Evaluate the results of Noncemented Total Hip Replacement (THR)
Md. Tofayel Hossain1*, Razib Ahmed2, Maftun Ahmed3, Nitya Ranjan Balo4, Nurul Alam Siddique5
1Associate Professor, Department of Orthopaedic Surgery, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
2Junior Consultant, Department of Orthopaedic Surgery, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
3Assistant Register, Orthopaedic Surgery, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
4Assistant Register, Orthopaedic Surgery, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
5Junior Consultant, Department of Orthopaedic Surgery, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
*Corresponding Author: Dr. Md. Tofayel Hossain, Associate Professor, Department of Orthopaedic Surgery, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh
Received: 21 January 2021; Accepted: 26 February 2021; Published: 03 May 2021
Article Information
Citation: Md. Tofayel Hossain, Razib Ahmed, Maftun Ahmed, Nitya Ranjan Balo, Nurul Alam Siddique. Evaluate the results of Noncemented Total Hip Replacement (THR). Journal of Surgery and Research 4 (2021): 248-254.
View / Download Pdf Share at FacebookAbstract
Introduction: Total Hip Replacement is one of the most successful orthopaedic procedures performed now-a-days. A British orthopaedic surgeon named Charnley first introduced with this treatment. A noncemented joint prosthesis, sometimes called a press-fit prosthesis, is specially textured to allow the bone to grow onto it and adhere to it over time.
Aim of the study: The study aims to determine the results and the complications associated with non-cemented total hip replacement (THR).
Methods: This cross-sectional study was conducted in the Department of Orthopaedic Surgery, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh during the period from February 2016 to February 2018. Sample size was 35. Statistical analysis of the results was done by computer software devised in the statistical packages for social scientist (SPSS-25) and MS excel-16.
Results: In total 35 patients in this cross-sectional study from the total of 35 patients we found most of the patients were male 29(82.86%) and female 6(17.14%). Most of the patients found in 31-40 age group 14(40.00%), then 41-50 and that was 11(31.43%) respectively 5(14.29%) found in 21-30, 11(31.43%) in 41-50 and 4(11.43%) in >61. So most of them found excellent on the score of 90-100, 20(57.14%), then 11(31.4%) was 80-89 score as good, 3(8.6%) found in 70-79 score fair and below <70 score found 1(2.9%) as poor.
Conclusion: There is many reasons that may have caused surgeons in the past to move away from the use of cemented implants have been found to be unwarranted and the evidence does not support the increasing using of noncemented implants. In particular, the risk of mortality in cemented THA has not been found to be higher than noncemented THA.
Keywords
<p>Noncemented, Orthopaedic procedures, Total hip replacement (THR)</p>
Article Details
1. Introduction
Total Hip Replacement is one of the most successful orthopaedic procedures performed now-a-days, as a form of treatment for various hip pathologies [1]. Now this is widely considered as “operation of the 20th century” [2]. Sir John Charnley, a British orthopaedic surgeon, developed the fundamental principles of the artificial hip and is credited as the father of THR [1]. Charnley’s low friction Replacement, acrylic cement became standard for femoral component fixation. Charnley systematically promoted THR, based on the concept of low friction Replacement by: (1) fixation with bone cement; (2) adoption of a 22-mm femoral head; (3) adoption of ultrahigh molecular weight polyethylene (UHMWPE); and (4) preparation of a manual of the surgical procedure [1]. This procedure works as an option for nearly all patients with diseases of the hip that cause chronic discomfort and significant functional impairment. Patient with unremitting pain and irreversibly damaged joint is an ideal candidate for total hip replacement [3, 4]. For a long time, the failures of cemented THR were attributed to bone cement, and were called “cement disease”. This has motivated the orthopaedic surgeons to develop non-cemented THR [5]. Bobyn JD and Galante J first introduced the concepts of noncemented replacement, had press fit and bone integration as forms of fixation between the bone and the implant [6,7]. This mode of fixation is known as biological fixation.
Figures 1-3 have been taken from study population. The development of circumferentially coated non-cemented implants which allow bone to grow into or onto the prosthesis has led to improved implant survival rate and supports their growing use. The advantages of noncemented femoral components include a reduced risk of cement-related cardiovascular and thromboembolic complications, the possibility of biological fixation, the minimisation of stress shielding of the proximal femur and potential of extended implant survival [8-13]. The study aims to determine the results and the complications associated with noncemented total hip replacement (THR).
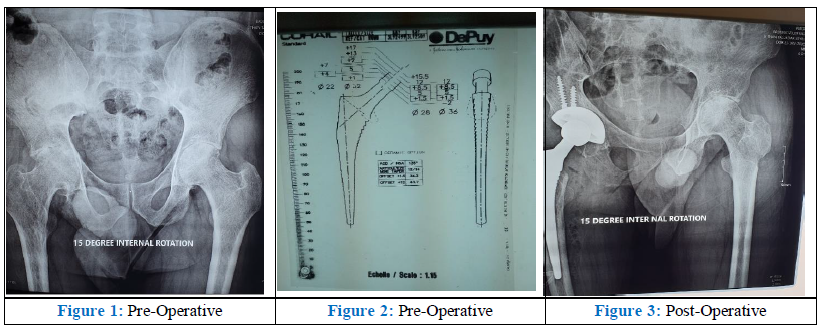
Figure 1: Pre-Operative Figure 2: Pre-Operative Figure 3: Post-Operative
2. Objectives
To goal was to observe the evaluation of outcome of noncemented total hip replacement (THR). To evaluate the results of long term and short term follow up associated with noncemented THR. To find out the complications associated with THR.
3. Methodology and Materials
This was a cross-sectional study and was conducted in the department of orthopaedic surgery, National Institute of Traumatology and Orthopedic Rehabilitation (NITOR), Dhaka, Bangladesh during the period from February 2016 to January 2019. The included patients were selected based on the history of noncemented total hip replacement operation and came for follow-up after surgery. There selected 35 patients for our study. Patients were in the age of 20 to more than 60 aged. All patients followed for minimum one year and maximum two years. The periodic assessment was defined based on Modified Harris Hip Scoring system and the follow up of the patients were collected radiologically in accordance with X rays at 6 weeks, 3 months, 6 months, 1 year and 2 year follow up data. All the primary data were compiled on a master chart first, then organized by using scientific calculator and standard statistical formula. Percentage was calculated to find out the proportion of the findings. After that statistical analysis of the results was done by computer software devised in the statistical packages for social scientist (SPSS-10) and MS excel-16.
4. Results
In this cross-sectional study from the total of 35 patients we found most of the patients were male 29 (82.86%) and female 6 (17.14%). Most of the patients found in 31-40 age group 14 (40.00%), then 41-50 and that was 11 (31.43%) respectively 5 (14.29%) found in 21-30, 11 (31.43%) in 41-50 and 4 (11.43%) in >61 (Table 1). Based to the distribution of the study patients according to the complications in follow up sessions. Most of the patients Loose acetabular in after 3 months 11 (45.31%) then in Loose stem 19 (54.31%), Unstable 9 (25.71%), Infection 6 (17.14%), Pain 26 (74.29%) and Femoral fracture 13 (37.14%). After 6 months Loose acetabular 7 (20.00%), Loose stem 2 (5.71%), Unstable 0 (0.00%), Infection 1 (2.86%), Pain 11 (31.43%), and Femoral fracture 3 (8.57%) (Table 2) Then the study from Modified Harris Hip Score. So most of them found excellent on the score of 90-100, 20 (57.14%), then 11 (31.4%) was 80-89 score as good, 3 (8.6%) found in 70-79 score fair and bellow <70 score found 1 (2.9%) as poor (Figure 1).
|
Age |
Male |
Female |
||
|
n |
% |
n |
% |
|
|
20-29 |
5 |
14.29 |
0 |
0 |
|
30-39 |
10 |
28.57 |
3 |
8.57 |
|
40-49 |
9 |
25.71 |
2 |
5.71 |
|
50-59 |
4 |
11.43 |
1 |
2.86 |
|
>60 |
1 |
2.86 |
0 |
0 |
Table 1: Distribution of the study population by Age and Sex (n=35)
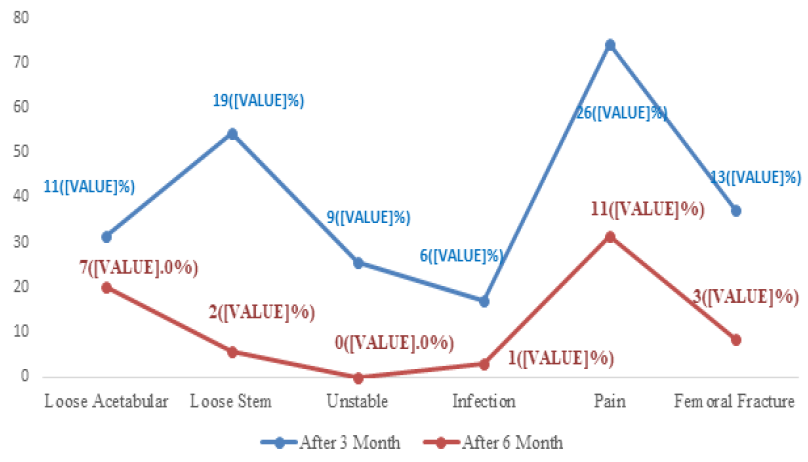
Figure 4: Distribute the study patients according to the complications in follow up sessions (n=35)
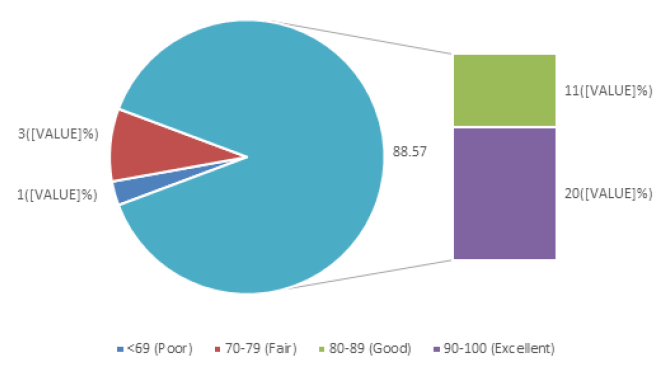
Figure 5: Outcome of the study patients in modified Harris Hip Score (n=35)
5. Discussion
The present study was aimed at evaluating the results of noncemented total hip replacement in Bangladesh population, performed at our hospital involving a controlled preoperative and postoperative follow up. From this study, we have concluded that operative treatment for various hip disorders in the form of noncemented total hip replacement has helped in alleviation of intractable pain, resumption of ambulation and return to functional activity. A Total of 35 patients most of the patients we found were male 29 (82.86%) and female 6 (17.14%). Most of the patients found in 31-40 age group 14 (40.00%), then 41-50 and that was 11 (31.43%) respectively 5 (14.29%) found in 21-30, 11(31.43%) in 41-50 and 4 (11.43%) in >61. In another study there were age varied from 18 to 65 years, with a mean age of 41-50 years. There was male predominance. Male: Female ratio was -2:1. Based to the distribution of the study patients according to the complications in follow up sessions. Most of the patients Loose acetabular in after 3 months 11 (45.31%) then in Loose stem 19 (54.31%), Unstable 9 (25.71%), Infection 6 (17.14%), Pain 26 (74.29%) and Femoral fracture 13 (37.14%). After 6months Loose acetabular 7 (20.00%), Loose stem 2 (5.71%), Unstable 0 (0.00%), Infection 1 (2.86%), Pain 11 (31.43%), and Femoral fracture 3 (8.57%). The New Zealand joint registry has shown a revision rate of 0.89/100 component years (cy) for noncemented THRs in patients under 55 years 0.98/100 cy for those between 55-65 years (P < 0.001). In another study, the reason for revision was analysed the major cause for early revision in noncemented implants was either due to femoral fracture (30%) or dislocation (40%) whereas 75% of early revisions in the cemented group were secondary to dislocation [14]. Femoral fracture with noncemented stems has been identified as an early cause for failure by others [15,16]. The rate of femoral loosening within 90d was significantly higher in noncemented stems (P < 0.009) found in a study. Then the study from Modified Harris Hip Score. So most of them found 20 (57.14%), then 11 (31.4%) was good, 3 (8.6%) found fair and 1 (2.9%) found poor. Another study showed, final follow-up, 24 (96%) patients had excellent result and 1 (4%) had good result. None of our patients had Fair/Poor results. Preoperative mean modified Harris hip score was 57.50 compared to postoperative score of 97.25.
6. Limitations of the study
Our study wasn’t a blinded study so patient bias was present along with observer bias in subjective recording and the study and follow-up period was short in comparison to other studies, small sample size, limited resources and facilities; computer simulation facility was not available properly. So, to make more conclusive results, the following recommendations are proposed for further studies. Importantly in today's economic climate, economic analysis confirms that noncemented THA is a higher cost-effective option then cemented.
7. Conclusion and Recommendations
Noncemented Total Hip Replacement is a procedure with maximum excellent outcome found in our study. This procedure provides a nearly physiological joint and with experience, proper instrumentation, proper selection of implants, its placement in correct version and inclination, excellent results could be achieved with nil or minimal complication rate.
References
- Tarun V Desai, Niravkumar P Moradiya. Results of uncemented total hip replacement. International Journal of Orthopaedics Sciences 4 (2018): 308-312.
- Learmonth, Ian D, Cecil Rorabeck PCY. The operation of the century: total hip replacement. Lancet 370 (2007): 1580-1587.
- Prospective A. The influence of arthritis in other major joints and the spine on the one-year out come of total hip replacement 10 (2017): 1428-1437.
- Callaghan, John J, Albright, et al. Total hip arthroplasty with cement: Minimum twenty-five-year follow-up. J Bone J Surg 82 (2000): 487-497.
- Galia, Carlos Roberto, Diesel, et al. Total hip arthroplasty: a still evolving technique. Revista Brasileira de Ortopedia 52 (2017): 521-527.
- Bobyn JD, Pilliar RM, Cameron HU, et al. The optimum pore size for the fixation of porous-surfaced metal implants by the ingrowth of bone. Clin Orthop Relat Res 150 (1980): 263-270.
- Galante J. Total hip replacement. Orthop Clin North Am 2 (1971): 139-155.
- Tryba M, Linde I, Voshage G, et al. Histamine release and cardiovascular reactions to implantation of bone cement during total hip replacement. Anaesthesist 40 (1991): 25-32.
- Donaldson AJ, Thomson HE, Harper NJ, et al. Bone cement implantation syndrome. Br J Anaesth 102 (2009): 12-22.
- Borghi B, Casati A. Thromboembolic complications after total hip replacement. Int Orthop 26 (2002): 44-47.
- Ereth MH, Weber JG, Abel MD, et al. Cemented versus noncemented total hip arthroplasty: Embolism, hemodynamics, and intrapulmonary shunting. Mayo Clinic Proc 67 (1992): 1066-1074.
- Chandran P, Azzabi M, Andrews M, et al. Periprosthetic bone remodeling after 12 years differs in cemented and uncemented hip arthroplasties. Clin Orthop Relat Res 470 (2012): 1431-1435.
- Prathyush, Sivarama, BLVS Prasad, et al. A clinical study of uncemented total hip replacement in various hip disorders 8 (2019): 1-12.
- Wyatt M, Hooper G, Frampton C, et al. Survival outcomes of cemented compared to uncemented stems in primary total hip replacement. World J Orthop 5 (2014): 591-596.
- New Zealand Joint Registry report (2011).
- Swedish Hip Registry report (2011).


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 