Long-term survival after Cranio-cervical disjuction in a Ankylosing spondylitis patient: A case report and review of the literature
Inverso M, Borruto MI*, Zirio G, Genitiempo M, Velluto C, Mazzella GG, Ingusci D, Proietti L, Scaramuzzo L
Department of Aging, Orthopaedic and Rheumatological Sciences, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy
*Corresponding Author: Maria Ilaria Borruto, Fondazione Policlinico Universitario A. Gemelli IRCCS, Largo A. Gemelli, 8, 00168 Roma, Italia.
Received: 04 April 2025; Accepted: 09 April 2025; Published: 31 July 2025
Article Information
Citation: Inverso M, Borruto MI, Zirio G, Genitiempo M, Velluto C, Mazzella GG, Ingusci D, Proietti L, Scaramuzzo L. Long-term survival after Cranio-cervical disjuction in a Ankylosing spondylitis patient: A case report and review of the literature. Journal of Surgery and Research. 8 (2025): 379-385
View / Download Pdf Share at FacebookAbstract
Introduction: Ankylosing spondylitis (AS) is a chronic inflammatory disease affecting the axial skeleton, leading to progressive ossification and spinal rigidity. These biomechanical alterations render patients highly susceptible to spinal fractures, even from low-energy trauma. Among these, cranio-cervical disjunction (CCD) is an extremely rare and often fatal injury. This case report describes the unprecedented survival of a 52-yearold male with AS who sustained multiple vertebral fractures, including a CCD, after a high-speed motorcycle accident. The case highlights the clinical complexity and importance of early multidisciplinary intervention.
Materials and Methods: We conducted a systematic review of Englishlanguage literature indexed in PubMed and Google Scholar using the search terms “ankylosing spondylitis” AND “spine fractures” OR “atlantooccipital dislocation.” Of 238 records, eight studies met inclusion criteria: case reports or series involving AS patients with CCD or multiple vertebral fractures. Data on demographics, neurological status, and survival were extracted and compared to our case.
Discussion: Our patient presented with life-threatening injuries, including CCD, bilateral pneumothorax, vertebral artery bleeding, and multiple spinal fractures. A comprehensive and aggressive management strategy was implemented: early airway control, targeted resuscitation, damagecontrol spinal fixation, vertebral artery embolization, and staged definitive surgery. Despite severe complications such as infections, pressure ulcers, thrombosis, and cranial nerve palsy, the patient survived for seven months—markedly longer than any other reported case of CCD in AS patients. Literature analysis revealed that survival beyond 7 days in such cases is exceedingly rare, with most patients succumbing within a week regardless of the number or location of fractures, or neurological status.
Conclusion: This case illustrates that prolonged survival after CCD in AS is possible through immediate, multidisciplinary intervention and sustained intensive care. It challenges existing notions of prognosis in AS-related spinal trauma and emphasizes the need for standardized protocols. Future research should explore whether aggressive, staged treatment strategies can systematically improve outcomes in this high-risk population.
Keywords
<p>Ankylosing spondylitis, Cranio-cervical disjunction, Spinal fractures, Atlanto-occipital dislocation</p>
Article Details
Introduction
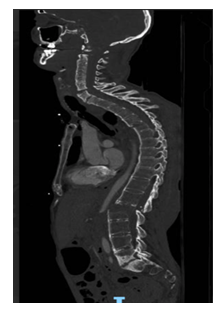
Axial spondyloarthritis, also known as ankylosing spondylitis (AS), is a chronic inflammatory disease that primarily affects the axial skeleton. The ongoing inflammation eventually leads to the progressive stiffening and fusion of the vertebrae, a process referred to as ankylosis, which in advanced stages causes the spine to take on a "bamboo" appearance. This rigidity severely limits spinal mobility and can result in significant pain and disability.
Patients with ankylosing spondylitis are at a notably higher risk of vertebral fractures due to the structural changes in their spines. The ossification of ligaments and joints causes the spine to become rigid, making it more vulnerable to fractures, even from minor trauma. The reduced ability of the vertebrae to absorb impacts increases the likelihood of complex fractures.
This case report details the clinical course, diagnostic challenges, and multidisciplinary management of a 52-year-old male patient with a history of ankylosing spondylitis who sustained multiple severe injuries in a motorcycle racing accident. Among the numerous spinal injuries, the patient suffered a cranio-cervical disjunction, a traumatic occurrence that is frequently fatal due to the severe instability and damage it causes to the upper cervical spine and brainstem. Remarkably, despite the typically poor prognosis associated with this injury.
Case Report
We present the case of a 52-year-old male with a medical history of ankylosing spondylitis who was involved in a high-speed motorcycle accident, while racing on a track. Upon arrival at the scene, emergency responders found him unconscious, necessitating immediate intubation to secure his airway and stabilize his breathing. This intervention was crucial in ensuring his survival and preparing him for rapid transport.
Given the patient's critical state, the decision was made to transport him via helicopter to our II level DEA center. This reduced transport time and allowed swift medical intervention.
Upon the patient’s arrival, immediate and comprehensive assessment and stabilization were paramount. The patient was immobilized using a spinal board and a cervical collar to prevent any potential exacerbation of his injuries. He was already intubated and connected to a transport ventilator, ensuring a secure airway.
On examining his breathing, we noted a significant reduction in bilateral breath sounds, indicating compromised lung function. Additionally, there was minimal subcutaneous emphysema, and both sides of his chest exhibited reduced expansion. His circulation status was dire; he presented with severe hypotension, recording a blood pressure of 58/30 mmHg, alongside a heart rate of 88 bpm. His skin was pale, with prolonged capillary refill and notably weak peripheral pulses, suggesting a critical state of shock.
Blood gas analysis revealed a pH of 7.225, indicating acidosis, with elevated PvCO2 at 66 and PvO2 at 35. His hemoglobin was 11.9, potassium at 5.4, lactate at 3, and base excess at -0.4, painting a picture of significant metabolic disturbance. The EFAST examination was negative for free fluid, but bilateral pleural sliding was absent, further pointing towards pneumothorax.
Given these findings, we promptly initiated intravenous fluid resuscitation, administered tranexamic acid and fibrinogen, and started a continuous infusion of norepinephrine to support his hemodynamic status. A chest X-ray confirmed the presence of bilateral pneumothorax, necessitating the placement of bilateral chest drains, which resulted in partial improvement of his hemodynamic stability.
In our neurological assessment, we identified anisocoria with the right pupil being larger than the left. Neurologically, he exhibited open eyes with a rightward lateral gaze deviation and complete absence of movement in all four limbs, alongside jugular venous distension, indicating possible severe intracranial or spinal pathology. Orthopedically, a suspected right shoulder dislocation was confirmed and promptly reduced.
Imaging, particularly a CT scan of the total body, revealed extensive traumatic injuries. Thoracic findings included bilateral pneumothorax, pulmonary contusions, and centrilobular and paraseptal emphysema, alongside multiple rib fractures and associated soft tissue hematomas. Abdominal imaging identified an extensive prevertebral hematoma and multiple areas of active bleeding, yet no traumatic organ injuries were noted. Cranio-cervical imaging showed severe dissociation between C1 and C2, multiple vertebral fractures, spinal cord involvement, and active bleeding from the right vertebral artery. Intracranial findings included an extra-axial haemorrhage, obliterated basal cisterns, and potential pontine haemorrhage.
Embolization of the right vertebral artery and segmentary lumbar vessels was performed in interventional radiology. This procedure was crucial for stabilizing the patient, as it controlled active bleeding and reduced the risk of hemorrhage, which was vital for the patient's survival. Furthermore, the embolization played a key role in the subsequent surgical strategies by minimizing intraoperative blood loss, allowing for safer and more effective spinal stabilization procedures. However, the patient was brought into the room on noradrenalin and went into cardiac arrest once he was prone. However, the patient was brought into the room on noradrenalin and went into cardiac arrest once he was prone. He was immediately resuscitated and once haemodynamically stabilised, surgical procedures began.
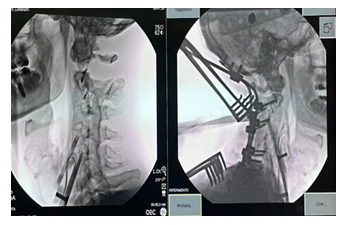
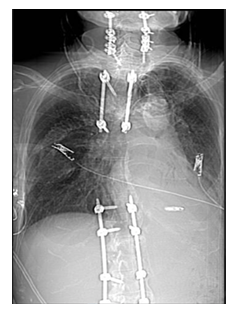
Given the patient's critical clinical condition, a damage control approach was chosen. This involved performing percutaneous fixation of both the lumbar and thoracic fractures, followed by the application of a halo vest for temporary stabilization. This strategy was essential to quickly stabilize the spinal injuries while minimizing the risk associated with a more extensive surgical intervention at that time, allowing for future definitive treatments once the patient’s condition had improved.
In the intensive care unit, the patient received continuous hemodynamic and respiratory monitoring. Follow-up interventions included maintaining continuous ventilation via tracheostomy, administering broad-spectrum antibiotics for infection management, and placing a pacemaker to address severe bradycardia. Thoracic surgeons managed the chest drains, and subsequent surgeries involved hematoma drainage and final cranio-cervical stabilization: the patient was placed under general anesthesia and positioned prone with Halo suspension. After disinfection and removal of previous sutures, multiple dorsal pressure sores were noted. The skin was disinfected, and a sterile operative field was prepared. A midline incision was extended from the occiput to T1, followed by bilateral dissection and exposure of the spine.
During preparation, diastasis at C1-C2 was identified, with complete rupture of the left lateral ligamentous complex, an isthmic fracture, avulsion of the C2 nerve root, and significant cerebrospinal fluid (CSF) leakage. Using the instrumentation system, screws were placed in the lateral masses of C3, C5, C6, and C7, the left lateral mass of C2, and the right pedicle of C2. Bilateral screws were also placed in the T1 pedicles. An occipital plate was secured, and the construct was stabilized with two contoured rods.
Under fluoroscopic guidance, reduction maneuvers were performed to address the C1-C2 dislocation. All components were secured with a dynamometric wrench. The surgical field was irrigated thoroughly, and Tachosil patches with fibrin glue were applied. Two subfascial drains were placed—one on the left for gravity drainage and one on the right with suction. Layered closure of the incision was performed, and the area was dressed appropriately.
At the end of the procedure, the Halo ring was removed, and a cervical collar was applied.
Throughout his hospital course, the patient encountered several complications. Infectiously, he developed Klebsiella oxytoca bacteremia and MSSA from a catheter tip, both treated with targeted antibiotics. Vascularly, he was diagnosed with popliteal vein thrombosis, managed with anticoagulants. Neurologically, new-onset horizontal diplopia was noted, and MRI scans ruled out intracranial causes, leading to a diagnosis of right cranial nerve VI palsy.
Two months after his arrival, the patient remains in the neuro-intensive care unit, having undergone multiple complex surgeries. He continues to receive comprehensive multidisciplinary care to address his extensive injuries and associated complications.
Due to his prolonged immobility, severe decubitus ulcers developed, requiring multiple plastic surgeries for wound closure. These ulcers were particularly difficult to manage due to the patient’s tetraplegia and extended periods of immobility in the supine position. Each surgery was coordinated with the broader medical team to ensure hemodynamic stability.
The patient also experienced popliteal vein thrombosis, which was treated with anticoagulation therapy. Neurologically, new-onset horizontal diplopia was noted, and imaging ruled out intracranial causes. The condition was diagnosed as right cranial nerve VI palsy, likely secondary to trauma.
The patient remains in the neuro-intensive care unit for 4 months. He has undergone multiple surgeries and comprehensive multidisciplinary care. 7 months after the accident, the patient died as a result of pulmonary complications.
Material and methods, demographic and Clinical Analysis of Selected Cases
We performed a systematic review of English literature indexed in PubMed and Google Scholar databases using as search-terms “ankylosing spondylitis” AND “spine fractures” (106) OR “atlanto-occipital dislocation”, finding 238 articles.
Two authors (M.I and M.I.B..) independently screened titles, abstracts and full-text papers, and any discordance was solved.
At the end of the screening of 238 manuscripts, 8 papers were included in our review, since they met our inclusion criteria which were:
• Case report/case series
• cranio-cervical disjunction (or at least multiple vertebral fractures)
• spondylitic patients
The analysis included a total of 8 patients with ankylosing spondylitis who sustained spinal trauma. The patients' ages ranged from 46 to 74 years, with a predominance of males. Only one case (12.5%) presented with cranio-cervical disjunction (CCD), while the remaining patients had multiple vertebral fractures at other levels (cervical, thoracic, and lumbar), with an average of more than two fractures per patient.
In terms of survival, all cases with available data reported a maximum survival of 7 days, regardless of the presence of CCD, the number of fractures, or the neurological status (classified according to the ASIA scale). Specifically, the average survival in patients with CCD was 7 days, identical to that of patients without CCD. Similarly, patients with an ASIA A classification (indicating complete neurological injury) had an average survival of 7 days, while complete data were not available for other ASIA categories (e.g., E).
The number of fractures also did not appear to significantly influence survival: both patients with more than two fractures and those with one or two fractures consistently showed a survival duration of 7 days. These findings, though preliminary, suggest that the severity of trauma in this patient population — regardless of lesion distribution or neurological impairment — often leads to a poor prognosis within a very short time frame.
Discussion
The management of spinal fractures in patients with ankylosing spondylitis (AS) represents a major challenge due to the intrinsic biomechanical alterations of the rigid spine. The literature extensively reports poor outcomes associated with cervical and thoracic fractures in AS patients, often leading to high mortality rates, particularly in cases involving cranio-cervical disjunction [1-4]. Our case stands out as a unique occurrence where a patient not only survived a cranio-cervical disjunction but has continued to receive multidisciplinary care for an extended period, a scenario rarely documented in previous studies [5].
Spinal fractures in AS patients frequently occur even with minor trauma due to the brittle nature of the ossified spine [2,3,6]. Several case reports and reviews highlight the severe consequences of vertebral fractures in AS, often leading to permanent disability or death [1,3,7]. For example, Samartzis et al. reported an 81-year-old patient with multiple spinal fractures following minor trauma, who ultimately succumbed to pulmonary complications within three months [3]. Similarly, Yagi et al. documented a case of double spinal fractures (cervical and lumbar) in an AS patient, resulting in fatal outcomes despite surgical intervention [1]. Other studies confirm that delayed diagnosis and inadequate stabilization lead to worsened prognoses [4,8]. Liang et al. reported a case of complete atlantoaxial dissociation in an AS patient who died seven days after admission, despite intensive treatment—highlighting the extreme lethality of such lesions in this population [16].
Unlike these cases, our patient survived despite sustaining one of the most catastrophic injuries in the context of AS. The unprecedented long-term survival in our case underscores the vital role of an early and aggressive multidisciplinary approach in managing such injuries [5].
One of the critical differentiating factors in our case is the application of a well-coordinated multidisciplinary strategy, which played a crucial role in patient survival. The integration of trauma surgeons, orthopedic specialists, intensivists, plastic surgeons, and infectious disease specialists ensured comprehensive management at every stage of care [1,2,9].
Early diagnosis and immediate immobilization were key factors in stabilizing the patient and preventing further neurological deterioration. Studies have shown that delayed diagnosis in AS patients leads to worsened outcomes due to secondary neurological damage and increased mortality [2,3,10]. Our rapid response with prehospital airway management, expedited transport, and emergency embolization of the vertebral artery significantly contributed to the patient's survival [1,6].
Furthermore, surgical intervention was meticulously planned to minimize intraoperative blood loss and reduce further spinal instability. Literature suggests that hybrid approaches combining open and percutaneous fixation can reduce surgical morbidity [1,11]. However, given the severity of the cranio-cervical disjunction, our case required a fully open approach with occipito-thoracic fusion, which was essential for achieving stability [3,12].
AS patients with spinal fractures often experience severe postoperative complications, including infections, pressure ulcers, and thromboembolic events [2,5]. In our case, the patient developed Klebsiella oxytoca bacteremia and methicillin-sensitive Staphylococcus aureus (MSSA) catheter-related infection, both of which were successfully managed with targeted antibiotic therapy [1,9]. Additionally, severe decubitus ulcers required multiple plastic surgeries, an aspect often underreported in literature but crucial in the long-term management of immobilized patients [2,13].
Thromboembolic events are another significant concern in AS patients with prolonged immobility [1,5]. Our patient developed popliteal vein thrombosis, which was promptly addressed with anticoagulation therapy. Neurologically, the onset of horizontal diplopia led to extensive neuroimaging studies, ultimately diagnosing cranial nerve VI palsy [2,7].
The survival of our patient, despite the devastating nature of his injuries, underscores the necessity of a proactive, multidisciplinary approach in managing AS-related trauma. The literature consistently highlights high mortality rates associated with cervical and thoracic fractures in AS, but our case challenges these statistics by demonstrating that long-term survival is achievable with optimal intervention [1-3,10].
As we can see from the table 1, maximum survival in patients with ankylosing spondylitis and cranio-cervical disjunction does not exceed 7 days, highlighting the severity of the fracture and the resulting clinical condition. This is consistent with several reported cases where patients expired within a week of injury despite receiving immediate care [16,17].
It is worth emphasizing that, in the majority of reported cases in literature, particularly in the presence of cranio-cervical disjunction (CCD), patients typically die instantly or are already deceased by the time emergency responders arrive. Even with timely on-site medical intervention, survival is usually not achievable, especially in individuals with a normal, non-pathological spine. In the specific case we describe, however, ankylosing spondylitis may have played a paradoxically protective role. Due to the extensive ossification and fragmentation of the spinal structures typical of the disease, spinal mobility is significantly reduced. This biomechanical rigidity may have prevented the odontoid process from migrating upward and impinging upon the medullary respiratory centers in the brainstem, which often leads to immediate death in cases of CCD. This unique biomechanical context might partially explain the exceptional survival observed in our patient.
Table 1: Reported cases of pediatric traumatic lumbosacral or thoracolumbar facet dislocations. The table summarizes demographic data, injury mechanisms, affected spinal levels, neurological status at admission (ASIA scale), surgical approaches, and outcomes as described in the literature.
An interesting case report [14] describes a 9-year-old girl who managed to survive an atlanto-occipital dislocation. However, the report emphasizes the remarkable ability of patients at that age to recover vital functions, the single fracture and especially how the absence of comorbidities played a crucial role.
Osgood et al. emphasized the extreme instability of cervical and thoracic fractures in AS patients, often leading to sudden neurological deterioration even with minor movements during patient handling. In one such case, despite aggressive management, the patient died within seven days [17]. Bernini et al. similarly reported the extreme vulnerability of the ankylosed spine to multiple fractures with minor trauma, reinforcing the concept that even stable-appearing patients can harbor life-threatening injuries if AS or hyperostosis is present [18].
In our case, the multidisciplinary approach and immediate trauma management were the key in allowing the patient to continue experiencing the affection of their loved ones for a longer period than any other patient in similar conditions with the same type of fractures.
Future research should focus on establishing standardized protocols for the early management of AS-related spinal fractures, emphasizing the need for rapid diagnosis, early surgical stabilization, and comprehensive postoperative care [2,4]. The role of hybrid surgical techniques in managing complex AS fractures should also be further explored, as minimally invasive approaches may offer benefits in select cases [1,6].
Conclusion
This case report presents an unprecedented long-term survival following cranio-cervical disjunction in an AS patient, highlighting the crucial role of a multidisciplinary approach. Unlike previously reported cases where similar injuries resulted in high mortality, our patient’s outcome demonstrates that aggressive and well-coordinated management can lead to extended survival, even in the most severe scenarios [1,2,3]. The integration of early surgical intervention, meticulous hemodynamic and infectious disease management, and continuous multidisciplinary care were pivotal in achieving this exceptional outcome [5]. Further studies should aim to refine treatment algorithms for AS-related spinal trauma, ensuring that similar success stories become more common in clinical practice [10].
References
- Sebastian AS, Fogelson JL, Dekutoski MB, et al. Multiple noncontiguous spinal fractures and occipitocervical dislocation in a patient with ankylosing spondylitis treated with a hybrid open and percutaneous spinal fixation technique: a case report. Spine J 15 (2015): e1-5.
- Schaefer RO, Rutsch N, Schnake KJ, et al. Rigid spine injuries - A comprehensive review on diagnostic and therapeutic challenges. Brain Spine 4 (2024): 102811.
- Samartzis D, Anderson DG, Shen FH. Multiple and simultaneous spine fractures in ankylosing spondylitis: case report. Spine (Phila Pa 1976) 30 (2005): E711- E715.
- Anwar, Fahim et al. Concomitant cervical and thoracic spinal fractures in ankylosing spondylitis: A case report and review of literature. Injury Extra 40 (2009): 242-245.
- Hitchon PW, From AM, Brenton MD, et al. Fractures of the thoracolumbar spine complicating ankylosing spondylitis. J Neurosurg 97 (2002): 218-222.
- Caron T, Bransford R, Nguyen Q, et al. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976) 35 (2010): E458-464.
- Lukasiewicz AM, Bohl DD, Varthi AG, et al. Spinal Fracture in Patients With Ankylosing Spondylitis: Cohort Definition, Distribution of Injuries, and Hospital Outcomes. Spine (Phila Pa 1976) 41 (2016): 191-196.
- Yagi M, Sato S, Miyake A, et al. Traumatic Death due to Simultaneous Double Spine Fractures in Patient with Ankylosing Spondylitis. Case Rep Orthop 2 (2015): 590935.
- Waldman SK, Brown C, Lopez de Heredia L, et al. Diagnosing and managing spinal injury in patients with ankylosing spondylitis. J Emerg Med 44 (2013): e315- e319.
- Kai K, Ikuta K, Masuda K, et al. Surgical Outcomes of Minimally Invasive Stabilization for Spinal Fractures in Patients with Ankylosing Spinal Disorders. Asian Spine J 12 (2018): 434-441.
- Ushijima T, Kawaguchi K, Matsumoto T, et al. Double non-contiguous fractures in a patient with spondylo-epiphyseal dysplasia with spinal ankylosis treated with open and percutaneous spinal fixation technique: a case report. BMC Res Notes 11 (2018): 106.
- Yagi M, Sato S, Miyake A, et al. Traumatic Death due to Simultaneous Double Spine Fractures in Patient with Ankylosing Spondylitis. Case Rep Orthop 20 (2015): 590935.
- Hunter T, Dubo H. Spinal fractures complicating ankylosing spondylitis. Ann Intern Med 88 (1978): 546-549.
- Salinsky JP, Scuderi GJ, Crawford AH. Occipito-atlanto-axial dissociation in a child with preservation of life: a case report and review of the literature. Pediatr Neurosurg 43 (2007): 137-141.
- Liang CL, Lu K, Lee TC, et al. Dissociation of atlantoaxial junction in ankylosing spondylitis: case report. J Trauma 53 (2002): 1173-1175.
- Osgood CP, Abbasy M, Mathews T. Multiple spine fractures in ankylosing spondylitis. J Trauma 15 (1975): 163-166.
- Bernini PM, Floman Y, Marvel JP Jr, et al. Multiple thoracic spine fractures complicating ankylosing hyperostosis of the spine. J Trauma 21 (1981): 811-814.
Article Views: 722
Journal Statistics




Discover More: Recent Articles
Grant Support Articles
© 2016-2026, Copyrights Fortune Journals. All Rights Reserved!