Fraser syndrome: About A Case and Review of the Literature
Laouali Laminou1a*, Oumarou Habou2a, Magagi Amadou3a, Abba Kaka Yakoura Hadjia4b, Amza Abdou5b
1Department of Ophthalmology, Zinder National Hospital, Niger.
2Department of Pediatric Surgery, Zinder National Hospital, Niger.
3Department of Anesthesia and Intensive Care, Zinder National Hospital, Niger.
4Department of Ophthalmology, Niamey National Hospital, Niger.
5Ophthalmology Department, Amirou Boubacar Diallo Hospital, Niamey, Niger.
aFaculty of Health Sciences, University of Zinder, Niger.
bFaculty of Health Sciences, Abdou Moumouni University of Niamey, Niger.
*Corresponding Author: Laouali Laminou, Department of Ophthalmology, Zinder National Hospital, Niger.
Received: 04 August 2022; Accepted: 12 August 2022; Published: 09 November 2022
Article Information
Citation: Laouali Laminou, Oumarou Habou, Magagi Amadou, Abba Kaka Yakoura Hadjia, Amza Abdou. Fraser syndrome: About A Case and Review of the Literature. Journal of Surgery and Research 5 (2022): 585-587.
View / Download Pdf Share at FacebookAbstract
Purpose: The aim of this study was to describe the management of a case of Fraser syndrome at the National Hospital of Zinder in Niger and review of the literature.
Observation: This was a newborn at day 1 of life, female, from a first degree consanguineous marriage referred from the mother and child health center (CSME) to the ophthalmology department of the national hospital of Zinder for polymalformative syndrome. On admission, he had complete bilateral cryptophthalmia, nasal depression and polydactyly. Bilateral ocular examination noted on bidigital palpation the presence of a renal globular mass behind the skin tissue. The general physical examination noted an umbilical hernia and simple polydactyly and the otorhinolaryngological examination did not reveal any other abnormalities apart from nasal depression.
Bilateral aphakia was found on ocular ultrasound and the abdomino-pelvic ultrasound showed a uterine inversion with no abnormalities in the urinary tree. Surgical exploration revealed an opaque cornea in the right eye that prevented further examination of the anterior segment.
Conclusion: Frazer's syndrome is a malformative syndrome that poses serious management difficulties, particularly in facilities with limited resources such as ours. An antenatal diagnosis and a multidisciplinary management are a guarantee of a functional and cosmetic prognosis.
Keywords
<p>Fraser, Bilateral cryptophtalmos, Aphakia, Uterine inversion, Zinder</p>
Article Details
Introduction
Fraser syndrome, also known as cryptophthalmosyndactyly syndrome, is a rare polymalformative syndrome characterized by cryptophthalmos (unilateral or bilateral), syndactyly, pulmonary, urogenital and other less frequent abnomalities (congenital obstruction of the nasolaryngeal, musculoskeletal, oro-facial, neurological, cardiovascular...) [1-3]. First described in 1962 by the Canadian geneticist Gorges Fraser, Fraser syndrome is a genetic syndrome (mutations in the FRAS1, FREM2 and GRIP1 genes) that is transmitted in an autosomal recessive mode [4,5]. Ocular abnomalities, dominated by cryptophthalmia, are the characteristic lesion of this syndrome. The management is complex and the vital prognosis remains poor in case of otolaryngological, pulmonary or renal anomalies [3]. We report a case of Frazer's syndrome and discuss the difficulties of managing this condition in a resource-limited setting.
Observation
A female infant was referred by the mother and child health center (CSME) to the ophthalmology department of the national hospital of Zinder for polymalformative syndrome. He was born to a first-degree consanguineous couple and was the sixth of his siblings. The pregnancy was poorly monitored, but there was no evidence of drug use, addiction or exposure to radiation. The delivery was at term, eutoctopic by vaginal delivery. Anthropometry of the newborn noted weight 2800 g, height 49 centimeters and head circumference at 32 centimeters. Examination of the newborn noted bilateral complete cryptophthalmos, nasal depression, polydactyly (Figure 1A). Bilateral ocular examination noted on bidigital palpation the presence of a renal globular mass behind the skin tissue (Figure 1A, blue arrow). General physical examination noted an umbilical hernia and simple polydactyly (Figure 1B). Otolaryngologic examination revealed no other abnormalities besides nasal depression. Two-dimensional ocular ultrasound showed aphakic eyeballs and a cystic mass over the left eye. The axial length was 19.1 mm on the right and 20.2 mm on the left, the optic nerves are well individualized (Figure 2A). Abdominal-pelvic ultrasound showed a uterine inversion without abnormalities in the urinary tree. Cardiac and transfontanellar ultrasound were normal. The requested karyotype could not be performed. At the surgical exploration, under general anesthesia we discovered in the right eye an opaque cornea that did not allow the rest of the examination of the anterior segment (Figure 2B).
Discussion
The prevalence is estimated at 0.2 cases per 100,000 live births [6,7]. The ethiopathogenesis remains debated and several theories have been proposed: a primary abnormality of eyelid formation with metaplasia of the corneal and conjunctival epithelium; a refusion of partially formed eyelids or a failure of programmed cell apoptosis that would result in utero in the opening of temporarily closed areas such as the eyelids, fingers, vagina and toes [8]. The notion of consanguinity has been described by many authors [2, 9,10]. This is the case of our patient whose father and mother are first cousins. Prenatal diagnosis can be evoked at obstetrical ultrasound around the 18th week of gestation; however, oligohydramnios makes this very difficult [10,11]. This diagnosis is often crucial for the therapeutic decision. Indeed, in case of early discovery in utero, with major renal anomalies (renal agenesis) or laryngeal atresia, some authors propose a termination of the pregnancy [11]. Postnatally, the diagnosis of fraser syndrome is based on the association of at least two major and one minor criteria or one major and at least four minor criteria (Tables I and II) [2,12]. In 2007 Van Haelst [2], after analysis of 59 cases of Fraser syndrome with the Fraser Syndrome Collaboration Group included airway and urogenital tract anomalies in the major criteria and cleft lip and mental retardation in the minor criteria (Table II). Our patient has two major criteria (cryptophthalmia and uterine inversion) and minor manifestations (polydactyly, umbilical hernia and nasal depression). In Fraser syndrome, also called cryptophthalmosyndactyly syndrome, polydactyly is rarely reported in the literature and is not a major criterion. Malformations of the gastrointestinal tract (especially anorectal anomalies) have not been included in the diagnostic criteria for Fraser syndrome although they have been frequently described in the literature [6,9]. Slavotinek [9] recommends that these abnormalities should be considered as minor criteria in the diagnosis of Fraser syndrome given their high frequency.
Frazer syndrome constitutes a major therapeutic challenge, requiring a multidisciplinary approach. The main objective of this treatment is the preservation of visual function and the creation of an aesthetic face by performing a palpebral reconstruction. There is no clear and well codified strategy for surgery of cryptophthalmos, according to Saley [13], the degree and type of cryptophthalmos are the 2 elements to take into account in the surgical indications. The functional prognosis of the eye is very often poor due to the structural abnormalities accompanying cryptophthalmos. In our case, the exploration revealed an opaque cornea in the right eye, which did not allow the rest of the examination of the anterior segment. The vital prognosis depends on the associated anomalies. It should be noted that twenty-five percent (25%) of affected children are stillborn, twenty percent (20%) die before the first year of life due to their renal malformations and/or laryngeal atresia. In the absence of renal agenesis, life expectancy can be considered normal [8,14].
Conclusion
Frazer syndrome is a malformative syndrome that poses serious management difficulties, particularly in resource-limited settings like ours. Ante-natal diagnosis and multidisciplinary management are a guarantee of a functional and cosmetic prognosis.
Conflict of interest
The authors declare no conflict of interest.

Figure 1: 1A complete cryptophthalmia, 1B Sample polydactyly right hand
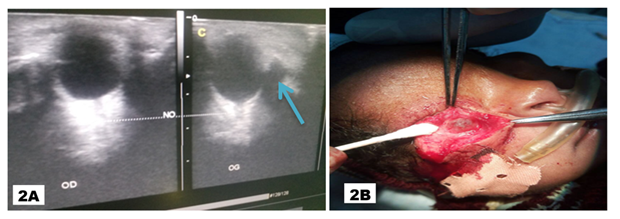
Figure 2: 2A Ocular ultrasound, in two-dimensional mode, showed the presence of aphakic eyeballs and a cystic mass opposite (blue narow) the left eye (OG )., 2B Intraoperative view with an opaque cornea
|
Major criteria |
Minor criteria |
|
- Cryptophtalmos |
- Nasal congenital malformations |
|
- Syndactyly |
- Congenital ear defects |
|
- Genital abnomalities |
- Congenital malformation of the larynx |
|
- First degree family history of Fraser Syndrome |
- Cleft lip ± palate |
|
- Abnomalities of the urinary tract and kidneys |
|
|
- Musculo-skeletal abnomalities |
|
|
- Ombilical hernia |
|
|
- Learning disability |
Table 1: Diagnostic criteria for Fraser syndrome [Thomas]
|
Major criteria |
Minor criteria |
|
- Cryptophthalmos |
- Nasal cogenital abnormalities |
|
- Syndactyly |
- Conenital ear defects |
|
- Anomalies génitales |
- Musculo-skeletal abnormalities |
|
- Urinary tract abnormalities |
- Umbilical hernia |
|
- Laryngeal and tracheal abnormalities |
- Learning disability |
|
- 1st degree family history of Fraser syndrome |
- Nasal congenital malformations |
|
- Congenital ear malformations |
Table 2: Modified diagnostic criteria for Fraser syndrome [Van Haelst]
References
- Fraser GR. Our genetical ‘load’. A review of some aspects of genetical variation. Ann Hum Genet 25 (1962): 387-415.
- Van Haelst MM, Scambler PJ, Group FSC, et al. Fraser syndrome: a clinical study of 59 cases and evaluation of diagnostic criteria. Am J Med Genet A 143 (2007): 3194-203.
- Beylerian M, Hugo J, Hadjadj È, et al. Fraser syndrome: Case report. J Fr Ophtalmol 41 (2018): e489-e490.
- Schanze D, Kayserili H, Satk?n BN, et al. Fraser syndrome due to mutations in GRIP1- clinical phenotype in two families and expansion of the mutation spectrum. Am J Med Genet A 164 (2013):837-840.
- Jadeja S, Smyth I, Pitera JE, et al. Identification of a new gene mutated in Fraser syndrome and mouse myelencephalic blebs. Nat Genet 37 (2005): 520-525.
- Barisic I, Odak L, Loane M, et al. Fraser syndrome: epidemiological study in a European population. Am J Med Genet A 161 (2013): 1012-1018.
- Bouaoud J, Olivetto M, Testelin S, et al. Fraser syndrome: review of the literature illustrated by a historical adult case. Int J Oral Maxillofac Surg (2020).
- Allali B, Hamdani M, Lamari H, et al. Syndrome de Fraser: À propos d′ un cas. J Fr Ophtalmol 29 (2006): 184-187.
- Slavotinek AM, Tifft CJ. Fraser syndrome and cryptophthalmos: review of the diagnostic criteria and evidence for phenotypic modules in complex malformation syndromes. J Med Genet 39 (2003): 623-633.
- Touré A, Diomandé IA, Nouraly H, et al. Cryptophtalmie bilatérale dans un syndrome de Fraser: à propos d’un cas et revue de la littérature. J Fr Ophtalmol 38 (2015): e97-100.
- Tuuli MG, Odibo AO. Fraser Syndrome. In: Obstetric imaging: fetal diagnosis and care. Elsevier 11 (2018): 547-549.
- Thomas IT, Frias JL, Felix V, et al. Isolated and syndromic cryptophthalmos. Am J Med Genet 25 (1986): 85-98.
- Saleh GM, Hussain B, Verity DH, et al. A surgical strategy for the correction of Fraser syndrome cryptophthalmos. Ophthalmology 116 (2009): 1707-1712.
- Karas DE, Respler DS. Fraser syndrome: a case report and review of the otolaryngologic manifestations. Int J Pediatr Otorhinolaryngol 31 (1995): 85-90.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 