic approach. The approach taken depends of the location of the defect, adhesions associated with previous surgical history, and surgeon preference. A previous case of diaphragmatic hernia following colectomy used a laparoscopic approach for repair on the POD 11 [1]. Transabdominal approach was optimal in their case given the patient stability and the recency of the initial surgery [1]. For our case, a thoracoscopic approach was taken. Time to presentation following initial abdominal surgery warranted sufficient concern for (1) intrabdominal adhesions from previous surgery that would require significant lysis and (2) possible intrathoracic adhesions to the herniated structures which would require lysis in order to mobilize and reduce the bowel [1-2].
4. Conclusion
We report the case of an iatrogenic diaphragmatic hernia with small bowel obstruction which presented 44 days after left hemicolectomy for colonic adenocarcinoma which was repaired via muscle-sparing left thoracotomy. Iatrogenic diaphragmatic hernia is a rare post-surgical complication which may be repaired by either abdominal or thoracic approach. A thoracic approach may be preferred in cases with concern for extensive intrabdominal adhesions.
Disclosure Statement
No funding was received in support of this work. The authors have no relevant conflict of interest to disclose. There are no competing interests. We have abided by all institution ethical requirements.
Acknowledgements
None.
References
- Paolo Dell'Abate, Elisa Bertocchi, Raffaele Dalla Valle, et al. Iatrogenic diaphragmatic hernia following laparoscopic left colectomy for splenic flexure cancer. Ann Ital Chir 87 (2016): S2239253X16025937.
- Shohei Takaichi, Tsuyoshi Takahashi, Soichiro Funaki, et al. Laparoscopic repair of an incarcerated diaphragmatic hernia after right hepatectomy for hepatic injury: a case report. Surgical Case Reports 4 (2018): 135.
- Youngjin Suh, Jun Hyun Lee, Haemyung Jeon, et al. Late onset iatrogenic diaphragmatic hernia after laparoscopy-assisted total gastrectomy for gastric cancer. J Gastric Cancer 12 (2012): 49-52.
- De Meijer VE, Vles WJ, Kats E, et al. Iatrogenic diaphragmatic hernia complicating nephrectomy: top-down or bottom-up?. Hernia 12 (2008): 655.
- German Mínguez Ruiz, Luis J García Florez, Dario Arias Pacheco R, et al. Post-nephrectomy diaphragmatic hernia. Increase suspicion and decrease morbi-mortality: two cases report. J Surgical Case Reports 8 (2018): 1-4.
- Fitzgerald C, McCormack O, Awan F, et al. Incarcerated thoracic gastric herniation after nephrectomy: A report of two cases. Case Rep Surg (2013): 1-4.
- Goi G, Callegaro D, Villa R, et al. Large-bowel obstruction as a result of occult diaphragmatic hernia 11 years after injuries. Ann Ital Chir 83 (2012): 425-428.
- Johnson CD, Ellis H. Acquired hernias of the diaphragm. Postgrad Med J 64 (1988): 317-321.
- Soufi M, Meillat H, Le Treut YP. Right diaphragmatic iatrogenic hernia after laparoscopic fenestration of a liver cyst: Report of a case and review of literature. World J Emerg Surg 8 (2013): 2.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 