Evaluating Disparities in Surgical Training across India and Opportunities for Global Collaboration
Maryam Borumand, Aanchal Madhok*,
Department of Surgery, All India Institute of Medical Sciences Delhi, India
*Corresponding Author: Aanchal Madhok, Department of Surgery, All India Institute of Medical Sciences, Delhi, India
Received: 14 October 2025; Accepted: 21 October 2025; Published: 30 October 2025
Article Information
Citation: Maryam Borumand, Aanchal Madhok. Evaluating Disparities in Surgical Training across India and Opportunities for Global Collaboration. Journal of Surgery and Research. 8 (2025): 512-517.
View / Download Pdf Share at FacebookAbstract
Background: India’s surgical training landscape faces significant disparities in quality, infrastructure, and access, particularly between metropolitan and rural settings. This cross-sectional study evaluated the perspectives of 29 surgical trainees across India to assess key challenges and opportunities within current training systems, with a focus on operative exposure, simulation access, research engagement, and interest in global collaboration. Methods: Participants included residents, super-specialty trainees and consultants, representing diverse geographical backgrounds. Findings revealed substantial inconsistencies in operative teaching and resource availability. Only 4 respondents felt their current hospital provided better training than previous placements, and simulation exposure was limited to basic models, with few having access to advanced tools. Research participation was skewed towards urban centres, with over a fifth of respondents unaware of academic surgical programmes.
Results: Thematic analysis identified five priority areas for international engagement: short-term fellowships, structured simulation training, workshops with visiting faculty, collaborative research, and systemlevel strengthening. Respondents strongly supported expanding day-case surgery under local anaesthesia and decentralising surgical services to improve rural access.
Conclusion: This study highlights an urgent need for equitable training reform, with actionable recommendations grounded in real-time trainee feedback. Integrating mentorship, simulation, and early academic exposure into surgical curricula especially in underserved areas could help bridge intra-national disparities. There has been interest in international collaboration, which offers a unique opportunity to match worldwide best practices with Indian surgical education while maintaining context-specific flexibility. These results offer national and international stakeholders a useful road map for improving surgical training and workforce resilience in India.
Keywords
<p>India Healthcare, Simulation-Based Education, Rural Surgery Access, Global Surgical Collaboration, Surgical Education</p>
Article Details
Introduction
Medical education in India starts with the MBBS degree, which requires students to complete a mandatory one-year rotating internship after completing clinical and academic coursework. After graduating, they can pursue super-specialty training (DM/MCh) for additional sub-specialization and postgraduate training (MD/MS) to become specialist trainees. After finishing, individuals might work as consultants in their sector of choice [1].
India will need approximately 291824 additional surgeons, obstetricians, and anaesthetists by 2030 to meet projected demands. Within India’s health system, there are striking disparities in specialist availability: rural community health centres face an 83% shortfall of surgeons, with only 913 surgeons in place out of 5 491 required [2].
Educational experiences remain highly inconsistent across institutions, particularly in low and middle-income countries (LMIC). A 2024 global survey of surgical trainees revealed significant disparities in operative exposure, availability of simulation-based learning, and access to academic mentorship highlighting the urgent need for systemic reforms and international support [3]. In India, although postgraduate surgical programs such as MS, DNB, and MCh are governed by the National Medical Commission (NMC) and the National Board of Examinations (NBE), considerable variability in training standards persists between institutions [4].
Simulation-based education and academic involvement are cornerstones of modern surgical training. In high-income countries (HICs), these modalities supplement clinical exposure and improve technical skills and critical thinking [5]. NIHR Global Health Research Unit on Global Surgery has implemented large multi-country trials such as the FALCON and ChEETAh studies which demonstrated that standardising surgical protocols across LMIC hospitals can lead to comparable outcomes between resource-limited and better-resourced centres [6].
Evidence from other low-income settings highlights the potential of international collaboration: a study published in the Journal of Public Health in Africa found that doubling health aid could save 44 infants per 1 000 live births, showing a significant long-term improvement in health outcomes [7]. This underscores the value of sustained overseas support in strengthening health systems and medical education.
One area where international effort could play a role is surgical training. Improving quality of surgical training can have a pivotal role in providing access to safe and effective surgical care across rural and remote regions [8,9]. As global surgery gains pace, international collaboration is increasingly considered to boost surgical capability in LMIC [10-13]. Understanding trainee perspectives on such collaborations is vital for determining areas of focus and for designing effective and sustainable global surgical partnerships.
This study aims to evaluate the current state of surgical training in India from the trainee perspective, focusing on four key areas: operative experience and teaching, regional disparities, access to simulation and research, and opportunities for global collaboration.
Methods
Study design
A cross-sectional study was conducted using an online survey created on google forms. The survey link was distributed across India through hospital-based WhatsApp groups that were specifically organised by surgical speciality. This ensured that only the surgeons from these groups (multi-speciality trainee – Surgical consultant) were able to participate, preventing responses from individuals outside the intended cohort. Surveys were administered over two equivalent two-month periods, first in 2023 and repeated 2 years later in 2025.
The 14-question survey included multiple-choice, Likert-scale, and open-ended questions. Domains covered were: Training level and locations, perceived adequacy of operative exposure and teaching, access to simulation and research, awareness of academic surgical programs, opinions on the geographical distribution of surgical services, views on how surgeons from HICs could support training and improve access.
Data analysis
Quantitative responses were analysed using descriptive statistics in Excel. Categorical responses were summarised by frequency and percentage. Open-ended responses were analysed using thematic analysis to discover reoccurring themes around global relationships and training quality.
Ethical approval
As the survey collected no personal or identifiable information, formal consent was not required. Completion of the questionnaire was taken as implied agreement to participate, and respondents were assured that their answers would remain anonymous and be used solely for research purposes.
Results
29 individuals completed the survey. Participant roles included: Super-specialty surgical trainees (e.g., MCh/DNB), 10, MS General Surgery residents, 14, Consultants, 3 and undisclosed, 2.
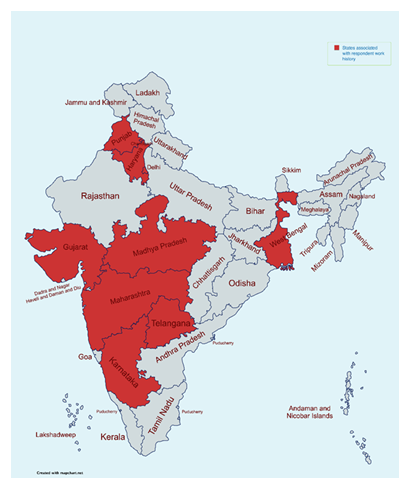
Respondents were trained across a wide range of regions in India, including major metropolitan centres such as Delhi, Mumbai, Kolkata, as well as smaller urban and rural areas such as Bihar and Faridkot. [Figure 1]. One participant had also undertaken training internationally in Dubai When asked if there is adequate surgical hospital coverage across India: 13 answered “Yes” and 5 selected “Maybe’’.
Rural areas, Bihar, and the North/Northeast were cited as under-resourced. One respondent commented, “In the interiors of every state, surgical accessibility is very low – overseas support could play a critical role there.”
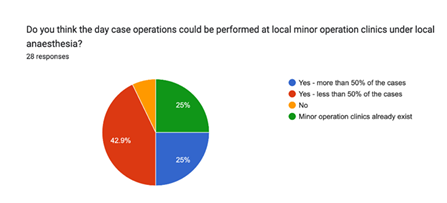
23 reported that less than half of surgeries were day-case procedures. Most respondents (27) believed that more surgeries could be done in minor procedure clinics under local anaesthesia, particularly for day- case operations [Figure 2].
Surgical Training
When comparing current hospitals to previous institutions 13 reported that previous hospitals had better facilities and teaching. Only 4 felt their current centre offered superior teaching. 13 had used simulation during training. Common simulations included: Laparoscopy box trainers, Airway management mannequins, Catheterisation and CPR models. Only a few respondents used specialty-specific models (e.g., vascular anastomosis or robotic trainers)
Research
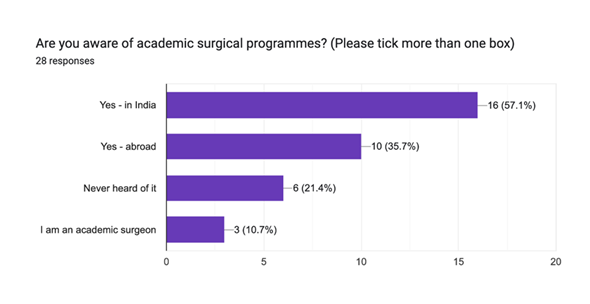
18 had participated in research. 6 were interested but felt there were no opportunities. 5 had no exposure to research. Similarly, 6 had never heard of academic surgical programs (Figure 3). Those with research experience had typically trained in metropolitan institutions, whereas lack of exposure was more common trainees in smaller centres such as Bihar.
International collaboration
Trainees expressed strong interest in international involvement. Thematic analysis revealed five key areas:
Fellowship Opportunities:
Majority were keen on short-term fellowships or observerships abroad. One wrote, “Fellowships would help us learn newer techniques and broaden our perspective.”
Simulation and Structured Courses:
Many suggested setting up simulation centres and having structured training programs, ideally with some international input.
Workshops and Visiting Faculty:
Trainees expressed strong interest in operative workshops led by foreign faculty, particularly in rural or underserved regions. Large tertiary hospitals such as AIIMS Delhi already host international surgeons for specialised training programs and surgical workshops, providing valuable exposure to advanced techniques.
Research Collaboration:
Trainees also wanted greater chance to learn about research, be able to attend international conferences, and take part in bigger, multi-centre projects.
System Strengthening:
Some also suggested support with improving hospital systems, like better logistics, setting up outpatient minor surgery models, and running things more efficiently overall.
One respondent noted that Indian training already matches global standards in some centres, emphasising the bidirectional nature of collaboration.
Discussion
This study is uniquely strengthened by its first-hand insights from a broad spectrum of surgical trainees, spanning surgical trainees to consultants and representing both urban and smaller city settings across India. It is worth noting that unlike many existing surveys, it captures real-time trainee ideas, concerns, and expectations, offering a valuable lens for reform grounded in lived experience rather than assumption. The thematic analysis identifies specific areas where global and national institutions can act.
The findings suggest that surgical education in India suffers from both systemic inequity and institutional inconsistency. Whilst high-performing centres such as AIIMs Delhi offer exposure to simulation, many rural and other programs lack basic infrastructure or mentorship pathways as highlighted by trainees’ responses. Smaller hospitals and institutions, especially those in non-metropolitan areas, should be encouraged to adopt similar initiatives to ensure equitable access to high-quality surgical education across the country.
Our results are consistent with international literature pointing to the underuse of simulation and variation in training quality across LMICs [14-16]. However, this study offers more detailed evidence on intra-country disparities, highlighting that within India, access to modern surgical education tools is uneven. While literature from HICs often assumes simulation is a universal adjunct, this expectation does not hold in many Indian surgical programs.
This study highlights several key disparities and opportunities within India’s current surgical training ecosystem. While a majority have had the opportunity to participate in research, a significant portion remain underserved, either due to lack of access or awareness, signalling a gap in institutional academic outreach. The fact that over one-fifth of respondents were unaware of existing academic surgical programs underscores the need for improved dissemination of research opportunities and mentorship pathways.
Notably, only 4 participants believed their current hospital offered better teaching than previous placements, highlighting variability in institutional quality. The expressed need for workshops, fellowships, and academic access reflects similar sentiments captured in COST-Africa and SURG-Africa mentorship initiatives, but no such model is yet established in India [16]. Strengthening institutional support and integrating research training into surgical curricula could foster a more uniformly academic culture and better prepare trainees for evidence-based practice.
Even though 13 felt that surgical hospital coverage in India was ‘adequate’, rural areas such as Bihar was repeatedly cited as underserved. A striking 27 of respondents felt that more day case surgeries could be done under local anaesthesia, implying support for expanding minor procedures beyond central hospitals to peripheral centres.
Trainees also expressed a strong interest in international engagement across five domains: fellowships, simulation and structured training programs, operative workshops led by visiting faculty, collaborative research opportunities, and system-level reforms, such as improving hospital logistics and outpatient surgery models. Many specifically identified laparoscopy, robotic surgery, and simulation labs as desired areas for investment which shows an increasing awareness of technological gaps and a willingness to adopt advanced techniques.
Some studies provide global overviews of surgical education disparities [3,5] but they generalise across LMICs and focus more on institutional metrics than lived experiences. Similarly, the MoHFW 2023 report outlines infrastructure and workforce shortfalls [1] but does not assess educational quality or simulation access. Global initiatives such as NIHR Global Surgery’s FALCON and CHEETAh trials have demonstrated the clinical impact of standardised surgical protocols in LMICs [6] but have not examined trainee expectations from such partnerships. This study fills that gap by providing direct, multi-level insights from Indian surgical trainees across 21 cities offering nuanced insights on how operative exposure, teaching quality, and academic access vary by region.
This paper identifies five actionable areas where Indian trainees seek global collaboration, providing a roadmap for more responsive and locally relevant global surgery initiatives. The finding that a more than a 3rd of respondents were MS trainees who were actively interested in training reform and research, highlights the necessity of starting academic engagement at the undergraduate level. This is a group that is frequently disregarded in the literature on surgical education reform.
The desire among trainees for global collaboration is evident and aligned with broader global health education trends. The overwhelming support for expanding minor procedure clinics and simulation-based training suggests a readiness for scalable, decentralised surgical solutions.
This study presents a proposed, evidence-based action plan to guide next actions in correcting the inequities discovered in India's surgical training landscape, based on trainee-reported priorities and gaps identified in this study. This framework provides practical and adaptable strategies that can serve as a foundational roadmap for institutional leaders, policymakers, and global partners seeking ways to enhance equity and effectiveness in surgical education in India.
Mentorship and fellowship
Respondents expressed concern about the lack of continuous mentorship in outlying and rural training centres. We encourage developing financed rural mentorship and fellowships based on successful models such as the SURG-Africa mentorship initiative [17]. These programs would send experienced surgical educators to underfunded hospitals to provide hands-on training, enable case-based learning, and support regular audit and quality improvement cycles.
Global faculty teaching days
Respondents expressed strong interest in learning about international surgical procedures. Institutions such as AIIMS Delhi have already pioneered programs in which visiting surgeons from other countries lead specialised training and actual surgical sessions. A national rollout of these "Global Faculty Days" could democratise access to such opportunities and hasten the adoption of contemporary surgical techniques. Rwanda's Human Resources for Health Program [18,19] demonstrates how coordinated international faculty involvement can improve national surgical training systems.
Undergraduate research pathways
Although many trainees expressed an interest in academic surgery, early exposure to research possibilities was restricted. To address this, medical institutions should begin integrating students into research environments at the undergraduate level, using structured initiatives such as elective audit projects, local and national student research, and formal research methodology workshops [19]. In HICs such as the United Kingdom and the United States, medical students are increasingly publishing in peer-reviewed journals during their undergraduate years, frequently through integrated research components or institutional mentorship programs. It is reported that such early exposure promotes long-term academic engagement and career growth [20]. Adoption of similar frameworks in LMICs, including India, could assist to close the academic participation gap and foster a more research-oriented culture among future surgeons.
This framework is not exhaustive, but it does provide a strategic and scalable foundation for enhancing surgical education in India. Each proposed intervention is based on both local trainee experiences and known worldwide best practices in LMIC environments. These proposals aim to minimise intra-national discrepancies, increase mentorship and academic integration, and foster a more consistent, fair environment for surgical trainees across the country.
Limitations
The study’s sample size of 29 participants over a two-month period was insufficient to fully capture the diversity of surgical training experiences across India. More participants are needed to improve generalisability. Furthermore, highly remote and neglected areas, like Nagaland, where representation was lacking, were not well-represented in the poll. In order to promote wider distribution and guarantee more thorough coverage, future research could enhance inclusivity by involving regional representatives from various regions of India.
Conclusion
Surgical training in India evidently presents an imbalance in which centres of expertise co-exist alongside under-resourced programs. Trainees advocate for increased standardisation, extended simulation, better rural access, and globally endorsed academic pathways. Investing in education, decentralisation, and global partnerships is essential to building a resilient surgical workforce that meets the health needs of India’s diverse population.
Acknowledgment
The authors would like to express their gratitude to everyone who took the time to fill out this survey. Their collaboration and insightful contributions have been crucial to the success of this study. Without their assistance, this effort would not have been feasible. No funding was required or received for the completion of this study.
References
- Tandon A. Postgraduate surgical training in India. Indian J Med Ethics 7 (2010): 264-265.
- Health Dynamics of India 2022-2023.
- Poudel S, Kurashima Y, Kapsampelis P, et al. What do surgical trainees and educators around the world need: a global needs assessment survey from 6 regions around the world. Global Surg Educ 4 (2024).
- Hooda A, Dhillon MS, Neradi D, et al. Orthopedic residency in a tertiary care hospital of India: Positives, negatives and perspectives for change. Indian J Orthop 55 (2021): 209-216.
- Shahrezaei A, Sohani M, Taherkhani S, et al. The impact of surgical simulation and training technologies on general surgery education. BMC Med Educ 24 (2024): 1297.
- Picciochi M, Alexander PV, Anyomih T, et al. Provision of inguinal hernia surgery in first-referral hospitals across low- and middle-income countries: Secondary analysis of an international cohort study. World J Surg 49 (2025): 374-384.
- Negeri KG. The long-run effects of health aid in low-income countries. J Public Health Africa 14 (2023): 2219.
- Zadey S. Measuring Access to Surgical Care in Rural India: Synthesis of Data and Novel Index (2021).
- Shaban L, Mkandawire P, O’Flynn E, et al. Quality metrics and indicators for surgical training: A scoping review. J Surg Educ 80 (2023): 1302-1310.
- Meara JG, Leather AJM, Hagander L, et al. Global Surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. Lancet 386 (2015): 569-624.
- Krakauer KN, Wong LY, Tobias J, et al. Evaluating global surgery partnerships from low and middle income country perspectives. J Surg Res 296 (2024): 681-688.
- Nwagbata A, Dutta R, Jayaram A, et al. Beyond the Ivory Tower: Perception of academic global surgery by surgeons in low- and middle-income countries. Plos Glob Public Health 4 (2024): e0002979.
- Raval H. Training at skills lab, need of the time? Neurol India 71 (2023): 567.
- Broekhuizen H, Ifeanyichi M, Mwapasa G, et al. Improving access to surgery through surgical team mentoring - policy lessons from group model building with local stakeholders in Malawi. Int J Health Policy Manag 11 (2022): 1744-1755.
- Wilkinson E, Aruparayil N, Gnanaraj J, et al. Barriers and facilitators of laparoscopic surgical training in rural north-east India: A qualitative study. International Journal of Surgery: Global 3 (2020): e29.
- Abahuje E, Tuyishime E, Alayande BT. Global surgical simulation education, current practices, and future directions. Surgery 180 (2025): 109050.
- Velin L, Lantz A, Ameh EA, et al. Systematic review of low-income and middle-income country perceptions of visiting surgical teams from high-income countries. BMJ Glob Health 7 (2022): e008791.
- Binagwaho A, Kyamanywa P, Farmer PE, et al. The human resources for health program in Rwanda- new partnership. N Engl J Med 369 (2013): 2054-2059.
- Chang Y, Ramnanan CJ. A review of literature on medical students and scholarly research: experiences, attitudes, and outcomes: Experiences, attitudes, and outcomes. Acad Med 90 (2015): 1162-1173.
- Griffin MF, Hindocha S. Publication practices of medical students at British medical schools: experience, attitudes and barriers to publish. Med Teach 33 (2011): e1-e8.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 