Mesenteric Pseudocyst Following Blunt Abdominal Trauma: Report of a Case and Review of Literature
Klaudia Gjinoska1*, Ognen Kostovski2, Andrej Nikolovski3, Daniela Bajdevska Dukoska4, Agron Alimi5, Svetozar Antovic2
1Faculty of Medicine, University "Ss. Cyril and Methodius", Skopje, North Macedonia
2University Clinic Digestive Surgery, Clinical Center "Mother Theresa", Skopje, North Macedonia; Faculty of Medicine, University "Ss. Cyril and Methodius", Skopje, North Macedonia
3University Clinic for Surgery "Sv. Naum Ohridski", Skopje, North Macedonia; Faculty of Medicine, University "Ss. Cyril and Methodius", Skopje, North Macedonia
4Institute of Pathology, Medical Faculty, University "St. Cyril and Methodius", Skopje, Republic of Macedonia; Faculty of Medicine, University "Ss. Cyril and Methodius", Skopje, North Macedonia
5General Hospital, Kumanovo, North Macedonia
*Corresponding Author: Klaudia Gjinoska, Faculty of Medicine, University "Ss. Cyril and Methodius", Skopje, North Macedonia
Received: 29 September 2022; Accepted: 06 October 2022; Published: 12 October 2022
Article Information
Citation: Klaudia Gjinoska, Ognen Kostovski, Andrej Nikolovski, Daniela Bajdevska Dukoska, Agron Alimi, Svetozar Antovic. Mesenteric Pseudocyst Following Blunt Abdominal Trauma: Report of a Case And Review of Literature. Journal of Surgery and Research. 5 (2022): 555-560.
View / Download Pdf Share at FacebookAbstract
Mesenteric pseudocysts are rare intraabdominal lesions. A total of 29 similar case reports were retrieved via the Medline/PubMed search engine. They represent a subtype of mesenteric cysts displaying histological similarity to pancreatic pseudocysts which are usually surrounded by a thick fibrous wall without an inner epithelial lining. Mesenteric pseudocysts may present as any other expanding intraabdominal lesion. Accurate preoperative characterization of mesenteric cystic lesions remains challenging. Imaging diagnostics for most of the cases involve both ultrasound and computerized tomography. It is unclear whether routine MRI use would increase preoperative diagnostic accuracy and aid in preoperative planning. Total surgical excision of the pseudocyst has been the treatment of choice. Surgical removal has been achieved by means of open surgery, laparoscopy and the robotic system. It remains unclear to this date whether other treatment approaches are feasible. Other options such as debridement, marsupialization or partial excision have been considered inadequate due to concerns such as the possibility of malignant cell seeding, septic complications and risk of recurrence. We present the case of a posttraumatic mesenteric pseudocyst following blunt abdominal trauma in a 27 year old female, treated by surgical excision.
Keywords
<p>Mesenteric cyst, Mesenteric pseudocyst, Blunt abdominal trauma</p>
Article Details
Introduction
Mesenteric pseudocysts are rare intraabdominal lesions. Trauma and infection have been discerned as possible causes, by means of hematoma or abscess resorption [1]. De Perrot’s histopathology classification of mesenteric cysts placed pseudocysts within a separate group, absence of epithelial lining being the common denominator. A total of 29 case reports were retrieved via the MedLine/PubMed search engine. The aim of this paper was to report a case of a mesenteric pseudocyst following blunt abdominal trauma and to review other previously published cases regarding this pathology.
Case Presentation
This is the case of a 27 year old female complaining of chronic abdominal pain for a few months prior to consult in the outpatient clinic. The aches were described as constant, dull, located in the mid abdominal region. Detailed interview brought to light an incident of blunt abdominal trauma that occurred 4-5 months earlier. Physical examination in the outpatient clinic was significant for abdominal tenderness in a wider area to the left of the umbilicus. Deep palpation did not reveal any abnormal growths. All lab values, including the serologic tumor markers fell within their reference ranges. The cystic lesion was first noted on ultrasound exam. Contrast enhanced computerized tomography (CT) scan and MRI were ordered for further characterization. The following traits were depicted by the cystic lesion on CT imaging: distinct margins, thin wall with subtle contrast enhancement, heterogeneous contents, and thick sediment. This round lesion measured 7cm x 6cm x 6,5cm and pushed away surrounding bowel (Figure 1a & 1b). MRI confirmed the CT diagnosis of a cystic fluid filled lesion, thick sediment, and mass-effect on adjacent bowel (Figure 2a,2b). The patient was scheduled for open surgery. Figure 3 presents the mesenteric pseudocyst enveloped by two peritoneal leaves of small bowel mesentery. The removed mesenteric pseudocyst is shown in figure 4. It was incompressible with slight elasticity upon pressure. Despite meticulous dissection, mesenteric vessel thrombosis led to segmental bowel ischemia, forcing segmental bowel resection. The postoperative period was uneventful. The patient was discharged on postoperative day 5. Pathological analysis revealed a unilocular cystic lesion filled with thick yellow-brown fluid with uneven inner surface. The following measurements were noted: weight 164g, size 7cm x 7cm x 5cm, wall thickness 3-4mm. Microscopic analysis was notable for the absence of epithelial lining, presence of collagen and smooth muscle fibers and chronic inflammation (See figure 5). The chronic inflammatory infiltrate consisted of the predominant lymphocyte population, the occasional lymphoid aggregate and foamy macrophages. The latter are scattered along the inner surface of the wall (Figure 6). Immunohistochemistry analysis yielded the following results: LCA+, CD68+, MCA -, CKAE1/AE3 -, CK7-, CD56-, CD10-.
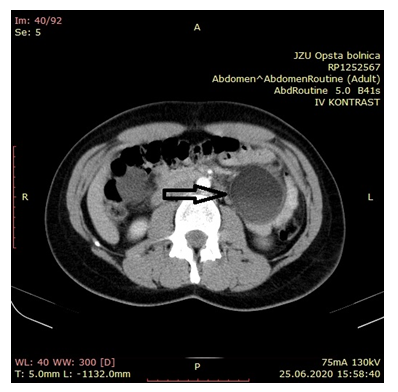
Figure 1a: Contrast CT image of mesenteric pseudocyst axial plane
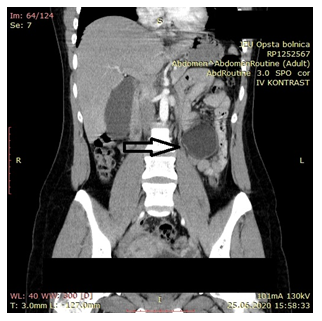
Figure 1b: Contrast CT image of mesenteric pseudocyst coronal plane
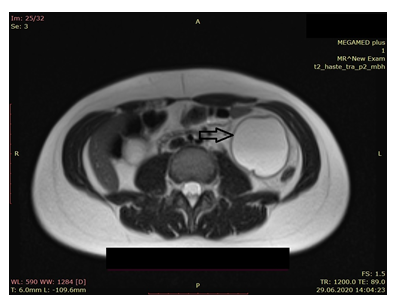
Figure 2a: Non-contrast MRI of mesenteric pseudocyst axial plane
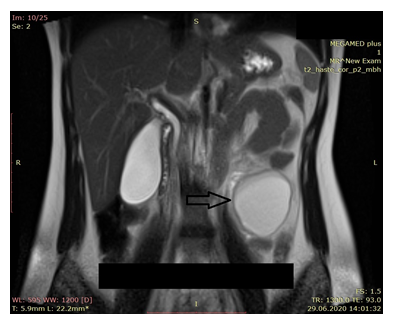
Figure 2b: Non-contrast MRI of mesenteric pseudocyst coronal plane
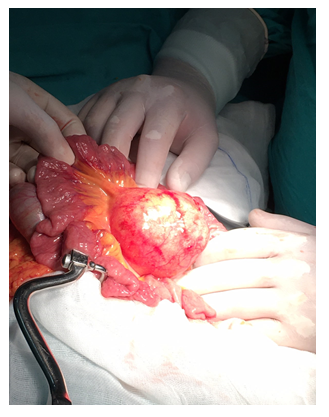
Figure 3: The mesenteric pseudocyst on exploration
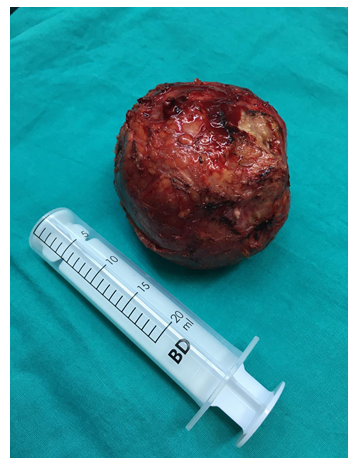
Figure 4: Removed specimen
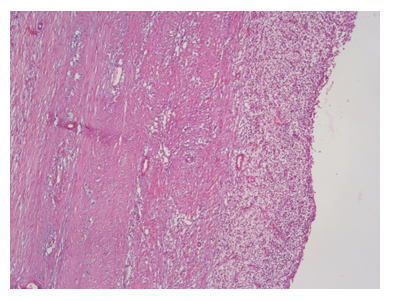
Figure 5: Microphotograph of the pseudocyst wall lacking epithelium (H&E x 5)
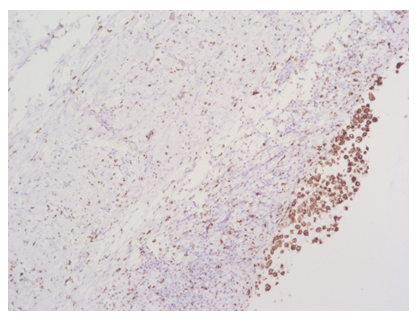
Figure 6: Pseudocyst wall, immunohistochemistry CD68 positive histiocytes, 10x
Discussion
Mesenteric cyst is a term referring to all the cystic and pseudocystic lesions arising from the retroperitoneum, mesentery and omenta. Although some authors define mesenteric cysts as cyst arising exclusively from the bowel mesentery, we believe this practice to be inadequate for three reasons: 1. as dePerrot depicts, retroperitoneal, omental and mesenteric cysts derive from the same embryological structures 2. In many cases it is impossible to determine the exact anatomic origin of the cyst on preoperative imaging and intraoperative exploration [1]. 3. Scientific research would be simpler if all cystic and pseudocystic lesions arising independently from abdominal viscera are named mesenteric cysts.
Mesenteric cysts (retroperitoneal, mesenteric and omental) are rare lesions with an average incidence of 1/100 000 hospital admissions in adults [1]. The occurrence of mesenteric pseudocyst is quite rare, the number of published cases amounting to several dozen. Although rare, mesenteric cysts should be included in the differential for an abdominal cystic lesion detected by ultrasound or CT.
Mesenteric cysts are classified into six groups as follows: 1. cysts of lymphatic origin, 2. cysts of mesothelial origin, 3. cysts of enteric origin, 4. cysts of urogenital origin, 5. mature cystic teratoma, 6. nonpancreatic pseudocysts [1]. Traumatic and infectious pseudocysts are histogically similar to pancreatic pseudocyst which are usually surrounded by a thick fibrous wall without an inner epithelial lining [1].
Mesenteric cysts (including pseudocysts) may present as any other expanding intraabdominal lesion. Symptoms arise mainly from compression and displacement of adjacent structures, therefore, dull abdominal pain is the most common presenting symptom. Rarely, they present as a surgical emergency due to rupture of the cyst/pseudocyst or torsion of the mesentery.
There are several clinical scenarios at the time of diagnosis of mesenteric cysts. The most common scenario is intermittent abdominal pain and discomfort in one or more quadrants, with or without a palpable abdominal mass [2-6]. Another common scenario is the acute onset of intense abdominal pain in one quadrant, abdominal tenderness and sings of systemic inflammation (elevated heart rate, elevated body temperature, elevated CRP, leukocystosis, loss of appetite, nausea) [7-10]. An abdominal mass might or might not be palpable. Other clinical scenarios include midgut volvulus, partial or complete small bowel obstruction [11,12], hemiabdominal swelling and abdominal mass on palpation [13], disappearing and migrating abdominal mass [14]. Sometimes the mesenteric cyst is discovered as an incidental finding while diagnosing and treating for other conditions [15-17].
Primary retroperitoneal pseudocysts present in a slightly different fashion. Constant dull aching in one or two quadrants and/or palpable mass is the most common mode [18-24]. Possible additional symptoms include vomiting and a feeling of fullness. On single occasions the retroperitoneal pseudocyst has presented as bilateral reducible groin swellings [25], acute onset right lower quadrant pain increasing in severity with concomitant leukocytosis [26], has been discovered incidentally [27], and presented only as a palpable mass [28].
The majority of cases mesenteric pseudocyst either don’t report or specifically deny a history of abdominal trauma. There are four cases reporting a history of blunt abdominal trauma, including a knee-kick, a traffic accident and a fall injury [3,4,12,29]. Therefore, lacking abdominal trauma history should not exclude the traumatic mesenteric cyst from the differential.
Traditionally ultrasound been considered as the primary modality for differentiating cystic and solid lesions and unilocular from multilocular lesions, CT offers the advantage of good spatial resolution, and MRI is best for tissue differentiation. MRI is not routinely obtained in the case of the mesenteric cystic lesion. In one case MRI determined the nonpancreatic origin of the cyst [3]. Magnetic resonance non-contrast series added little value to the investigative process in our case. It is unclear whether routine MRI use would increase preoperative diagnostic accuracy and aid in preoperative planning.
Pseudocysts display varying imaging characteristics, making correct preoperative diagnosis unlikely (see table). Distinct margins and compressing/displacing parenchymal organs and vascular structures are consistent features but common to all benign intraabdominal lesions. The mass-effect is only evident with larger lesions, but goes unnoticeable with lesions sized 5cm or less.
Total surgical excision of the nonpancreatic pseudocyst has been cited as the treatment of choice by all the authors. Total removal has been accomplished by enucleating using blunt and sharp dissection or by means of segmental bowel resection. Other options such as debridement, marsupialization, or partial excision have been considered inadequate due to concerns such as the possibility of malignant cell seeding, septic complications and risk of recurrence. These concerns arise generally as a consequence of diagnostic uncertainty. Benign cystic mesotheliomas and lymphangiomas have been shown to recur when incompletely resected [1]. However such occurrence hasn’t been demonstrated for the nonpancreatic pseudocyst. If diagnostic uncertainty weren’t an issue, attempts at treating the nonpancreatic pseudocyst as the pancreatic pseudocyst might yield satisfactory results, given their histopathological resemblance. Approaches other than total surgical excision might eliminate the necessity for extensive resection including adjacent bowel or parenchyma.
Segmental bowel resection has been performed for the following reasons: inability to exclude malignancy [6], avoiding rupture and spillage [6], intimate involvement of mesenteric vessels by the pseudocyst wall [4,14,15], proximity to bowel wall [10,15]. Wedge resection of the stomach [16] and removal of the left adrenal [22] have been performed for the same reasons.
Surgical removal has been achieved by means of open surgery, laparoscopy and the DaVinci robotic system. When faced with larger cystic lesions authors opted for the open approach [8,9,18,24]. The inability to exclude pancreatic or adrenal origin was the reason why the authors settle for the open approach [22]. The laparoscopic approach has been the most favored owing to the usual advantages of laparoscopy plus the high success rate in treatment of mesenteric cystic lesions [6,7,13,19,23,26,27,30]. Li et al. performed laparoscopic removal of a calcified pseudocyst through a retroperitoneal approach. Inadvertent puncture with content spillage occurred in two instances of laparoscopic removal. Calvar et al. decided for fluid aspiration through a Veress needle for safer removal. Chandradevan et al. discuss the potential advantages of a robot over open and laparoscopic removal, but also note that further data are needed to determine statistical significance.
Conservative management was attempted in one case and ceased due to symptom progression [9]. It is unknown to this date whether the watch and wait approach is feasible for the patient who remains symptom free.
|
Radiologic characteristic |
Author |
|
Displacing/compressing parenchyma and vascular structures |
Rosado13, Falidas3, Olakowski22, Mickovic4, Palanivelu23, Abedini18 |
|
Distinct margins |
Iida10, Olakowski22, Park16, Uchiyama5, Calvar19, Yamabuki6, Karim25, Latif26 |
|
Perfectly round shape |
Mickovic4 |
|
Uneven shape |
Falidas3 |
|
Thin wall |
Rosado13, Gallego17, Mickovic4, Prabhu24, Serena9, Uchiyama5 |
|
Thick wall |
Abedini18 |
|
Unenhanced wall |
Latif26, Lee15 |
|
Peripheral calcifications egg-shell like or partial |
Gallego17, Palanivelu23, Mickovic4, Latif26 |
|
Unilocular |
Serena9, Abedini18, Calvar19, Karim25 |
|
Multilocular |
Falidas3, Iida10, Park16 |
|
Homogeneous contents (-22 up to 14 HU) |
Olakowski22, Abedini18, Serena9 |
|
Heterogeneous contents sometimes as fluid-fluid level |
Mickovic4, Park16, Yamabuki6, Gallego17, Liao29 |
|
Peritoneal effusion |
Sabounji8, Serena9 |
Table 1: Combined radiologic characteristics from US and CT
Conclusions
Accurate preoperative characterization of mesenteric cystic lesions remains challenging. Presence of intraabdomial cystic lesion in a patient with positive history for abdominal trauma should raise the suspicion for a traumatic mesenteric pseudocyst. Total surgical excision of the nonpancreatic pseudocyst has been the treatment of choice. It remains unclear to this date whether other treatment approaches are feasible. Due to the rarity of mesenteric pseudocyst, designating a prospective study would include the effort and coordination of many surgical centers in the world. Because this is rather difficult, a more standardized style of reporting these cases would facilitate higher quality literature reviews in the future.
Acknowledgements
Funding not received
Conflicts of interest
None
References
- De Perrot M, Bründler M, Tötsch M, et al. Mesenteric cysts. Toward less confusion? Dig Surg. 17 (2000): 323-328.
- Chandradevan R, Rutkofsky I, Sirju K, et al. "Look Before You Leap": Robotic Resection of a Jejunal Mesenteric Pseudocyst. Cureus 11 (2019): e4750.
- Falidas E, Mathioulakis S, Vlachos K, et al. Traumatic mesenteric cyst after blunt abdominal trauma. Int J Surg Case Rep 2 (2011): 159-62.
- Mickovic S, Bezmarevic M, Nikolic-Mickovic I, et al. Traumatic mesenteric pseudocyst. Vojnosanit Pregl. 71 (2014): 685-688.
- Uchiyama S, Suzuki T, Imai S, et al. Time-course ultrasonographic observation of a mesenteric pseudocyst of the sigmoid colon: report of a case. Surg Today 27 (1997): 257-260
- Yamabuki T, Suzuoki M, Murakami T, et al. Laparoscopic Resection of a Jejunal Mesenteric Pseudocyst. Case Rep Gastroenterol 11 (2017): 526-530.
- Kurnicki J, Swiatkiewicz J, Wrzesinska N, et al. Laparoscopic treatment of a huge mesenteric pseudocyst - case report. Wideochir Inne Tech Maloinwazyjne 6 (2011): 167-172
- Sabounji SM, Fall M, Gueye D, et al. Acute appendicitis revealing a giant mesenteric pseudocyst: case report. Pan Afr Med J 41 (2022): 178.
- Serena T, Gao R, Dinnan K. Open surgical approach for infected mesenteric pseudocyst presenting as lifelong, migratory abdominal pain-A case report. Int J Surg Case Rep 66 (2020): 96-100.
- Iida T, Suenaga M, Takeuchi Y, et al. Mesenteric pseudocyst of the sigmoid colon. J Gastroenterol 38 (2003): 1081-1085.
- Bolívar-Rodríguez MA, Cazarez-Aguilar MA, Luna-Madrid EE, et al. Pseudoquiste mesentérico infectado en yeyuno: reporte de un caso [Infected jejunal mesenteric pseudocyst: A case report]. Cir Cir 83 (2015): 334-338.
- Fan HL, Chen TW, Hong ZJ, et al. Volvulus of small intestine: rare complication of mesenteric pseudocyst. Z Gastroenterol 47 (2009): 1208-1210.
- Rosado CRB, Machado DS, De Magalhães Esteves J, et al. A Case of Mesenteric Pseudocyst Causing Massive Abdominal Swelling. Eur J Case Rep Intern Med 3 (2016): 000364.
- Bhullar JS, Orfanou P. The disappearing abdominal mass: mesenteric pseudocyst. JSLS 18 (2014): 319-322.
- Lee SE, Choi IS, Choi WJ, et al. Mesenteric pseudocyst of the small bowel in gastric cancer patient: a case report. J Gastric Cancer 12 (2012): 43-45.
- Park SE, Jeon TJ, Park JY. Mesenteric pseudocyst of the transverse colon: unusual presentation of more common pathology. BMJ Case Rep 15 (2014): bcr2013202682.
- Gallego JC, González JM, Fernández-Virgós A, et al. Retrorectal mesenteric cyst (non-pancreatic pseudocyst) in adult. Eur J Radiol 23 (1996): 135-137.
- Abedini L, Hosseinpour R, Mehrabi S, et al. An asymptomatic huge primary retroperitoneal pseudocyst: a case report and review of the literature. BMC Surg 22 (2022): 58.
- Calvar LA, Jiménez LR, Fdez-Pello Montes S, et al. Non-pancreatic Pseudocyst Presenting as a Giant Retroperitoneal Mass. Arch Esp Urol 75 (2022): 472-475.
- Li ZL, Li HL, Chen HW, et al. An egg shell-like retroperitoneal pseudocyst. Urology 78 (2011): 561-562.
- Ng JW, Ng HK. Retroperitoneal pseudocyst: an explanation. Pediatr Surg Int 11 (1996): 435-436.
- Olakowski M, Ciosek J. Giant pseudocyst of the retroperitoneal space mimicking a lesion arising from the left adrenal gland. Endokrynol Pol 73 (2022): 790-791.
- Palanivelu C, Rangarajan M, Senthilkumar R, et al. Laparoscopic excision of an infected "egg-shelled" retroperitoneal pseudocyst. J Gastrointestin Liver Dis 17 (2008): 465-8.
- Prabhu R, Rodrigues G, Sarma YS, et al. Non-pancreatic retroperitoneal pseudocyst: a benign disease with non-specific symptoms. BMJ Case Rep 2 (2013): bcr2013200184.
- Karim L, Larkin D, Sadat M. Examine the patient not the hernia: identification of an asymptomatic giant primary retroperitoneal pseudocyst. A case report and literature review. J Surg Case Rep 17 (2016): rjw092.
- Latif E, Musthafa S, Ahmed A, et al. Idiopathic Retroperitoneal Non-pancreatic Pseudocyst in an Adult Male: Radiological Images and Surgical Video of Laparoscopic Excision. Cureus 12 (2020): e7243.
- Farag M, Gyomber D, Norden S. Primary retroperitoneal pseudocyst: beware of the hoax solid enhancing adrenal mass. BMJ Case Rep 12 (2019): e232852.
- Tsukada O, Kawabe K. A case of retroperitoneal pseudocyst filled with necrotic material. Nihon Hinyokika Gakkai Zasshi 69 (1978): 1667-1670.
- Liao WI, Lin YY, Ko KH, et al. Midgut volvulus as a delayed consequence of posttraumatic mesenteric pseudocyst. Am J Emerg Med 27 (2009): 1025-1026.
- Resta G, Tartarini D, Fabbri N, et al. Laparoscopic resection of a jejunal mesenteric pseudocyst: case report. G Chir 35 (2014): 279-282.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 