Evaluation of Phospholipase A2 Activity, High Sensitive C- Reactive Protein Level and White Blood Cell Count as Predictive Markers in Acute Appendicitis: Novel Approach
Suma S*, Sreeramulu PN, Dayanand CD
Department of General Surgery, Sri Devraj Urs Medical College, Kolar, Karnataka, India
*Corresponding author: Suma S, Department of General Surgery, Sri Devraj Urs Medical College, Kolar, Karnataka, India
Received: 02 September 2021; Accepted: 09 September 2021; Published: 28 September 2021
Article Information
Citation: Suma S, Sreeramulu PN, Dayanand CD. Evaluation of Phospholipase A2 Activity, High Sensitive C- Reactive Protein Level and White Blood Cell Count as Predictive Markers in Acute Appendicitis: Novel Approach. Journal of Surgery and Research 4 (2021): 491-503.
View / Download Pdf Share at FacebookAbstract
We compared the predictive value of determining group II phospholipase A2 (PLA2) in serum for diagnosing acute appendicitis with the predictive values of white blood cell count (WBC) and measurement of C-reactive protein (CRP). In this prospective study, we included 62 patients who were undergoing appendectomy after clinical diagnoses of acute appendicitis. The performance of each test was measured by receiver-operating characteristic curves. The white blood cell count usually becomes elevated with infection. In early appendicitis, before infection sets in, it can be normal, but most often there is at least a mild elevation even early in the process. Unfortunately, appendicitis is not the only condition that causes elevated white blood cell counts.
Background
Appendicitis and acute abdominal pain are interrelated; pose to emergency surgical intervention for remedy. Despite of advanced techniques, the chance of appendicular perforation worsening the condition is high. An ideal approach to understand such an emergency scenario is more vital in patient care at health delivery system.
Materials and Methods
This Prospective study was conducted in 62 patients who have been clinically diagnosed as having acute appendicitis and posted for emergency appendectomy, from December 2016 to 2018. Pre-operatively blood was collected for high sensitive C- reactive protein (hs CRP) and PhospholipaseA2 (PLA2) estimation, after completion of surgical procedure, all specimens were sent for histopathological examination, which were correlated with the results of hs CRP levels and PLA2 activity.
Results
In present study, males (54.8%) outnumbered females (45.2%). In the study mean age of subjects was 26.77 ± 11.371 years. Majority of them were in the age group <20 years (38.7%), 25.8% were in the age group 21 to 30 years, 22.6% were in the age group 31 to 40 years an
Keywords
<p>Appendicitis, High sensitive C- reactive protein, Acute-phase reaction, Leukocytosis, Enzymes, Immunoassays</p>
Article Details
1. Introduction
Appendix is a tubular structure found at the base of the caecum in the human body and regarded as vestigial in nature and initially described by Reginald Heber Fitz in 1886 [1]. Whenever, this organ gets infected by unknown etiologies results inflammation and intense pain in the right iliac fossa, termed as “appendicitis”. The lifetime occurrence of this disease is approximately 7%, with perforation rate of up to 20% [2]. Despite of advanced techniques, it is still often difficult to differentiate between simple and complicated appendicitis, which is usually defined as appendicitis with gangrenous change, abscess, or perforation [3,4]. Hence, this condition has become the serious health problem, attracts immediate medical intervention, if delayed, edematous appendix can progress to gangrene, rupture with generalized peritonitis and serve as fatal. Factors that you construct your forecast with respect to. In general surgical practice, acute appendicitis is frequently encountered as a cause for acute abdomen [5]. The domain of appendix has been a paramount importance for research activity ever since the time it was known. Significant amount of research has been carried out linked to its etiological factors, laboratory parameters and management options. The research is advanced in the field of investigations including laboratory and radiological studies over the years. Furthermore, studies and trials are being conducted to aid in prompt identification of complicated appendicitis and to find the most appropriate and sensitive diagnostic tool. Even though, with the advent of numerous studies, it is observed that the clinical diagnosis of appendicitis is often at a dilemma and needs an adjuvant parameter which aids in confirmation of diagnosis. On the other hand, complicated appendicitis such as gangrenous (necrotic) appendicitis should be treated with emergency surgery [6]. There have been a number of laboratory tests widely available in determining the severity of acute appendicitis. Conventional clinical or laboratory parameters, including the body temperature (BT), white blood cell count (WBC), neutrophil/ lymphocyte ratio (N/L ratio), and C-reactive protein (CRP) level, have been in use to distinguish between uncomplicated and complicated appendicitis [7,8]. In 1994, Juha M. Grnroos et al. reported the role of WBC, C- reactive protein and PLA2 as indicators of perforation and formation of appendiceal abscess. The current study aims to evaluate relationship between hsCRP, PLA2, clinical and histo-pathological examination of specimens
2. Materials and Methods
2.1 Materials
2.1.1 Study design: The Prospective studywas conducted with 62 patients’ enrolment on obtaining patient information consent. The subjects were clinically diagnosed for acute appendicitis and posted for emergency appendectomy in Department of General Surgery, RL Jalappa Hospital and Research Center of Sri Devraj Urs Medical College, Kolar during the period from December 2016 to November 2018. An institutional human ethical clearance obtained to conduct this study. The study has Inclusion criteria as patients clinically diagnosed to have appendicitis. However, patients with Urinary tract infection, diverticulitis, mesenteric lymphadenitis, crohn’s disease, Pelvic Inflammatory Disease and Other inflammatory conditions were excluded. The patients presenting with right iliac fossa pain and tenderness subjected to clinical examination with relevant investigations after obtaining a patient information consent and recruited in the study for collection of the demographic, clinical and biochemical data. Then after, cases were subjected to surgical interventional procedure for appendectomy.
2.1.2 Sample collection: Three ml of blood was collected during preoperative condition into plain vacationer and allowed for retraction to separate the serum, centrifuged at 300rpm at room temperature for 20 minutes to get a clear serum and was stored at -200 C until analysis. After surgical intervention, all appendix specimens collected were sent for histo-pathological examination.
3. Related Work
- George Bax, and Simon Paterson-Brown et al [1] author describes that the white cell count and C-reactive protein measurements are useful in the assessment of acute appendicitis: if used judiciously, they may spare a group ofvpatients not only an unnecessary surgical procedure, but also unnecessary admission to hospital for observation.
- Mario Di Napoli and Hedley CA, Ensley et al [2] author explained there is not sufficient evidence to recommend measurement of CRP in the routine evaluation of cerebrovascular disease risk in primary prevention, because there is insufficient evidence as to whether early detection, or intervention based on detection, improves health outcomes, although shared risk of cardiovascular disease indicates this may be of value. In secondary prevention of stroke, elevated CRP adds to existing prognostic markers, but it remains to be established whether specific therapeutic options can be derived from this.
- Han-Ping Wu MD and Ching-Yuang L et al [3] author described that the different cutoff values of CRP concentration may serve as a predictive parameter in early diagnosis of acute appendicitis on the first 3 days after onset of symptoms. The predictive value of CRP is especially effective in the patients with perforated appendicitis. We therefore propose the addition of CRP measurement as a routine laboratory test in patients suspected of having acute appendicitis.
- Grönroos, J Forsström, K Irjala, TJ Nevalainen et al the performance of each test was measured by receiver-operating characteristic curves. WBC was the test of choice in diagnosing uncomplicated acute appendicitis [5]. However, in contrast to CRP and PLA2, which increased in patients with protracted inflammation, there was not a concomitant increase in WBC. Therefore, especially CRP, but also PLA2, were better indicators of appendiceal perforation or abscess formation than was WBC. Increased WBC, CRP, and PLA2 values did not unequivocally corroborate the clinical suspicion of appendicitis, but if all three values were within normal limits, acute appendicitis could be excluded with a 100% predictive value.
- Juha M Grönroos et al. author explained both clinical findings and laboratory tests are unable to reliably distinguish between patients with acute appendicitis and those without [6]. If both WBC count and CRP are normal, acute appendicitis is very unlikely. The current results emphasize the role of CT imaging in patients with suspected acute appendicitis.
4. Research Methodology
4.1 Methods
Three values were within normal limits, acute appendicitis could be excluded with a 100% predictive value. PLA2 values showed a highly significant correlation with CRP but not with WBC values, which supports the view that PLA2 represents an acute-phase reactant.
4.2 Determination of serum PhospholipaseA2 level 4.2.1 Principle: The procedure of PLA2 activity is based on sandwich enzyme-linked immune-sorbent assay technology and measurement was done as per the procedure leaflet supplied by the Cayman Company, USA. Anti PLA2G1B antibody was pre-coated onto well plates. And the biotin conjugated Anti PLA2G1B antibody was used as detection antibodies in the standard and test samples. Subsequently, it is washed with the wash buffer. HPR-streptavidin added and unbound conjugates washed. TMB substrates were used to visualize HPR enzymatic reaction. TMB was catalyzed, a blue color that changes into yellow color after addition of the acidic solution. The absorbance recorded at 450nm using micro plate reader and the concentration of PLA2 can be calculated and represented as ng/ml.
4.3 Determination of serum high sensitive C- reactive protein level
Serum hs CRP level is quantified by solid phase direct sandwich method as per the procedure sheet supplied by Cal biotech, USA. Anti CRP antibody was pre-coated onto well plates. Sample and standard was added for detection of CRP, subsequently anti CRP-HRP conjugate was added to the wells coated with CRP antibody and washed with wash buffer to remove the excess unbound conjugates. Upon the addition of the substrate, the intensity of the color produced measured by micro plate reader at 450nm and the concentration of CRP calculated referring to graph and represented as mg/L. To do this as effectively as possible, some form of intraoperative imaging is typically used to verify surgical accuracy. The intraoperative images help make sure.

Figure 1: Acute appendicitis
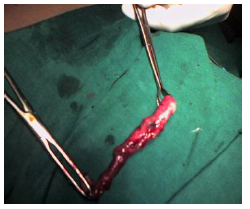
Figure 2: Perforated appendix

Figure 3: Gangrenous appendix
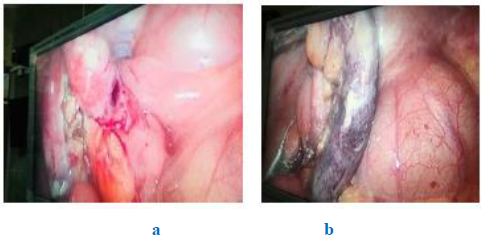
Figure 4a, 4b: Appendicular perforation and gangrenous appendix (Laparoscopy)
5. Simulation and Result Discussion
5.1 Clinical results
The demographic variables of the study patients of acute appendicitis fall in less than 20 years of age and amounts to 38.7 percent whereas 23 percent cases were between 20-40 years as shown in table 1. However, the data indicated minimal percent (13 %) cases belong to age group above 40 years. Predominantly, it has be revealed that male subjects in the study group evinced more tendency with acute appendicitis (54%) in comparison with the female patients (46%) were in the mean age of 26.7 years. This study also describes the distribution of acute appendicitis without complication contributes (56.5%), cases with Appendicular Perforation (6.5%) and Recurrent Appendicitis (37.1%), from the study population. Table 2 illustrates mean and standard deviation of biochemical parameters measured from the acute appendicitis cases enrolled in the study (n=62). The mean results of high sensitive C- reactive protein (hs CRP), a well-known establishes inflammatory marker indicated mean concentration in mg/ml (mean 3.16, SD± 2.60). This serves as ideal reference inflammatory marker in the study to which a new parameter phospholipase A2 enzyme was compared and found to be statistically significant (mean 12.6ng/ml, SD± 1.25).
|
S.No |
Sampling |
P value |
P<0.001 |
Test results |
|
1 |
Hs CRP |
0.168 |
Significant value |
+positive |
|
2 |
PLA2 |
0.479 |
Significant value |
+positive |
|
3 |
TLC |
0.015 |
Significant |
+positive |
Table 1: Demographic profile for sampling method for study population respondents
|
Sl.No. |
Particulars |
TLC |
Hs CRP |
PLA2 |
|
1 |
Sample size |
62 |
62 |
62 |
|
2 |
Mean |
11.64 |
3.1516 |
12.5723 |
|
3 |
Std. Deviation |
4.49 |
2.60124 |
1.24772 |
Table 2: Mean distribution of hs CRP and PLA2 in the study population.
According to the number of cases identified for various types of appendicitis based on histopathological examination. As per the results the cases characterized with inflammatory appendix has 50 cases amounts to 80.6 percent from the subjects. 5 cases reported as acute necrotizing appendicitis with 8.1 percent distribution. However, Acute gangrenous appendicitis and Acute Appendicitis and Peri Appendicitis reported with 2 cases of 3 percent distribution. The remaining, Acute Necrotizing Appendicitis and PeriAppendicitis, Appendicular Perforation and PeriAppendicitis and Lymphoid Hyperplasia reported with one each cases amount to 1.6 percent, table 3 signifies the positive correlation between hs CRP and PLA2. i.e. with increase in hs CRP, there was increase in PLA2 and Vice versa. However the correlation was not statistically significant.
|
Correlations(r) |
|||
|
Hs CRP |
PLA2 |
||
|
Hs CRP |
Pearson Correlation |
1 |
0.12 |
|
Sig. (2-tailed) |
0.352 |
||
|
N |
62 |
62 |
|
Table 3: Correlation between hs CRP and PLA2
|
Clinical Diagnosis |
P value |
||||||
|
Acute Appendicitis |
AP |
RA |
|||||
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
||
|
Hs CRP |
3.32 |
2.34 |
5.88 |
2.59 |
3.42 |
2.82 |
0.168 |
|
PLA2 |
12.46 |
1.22 |
12.81 |
1.72 |
12.21 |
1.22 |
0.479 |
|
TLC |
11.5 |
4.36 |
17.7 |
1.54 |
10.8 |
4.36 |
0.015* |
Table 4: hs CRP and PLA2 levels comparison with respect to clinical diagnosis
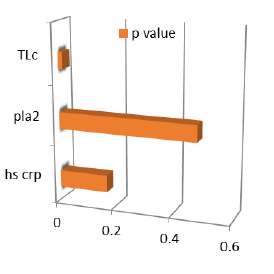
Figure 5: Plotted graph represent Pvalue for clinical diagnosis
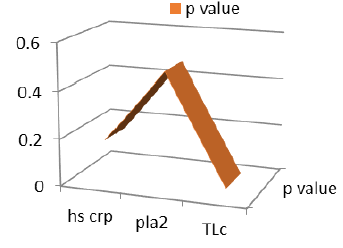
Figure 6: Curve plotted represent P values lies between 0.015 to 0.479.
Figure 7: Graph represent number of patients records
|
Number of patients |
|
|
male |
35 |
|
female |
27 |
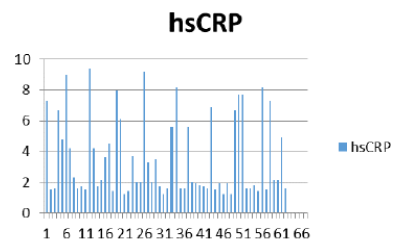
Figure 8: Hs CRP represent varies level.
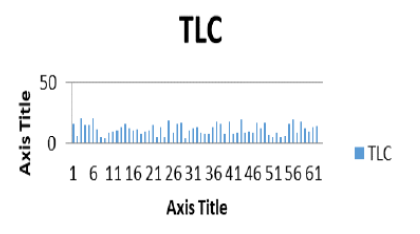
Figure 9: TLC based plotted graph represent level of values.
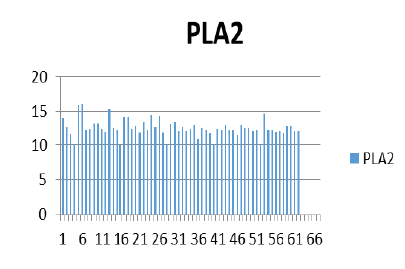
Figure 10: PLA2 based plotted graph represent level of different values
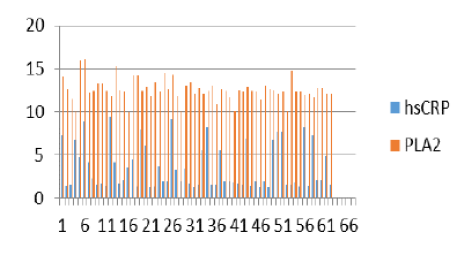
Figure 11: HS crp and PLA2 comparision analysis representation
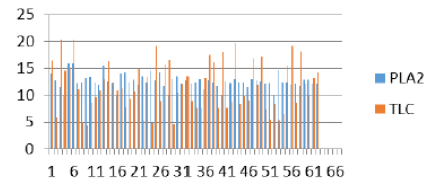
Figure 12: PLA2 and TLC comaprision analysis representation
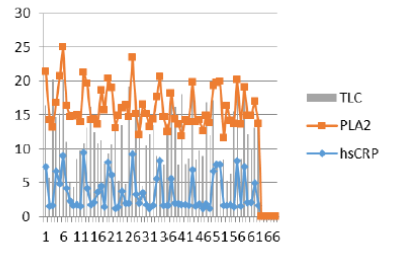
Figure 13: Compare various clinical diagnosis values simultaneously.
6. Discussion
Acute appendicitis is more frequent cause for emergency abdominal surgeries. As per the report, it appears during second and third decade of life [9]. Similarly, it is found in the current study population in the age group of 24 years amounts to 38.7% whereas 21-30 years amounts to 25.8%. Generally, acute appendicitis rarely observed in children, Nevertheless, Our study had one enrollment at the age of five years, rest of the participants enrolled were adults. It is clearly evident in the study that at the early age or at elderly age, the chance of acute appendicitis gradually reduces [9]. In support of this, study revealed that about 12.9% cases belonged to age groups of more than 40 years. The chances of need of surgery for appendectomy are same among male and female before puberty. However, after puberty the percentage of appendectomy varies from 12% for men and 25% for women. However, during the life span the overall 7% of all people undergoing appendectomy [10-12]. The overall study population consists of 54.8% male and 45.2% female represented with acute appendicitis. This data facilitates to gather the possible causes for acute appendicitis, which is generally high in females than males. The classic triad of a history compatible with appendicitis, pain at Mc Burney’s point, and leukocytosis has a diagnostic accuracy rate <80% and, even when the triad is combined with new radiologic techniques, the accuracy is no better than 90% [12-14]. As a result, a new method to aid in the diagnosis of acute appendicitis would be well encouraged in clinical scenario which usually hints the diagnosis of appendicitis. Even though, a diagnosis can only be confirmed with subsequent pathological evaluation for surgery. Several blood markers, including bilirubin, C-reactive protein (CRP), and white blood cell (WBC) count may be relevant and increased in patients with appendicitis [15,16]. Numerous scoring systems evaluating clinical symptoms and blood tests to increase the prognostic accuracy of appendicitis have been designed [17]. However, despite of several scoring system are in use to understand the signs of appendicitis, none of the scoring systems as single or in combination with blood markers helps to evaluate the risk of appendicular perforation. In the search for a reliable indicator, current study focused on measurement of hs CRP and PLA2 also as blood markers to the existing parameters in use to evaluate the acute appendicitis. Blood markers in combination are useful in predicting appendicitis and perforated appendicitis namely C- reactive protein, white cell count, serum bilirubin, alpha-1 acid glycoprotein and erythrocyte sedimentation rate are may be appropriately used in diagnosis. Therefore, blood levels of these diagnostic markers should be taken into consideration when predicting appendicitis [18,19]. In our study population, hs CRP along with an enzyme marker PLA2 were measured and found that the mean hs CRP value was high among patients with appendicular perforation amounting to 4.43mg/L. We also measured PLA2 level to evaluate the possibility of acute appendicitis and considering PLA2 as a new biochemical marker to help in the diagnosis of acute appendicitis along with hs CRP. And also the possibility of detecting early and impending complications associated with acute appendicitis like the necrotizing or gangrenous appendix. There are limited information about the use of PLA2 in association with diagnosis of appendicitis [20]. Therefore we evaluated serum PLA2 and its possible relation with hs CRP in acute appendicitis to evaluate its efficacy as a diagnostic marker for acute appendicitis. Besides this, the correlation between elevated PLA2 and hs CRP levels have a high predictive potential in the early diagnosis of Appendicular perforation with hs CR Pmg/L(4.43±3.34) and PLA2 ng/ml(12.21±1.72) than other conditions like recurrent appendicitis with 3.31±2.80mg/L and 12.81±1.22ng/ml respectively. From the total population (n=62) about 56.5% were diagnosed to have Acute Appendicitis with hs CRP (3.02±2.42) and PLA2 (12.21±1.22), 6.5% had Appendicular Perforation and 37.1% had Recurrent Appendicitis. Study also demonstrated that evaluation of hs CRP, even though it is a well-known inflammatory marker, in cases like acute appendicitis, appendicular perforation and recurrent appendicitis is not statistically significant. However measures of PLA2 in all the cases were found to be statistically significant with p value of <0.05. In the study, in the aspect of histopathological examination and clinical diagnosis, there was a prominent increase of hs CRP(mg/L) noticed in complicated appendicitis like acute necrotizing appendicitis with per appendicitis(7.30mg/L), inflamed appendix(3.28±2.66mg/L), acute necrotizing appendicitis(3.65±5.16), acute appendicitis with per appendicitis(2.90±1.84). However, in the remaining conditions the hs CRP value ranges from 1.2-1.9mg/L. The PLA2 level in all the conditions of acute appendicitis displayed 11-14ng/ml constantly. Therefore for the diagnosis of appendicitis, the measure of phospholipase A2 along with other established marker in consideration a single perhaps useful to understand the appendicitis along with the clinical examinations.
7. Conclusion
PLA2 activity appears to be a promising new laboratory parameter for diagnosing acute appendicitis along with clinical examination. It also promises to have a predictive potential for the diagnosis of acute appendicitis. Patients with clinical signs and symptoms of appendicitis and high hs CRP and PLA2 activity should be identified as having a higher probability of acute appendicitis, more significant in appendicular perforation suggesting that these markers have a high predictive potential for the diagnosis of acute appendicitis.
Acknowledgement:
We would like to thank the authorities of Sri Devraj Urs Academy of higher education and research Kolar, Karnataka, India for supporting this post study. We would also like to acknowledge department of Pathology for the support given for the study.
Limitations:
Study needs more enrollments and screening of study parameters in the control population as basal information.
Conflict of interest:
There is no conflict of interest between the authors.
References
- Wu X, Kumar V, Ross Quinlan J, et al. Top 10 algorithms in data mining. Knowledge and Information Systems 14 (2007): 1-37.
- Damien R. The early days in the history of appendectomy. Hektoen International Journal (2013).
- Storm-Dickerson (TL), Horattas (MC). What have we learned over the past 20 years about appendicitis in the elderly? Am J Surg 185 (2003): 198-201.
- Martin AE, Vollman D, Adler B, Caniano DA J. CT scans may not reduce the negative appendectomy rate in children. Pediatr Surg 39 (2004): 886-890.
- Markar SR, Karthikesalingam A, Cunningham J, et al. Increased use of pre-operative imaging and laparoscopy has no impact on clinical outcomes in patients undergoing appendicectomy. Ann R Coll Surg Engl 93 (2011): 620-623.
- Addiss DG, Shaffer N. The epidemiology of appendicitis and Appendectomy in the United States. Am J Epidemiol 132 (1996): 910-925.
- Mason RJ. Surgery for appendicitis: is it necessary? Surg Infect 9 (2008): 481-488.
- Grönroos JM, Grönroos P. Leucocyte count and C-reactive protein in the diagnosis of acute appendicitis. Br J Surg 86 (1996): 501-504.
- Sand M, Bechara FG, Holland- Letz T, et al. Diagnostic value of hyperbilirubinemia as a predictive factor for appendiceal perforation in acute appendicitis. B Am J Surg 198 (2009): 193-198.
- Lally KP, Cox SC, Andrassy RJ. The Appendix, In: Sabiston Textbook of Surgery 2005, (18th edtn), vol 2, India pp: 1333-1347.
- Addiss DG, Shaffer N et al. The epidemiology of appendicitis and Appendectomy in the United States. Am J Epidemiol 132 (1996): 910-925.
- Luckmann R, Davis P. The epidemiology of acute appendicitis in California: racial, gender, and seasonal variation. Epidemiology 2 (1991): 323-330.
- Andersson RE, Hugander A, Thulin AJ. Diagnostic accuracy and perforation rate in appendicitis: association with age and sex of the patient and with appendicectomy rate. Eur J Surg 158 (1992): 37-41.
- Van Dieijen-Visser MP, Go PMNYH, Brombacher PJ. The value of laboratory tests in patients suspected of acute appendicitis. Eur J Clin Chem Clin Biochem 29 (1991): 749-752.
- Paulman AA, Huebner DM, Forrest TS. Sonography in the diagnosis of acute appendicitis. Am Fam Physician 44 (1991): 465-.468.
- Arshad K, Shafiullah. Significance of total leucocyte count in the diagnosis of acute appendicitis in children. Gomal journal of medical sciences 9 (2011): 90.
- Al-gaithy ZK. Clinical value of total white blood cells and neutrophil counts in patients with suspected appendicitis: retrospective study. World J Emerg Surg 7 (2012): 32.
- Graham Thompson. Clinical scoring systems in the management of suspected appendicitis in children, Appendicitis- A collection of essays from around the world, Dr.Anthony Lander (edtn) (2012).
- Petrosyan M, Barnhart J, Tao M, et al. Hyperbilirubinemia in appendicitis: a new predictor of perforation. Estrada JJ. J.Gastrointest Surg (2007): 714-718.
- De Carvalho BR, Diogo-Filho A, Fernandes C, et al. Leukocyte count, C-reactive protein, alpha-1 acid glycoprotein and erythrocyte sedimentation rate in acute appendicitis. Arq Gastroenterol 40 (2003): 25-30.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 