Early Enteral Nutrition in Cases of Perforation of the Gut with Peritonitis
Siddarth Jain1, Yogesh Kailasi1, Ashutosh Garg2*, Shivam Patidar1, Apoorvi Banerjee1
1Department of Surgery, Sanjay Gandhi Memorial Hospital, Hari Bhushan Nagar, Rewa, Madhya Pradesh 486001, India
2Department of Anesthesiology, Sanjay Gandhi Memorial Hospital, Hari Bhushan Nagar, Rewa, Madhya Pradesh 486001, India
*Corresponding Author: Ashutosh Garg, Department of Anesthesiology, Sanjay Gandhi Memorial Hospital, Hari Bhushan Nagar, Rewa, Madhya Pradesh 486001, India
Received: 18 July 2025; Accepted: 27 July 2025; Published: 18 August 2025
Article Information
Citation: Siddarth Jain, Yogesh Kailasi, Ashutosh Garg, Shivam Patidar, Apoorvi Banerjee. Early Enteral Nutrition in Cases of Perforation of the Gut with Peritonitis. Journal of Surgery and Research. 8 (2025): 410-415.
View / Download Pdf Share at FacebookAbstract
Background: Gastro-duodenal perforation is a common surgical emergency requiring prompt surgical intervention, typically via omental patch repair. Traditional postoperative management involves delayed enteral nutrition to prevent stress on the gut; however, recent evidence supports early enteral feeding (EEF) to enhance recovery.
Objective: To evaluate the safety, feasibility, and outcomes of Early Enteral Feeding via nasojejunal (NJ) tube in patients undergoing surgery for gastro/duodenal perforation with peritonitis.
Methods: A prospective study was conducted on 50 patients diagnosed with gastrointestinal perforation and peritonitis, randomized into two groups: 25 received EEF (within 48 hours postoperatively via NJ tube), and 25 received Late Enteral Feeding (LEF) after return of bowel function (POD 6–8). Postoperative clinical and biochemical parameters were monitored on POD 3 and POD 7. Statistical analysis was performed using SPSS v20.
Results: The EEF group demonstrated significantly faster return of bowel function, reduced duration of ileus, and shorter hospital stays compared to the LEF group (p<0.05). Improvements in pulse rate, WBC count, serum albumin, and other vital parameters were observed earlier in the EEF group. The incidence of surgical site infection was lower in the EEF group (24% vs. 40%), although not statistically significant (p>0.05). No differences in mortality were observed between the groups.
Conclusion: Early enteral feeding via nasojejunal tube is a safe and effective strategy in patients with gastro/duodenal perforations. It accelerates recovery, reduces postoperative complications, shortens hospital stays, and is cost-effective without increasing mortality risk. Incorporating EEF into postoperative care protocols may enhance patient outcomes in emergency gastrointestinal surgeries.
Keywords
<p>Perforation, Enteral Nutrition, Peritonitis, Early enteral feeding (EEF), Surgical emergency</p>
Article Details
Introduction
Perforation of the gastrointestinal tract is a common surgical emergency that often presents with severe peritonitis and sepsis. These patients typically require urgent surgical intervention, most commonly managed by omental patch closure [1]. Postoperatively, patients are monitored for stabilization of vital signs, return of bowel function, and improvements in biochemical parameters to guide the timing of oral feeding [2].
Traditionally, early oral intake was avoided due to concerns that it might interfere with wound healing at the perforation site or prolong postoperative ileus [3]. As a result, patients were often kept nil per oral (NPO) for 5–7 days until bowel sounds returned or flatus was passed [4]. However, this approach has recently come under scrutiny. Prolonged fasting may delay recovery and contribute to caloric deficits during a critical period of healing.
The rationale behind withholding enteral nutrition after gastrointestinal surgery is to provide rest to the gut, thereby promoting healing. During this period, patients are maintained on intravenous fluids and nutrition tailored to their biochemical and clinical status [5,6]. Nevertheless, intravenous supplementation cannot fully replicate the physiological benefits of enteral nutrition, especially in correcting metabolic imbalances. Additionally, the absence of enteral feeding can impair gut-associated immunity and promote a negative nitrogen balance, both of which can adversely affect recovery [7].
Recent studies in abdominal surgery suggest that early enteral feeding is safe and may improve outcomes by enhancing recovery and reducing hospital stay [8]. Various protocols exist for initiating early postoperative feeding, depending on patient tolerance and surgical factors.
Given these considerations, this study aims to evaluate the outcomes of early enteral nutrition in patients with gut perforation complicated by peritonitis.
Materials and Methods
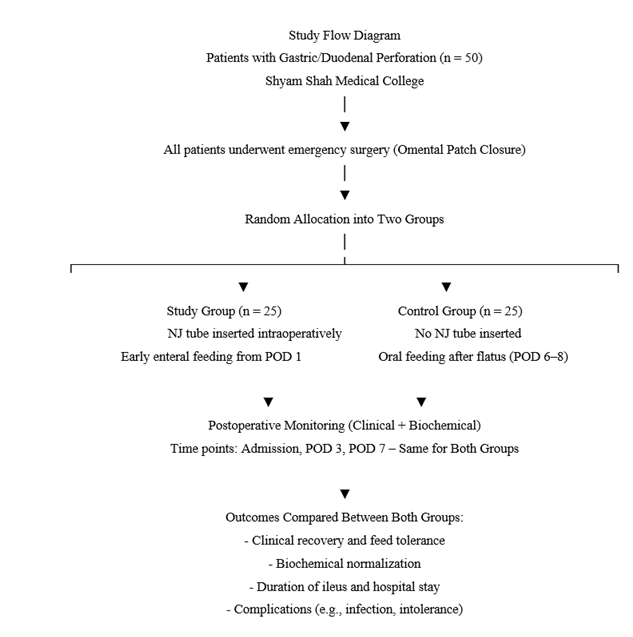
This prospective, comparative study was conducted at Shyam Shah Medical College, Rewa, during the year 2024. A total of 50 patients diagnosed with gastric or duodenal perforation and undergoing emergency surgical repair were enrolled. Patients were randomly allocated into two groups of 25 each:
- • Study Group (n = 25): Received early enteral feeding (EEF) via nasojejunal (NJ) tube inserted intraoperatively.
- • Control Group (n = 25): Received late enteral feeding (LEF), started only after the appearance of bowel sounds and passage of flatus, typically on postoperative day (POD) 6–8.
Eligibility Criteria
- • Inclusion: Adults diagnosed with gastric/duodenal perforation, undergoing omental patch repair.
- • Exclusion: Patients with perforation due to malignancy, severe shock, bowel ischemia, or with contraindications to enteral feeding.
Preoperative and Intraoperative Care
All patients underwent standard preoperative evaluation. Emergency omental patch closure was performed under general anesthesia. In the study group, a nasojejunal tube was positioned during surgery under direct vision.
Postoperative Management
- • In the study group, enteral feeding was initiated through the NJ tube on POD 1. Feeds started with oral rehydration solution (ORS) at 30 mL/hour and were gradually advanced to include:
- • Boiled milk
- • Protein supplements
- • Starch preparations
- • Egg white with milk
- • Cereal-based feeds
- • Multivitamin syrups
Feed intolerance (e.g., abdominal distension, ileus, vomiting) was managed by withholding feeds for 24 hours, followed by cautious reintroduction. Prokinetics were administered as needed.
- • In the control group, oral feeds were initiated after passage of flatus, between POD 6 and 8, following conventional management.
Monitoring and Data Collection
- • Clinical parameters: Pulse rate, blood pressure, respiratory rate
- • Biochemical parameters: Hemoglobin (Hb), total leukocyte count (WBC), serum urea, creatinine, sodium, potassium, and albumin
- • Assessment timepoints: At admission, POD 3, and POD 7
A structured proforma was used to collect demographic details, comorbidities, perforation characteristics, and time to presentation. Outcomes such as feed tolerance, time to oral intake, duration of ileus, length of hospital stay, and postoperative complications were documented.
Surgical Intervention
All patients underwent omental patch closure of the perforation. Correct placement of the NJ tube was confirmed intraoperatively in the study group. The control group did not receive NJ tube placement.
Observation and Results
Data were analyzed using SPSS version 20.0, while Microsoft Excel was used for managing empirical data. Categorical variables were summarized using frequency distributions and percentages, while numerical variables were expressed as mean (± standard deviation). Appropriate statistical tests were applied to assess associations between categorical variables, and a p-value of less than 0.05 was considered statistically significant.
The frequency distribution showed that the majority of participants were male. However, there was no statistically significant difference in the gender distribution between the experimental and control groups (P > 0.05). Similarly, the mean age of patients in both groups was approximately 49 ± 15 years, with no significant difference between the groups (P > 0.05). The duration of perforation also did not significantly differ between the two groups.
Hemodynamic parameters—including systolic blood pressure, diastolic blood pressure, and respiratory rate—did not show statistically significant differences between the experimental and control groups (P > 0.05). However, pulse rate was significantly lower in the experimental group (P < 0.05).
In terms of biochemical parameters, there were no significant differences between the groups for hemoglobin, urea, creatinine, serum albumin, sodium, and potassium (P > 0.05). However, white blood cell (WBC) count was significantly lower in the experimental group (P < 0.05), indicating a possible reduction in systemic inflammation.
Although most hemodynamic and biochemical parameters were statistically similar between the two groups, patients in the experimental group showed favorable trends: they had lower pulse rate, respiratory rate, and WBC counts, as well as higher hemoglobin, serum albumin, and sodium levels compared to the control group.
Statistically significant differences were observed between the experimental and control groups regarding the duration of ileus, time to initiation of feeds, and length of hospital stay (P < 0.05). These findings suggest that early enteral nutrition may contribute to improved postoperative recovery.
Regarding surgical site infections, no statistically significant difference was found between the two groups (P > 0.05). The incidence was 40% in the control group compared to 24% in the experimental group.
|
Variable |
Experimental Group (n = 25) |
Control Group (n = 25) |
P-value |
|
Mean Age (years) |
49 ± 15 |
50 ± 14 |
>0.05 |
|
Male Gender (%) |
68% (17) |
72% (18) |
>0.05 |
|
Duration of Perforation (hrs) |
28 ± 6 |
30 ± 5 |
>0.05 |
Table 1: Demographic parameters.
|
Parameter |
Experimental Group (Mean ± SD) |
Control Group (Mean ± SD) |
P-value |
|
Systolic BP (mmHg) |
112 ± 10 |
110 ± 11 |
>0.05 |
|
Diastolic BP (mmHg) |
72 ± 7 |
70 ± 8 |
>0.05 |
|
Pulse Rate (beats/min) |
82 ± 6 |
90 ± 7 |
<0.05 |
|
Respiratory Rate (/min) |
18 ± 2 |
20 ± 3 |
>0.05 |
Table 2: Hemodynamic parameters (Post operative day 1).
|
Parameter |
Experimental Group (Mean ± SD) |
Control Group (Mean ± SD) |
P-value |
|
Hemoglobin (g/dL) |
12.2 ± 1.1 |
11.5 ± 1.2 |
>0.05 |
|
WBC (×10³/µL) |
10.5 ± 1.8 |
12.2 ± 2.0 |
<0.05 |
|
Urea (mg/dL) |
38 ± 6 |
40 ± 7 |
>0.05 |
|
Creatinine (mg/dL) |
1.0 ± 0.2 |
1.1 ± 0.3 |
>0.05 |
|
Serum Albumin (g/dL) |
3.8 ± 0.4 |
3.5 ± 0.3 |
>0.05 |
|
Sodium (mEq/L) |
138 ± 3 |
135 ± 4 |
>0.05 |
|
Potassium (mEq/L) |
4.1 ± 0.3 |
4.0 ± 0.4 |
>0.05 |
Table 3: Biochemical parameters (Post operative day 1).
|
Outcome Variable |
Experimental Group |
Control Group |
P-value |
|
Duration of Ileus (days) |
2.2 ± 0.6 |
3.5 ± 0.8 |
<0.05 |
|
Time to Start Feeds (days) |
2.0 ± 0.5 |
4.5 ± 1.0 |
<0.05 |
|
Duration of Hospital Stay (days) |
6.5 ± 1.2 |
9.0 ± 1.5 |
<0.05 |
|
Surgical Site Infection (%) |
24% (6) |
40% (10) |
>0.05 |
Table 4: Clinical outcomes.
|
Variable |
Post-op Day |
Experimental Group (Mean ± SD) |
Control Group (Mean ± SD) |
P-value |
|
Pulse Rate (beats/min) |
Day 3 |
80 ± 5 |
88 ± 6 |
<0.05 |
|
Day 7 |
76 ± 4 |
84 ± 5 |
<0.05 |
|
|
Respiratory Rate (/min) |
Day 3 |
18 ± 2 |
20 ± 2 |
<0.05 |
|
Day 7 |
16 ± 2 |
18 ± 2 |
<0.05 |
|
|
Duration of Ileus (days) |
— |
2.2 ± 0.6 |
3.5 ± 0.8 |
<0.05 |
|
Time to Start Feeds (days) |
— |
2.0 ± 0.5 |
4.5 ± 1.0 |
<0.05 |
|
Hospital Stay (days) |
— |
6.5 ± 1.2 |
9.0 ± 1.5 |
<0.05 |
Table 5: Clinical Recovery Indicators (Postoperative Days 3 and 7).
|
Parameter |
Post-op Day |
Experimental Group (Mean ± SD) |
Control Group (Mean ± SD) |
P-value |
|
Hemoglobin (g/dL) |
Day 3 |
12.0 ± 1.0 |
11.4 ± 1.2 |
>0.05 |
|
Day 7 |
12.5 ± 1.1 |
11.6 ± 1.3 |
>0.05 |
|
|
WBC (×10³/µL) |
Day 3 |
10.0 ± 1.5 |
12.0 ± 1.8 |
<0.05 |
|
Day 7 |
8.5 ± 1.2 |
10.5 ± 1.6 |
<0.05 |
|
|
Serum Albumin (g/dL) |
Day 3 |
3.7 ± 0.3 |
3.4 ± 0.3 |
>0.05 |
|
Day 7 |
4.0 ± 0.4 |
3.5 ± 0.4 |
<0.05 |
|
|
Sodium (mEq/L) |
Day 3 |
137 ± 3 |
135 ± 4 |
>0.05 |
|
Day 7 |
138 ± 2 |
135 ± 3 |
<0.05 |
|
|
Wound Infection (%) |
Day 7 |
24% (6 patients) |
40% (10 patients) |
>0.05 |
Table 6: Biochemical and Immunological Parameters (Postoperative Days 3 and 7).
These tables 5 and 6 highlight the impact of early enteral nutrition on patient recovery, with improvements seen in vitals, inflammation (WBC), nutrition (albumin), and recovery time.
Discussion
Gastro-duodenal perforation is a common surgical emergency presenting with acute abdomen and requires prompt surgical intervention. The omental patch repair remains the universally accepted procedure for the management of such perforations. Despite adequate surgical and medical care, postoperative complications such as sepsis and mortality remain significant in cases of perforative peritonitis [1]. In our clinical setup, gastro-duodenal perforations are frequently encountered, and this study was conducted to evaluate the safety and efficacy of Early Enteral Feeding (EEF) via a nasojejunal tube in such patients. Our findings align with previous evidence and confirm that EEF is a safe, feasible, and beneficial strategy for postoperative nutritional support in emergency gastrointestinal surgery [1,2]. In this study, none of the patients receiving EEF showed intolerance to feeding, confirming its tolerability. Patients in the EEF group exhibited faster normalization of vital signs and earlier resolution of systemic inflammation. Notably, pulse rate and respiratory rate were significantly lower in the EEF group on both postoperative days 3 and 7 (P < 0.05), suggesting improved hemodynamic stability and reduced systemic stress. These findings are consistent with earlier reports indicating improved recovery and fewer complications with early feeding [6,7,10]. Biochemical parameters also showed favorable trends in the EEF group. WBC counts were significantly lower, indicating faster resolution of infection or inflammation. Additionally, serum albumin levels were significantly higher by day 7 (P < 0.05), reflecting improved nutritional absorption and metabolic status. Similar benefits of early jejunal feeding were reported in a study by Singh et al. [2,16]. The clinical outcomes further reinforce the advantages of EEF. Patients receiving early feeding had a shorter duration of ileus, earlier initiation of oral intake (2.0 ± 0.5 vs. 4.5 ± 1.0 days), and reduced hospital stay (6.5 ± 1.2 vs. 9.0 ± 1.5 days), all statistically significant (P < 0.05). These findings are in agreement with Lee et al. [1] and Moore et al. [6], who observed quicker recovery, early return of bowel function, and improved postoperative outcomes with early feeding practices.While the incidence of surgical site infection was lower in the EEF group (24% vs. 40%), the difference was not statistically significant (P > 0.05). However, the trend suggests that EEF may help reduce infectious complications by preserving mucosal immunity and preventing bacterial translocation—a benefit also emphasized in the study by Lewis et al. [7,20]. Importantly, no mortality was reported in either group, and the safety profile of EEF was excellent. These results are consistent with Malhotra et al. [17], who found no increased risk of mortality with early feeding and highlighted its cost-effectiveness.
Summary
Our study supports the conclusion that Early Enteral Feeding in patients undergoing emergency surgery for gastro-duodenal perforations leads to faster recovery, better nutritional and inflammatory profiles, shorter hospital stay, and potentially fewer complications, without increasing morbidity or mortality. This approach also offers economic benefits through reduced ICU and hospital utilization. These observations reinforce the shift in modern surgical practice toward early postoperative feeding even in emergency settings [3,4,5,8,9,11-15,18,19,21].
Conclusion
Early Enteral feeding is a safe and effective intervention among Gastro/ Duodenal perforation patients following surgical repair of the perforation in avoiding post-surgical nutrition of the patients. NasoJejunal tube placement is a easy and safe method for administering enteral feeds in post operative patients. Early enteral feeding has a better outcome in patients operated for gastroduodenal perforation than conventional feeding of postoperative patients. Patients who were fed early through enteral route showed earlier improvement in both clinical and biochemical parameters than the other group of patients who were fed only after passing flatus on POD 6-8.The long stay at the ICU is shortened in Early Enteral fed group. Also early enteral fed group showed earlier bowel movements and early passage of flatus and also early removal of Ryle’s tube than the control group. Post operative major complications are evidently reduced in enteral fed group compared to the control group. The length of hospital stay is shortened in the enteral fed group. Hence the cost of medical expenses is grossly reduced among enteral fed group both directly and indirectly. Delay in starting orals in LEF group due to any other complications necessitated total parenteral nutrition which in EEF group is not needed, hence it is cost effective Although the complication rates are lower in enteral fed group there is no significant reduction in mortality compared to the control group. In any patient with Gastroduodenal perforation starting early enteral feeding via NJ tube is a safer and effective option which has direct impact on the outcome of the patient both in recovery and in preventing postoperative complications
References
- Shamaki GR, Markson F, Soji-Ayoade D, et al. Peripheral Artery Disease: A Comprehensive Updated Review. Curr Probl Cardiol 47 (2022): 101082.
- Rodriguez Alvarez AA, Cieri IF, Morrow KL, et al. Association of age on thromboelastography coagulation profiles among elderly patients with peripheral arterial disease. J Vasc Surg 82 (2025): 173-179.
- Rodriguez Alvarez AA, Patel SS, Cieri IF, et al. Single versus dual antiplatelet therapy impact on coagulation/thrombosis post-PAD revascularization. Sci Prog 108 (2025).
- Bates KJ, Moore MM, Cibotti-Sun M. 2024 Lower Extremity Peripheral Artery Disease Guideline-at-a-Glance. J Am Coll Cardiol 83(2024): 2605-2609.
- Godier A, Albaladejo P. Management of bleeding events associated with antiplatelet therapy: Evidence, uncertainties, and pitfalls. J Clin Med 9 (2020): 1-11.
- Whyte CS, Brodmann M, Schmaier A, et al. Antithrombotic Therapy in Peripheral Arterial Disease 9 (2022): 927645.
- Carciotto G, Costa F, Garcia-Ruiz V, et al. Individualization of Duration of Dual Antiplatelet Therapy after Coronary Stenting: A Comprehensive, Evidence-Based Review. J Clin Med 12 (2023).
- Majumdar M, Hall RP, Feldman Z, et al. Predicting Arterial Thrombotic Events Following Peripheral Revascularization Using Objective Viscoelastic Data. J Am Heart Assoc 12 (2023): e027790.
- Suarez Ferreira S, Agrawal A, Lee I, et al. The Use of Clot Strength as a Predictor of Thrombosis in Peripheral Artery Disease. Ann Vasc Surg 109 (2024): 273-283.
- RStudio Team. R Studio: Integrated Development for R (2023).
- Tian L, Gao X, Yang J, et al. Association of Adenosine Diphosphate-Induced Platelet Maximum Amplitude With Postoperative Bleeding and Blood Transfusions in Patients Undergoing Coronary Artery Bypass Grafting. J Cardiothorac Vasc Anesth 35 (2021): 421-428.
- Alghamdi AA, Moussa F, Fremes SE. Does the use of preoperative aspirin increase the risk of bleeding in patients undergoing coronary artery bypass grafting surgery? Systematic review and meta-analysis. J Card Surg 22 (2007): 247-256.
- Bhatt DL, Fox KAA, Hacke W, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med 354 (2006): 1706-1717.
- Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361 (2009): 1045-1057.
- Bonaca MP, Bhatt DL, Cohen M, et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med 372 (2015): 1791-1800.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 