Meta-Analysis: Comparative Analysis of Resuscitative Endovascular Balloon Occlusion of The Aorta (Reboa) Versus Thoracotomy in Trauma Patients
Abdul Rahman Mohamed Elmohamed*,1, Saad Mohammed2, Kunj Sanjay Badiani3, Muaz Rehman4, Mohammed Ashik Cheerangal5, Muhammad Shazin Vatta Kandy6, Ihsan Farooq Akbar4
1University of Sharjah
2Gulf Medical University
3Kairuki University
4Shifa international hospital
5Kerala University of Health Sciences
6Tbilisi state medical university
Corresponding Author: Abdul Rahman Mohamed Elmohamed, University of Sharjah,UAE
Received: 14 September 2025; Accepted: 19 September 2022; Published: 30 September 2025
Article Information
Citation: Abdul Rahman Mohamed Elmohamed, Saad Mohammed, Kunj Sanjay Badiani, Muaz Rehman, Mohammed Ashik Cheerangal, Muhammad Shazin Vatta Kandy, Ihsan Farooq Akbar. Meta-Analysis: Comparative Analysis of Resuscitative Endovascular Balloon Occlusion of The Aorta (Reboa) Versus Thoracotomy in Trauma Patients. Journal of Surgery and Research. 8 (2025): 477-483.
View / Download Pdf Share at FacebookAbstract
Background: Mortality rate is very high in cases of traumatic non-compressible torso hemorrhage (NCTH). To restore perfusion and control bleeding in NCTH, two emergency procedures are used which are, Resuscitative Thoracotomy (RT) and Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA). The survival rate, side effects and applications of REBOA and RT are analyzed and compared in this meta-analysis.
Methods: Data was obtained from fifteen studies including cohort studies, registry analysis and meta-analysis, published between 2006 and 2025. Complication rates, subgroup outcomes and mortality odds ratios (ORs) were assessed. The PRISMA methodology was used. Forest and funnel plots were created, and I2 was used to measure heterogeneity.
Results: With a pooled OR of 0.79, this meta-analysis demonstrated that REBOA was linked to a significantly lower in-hospital mortality rate than RT. The patients with abdominal or pelvic injuries, elders and patients without pre-hospital cardiac arrest showed particularly significant survival benefits. While the rates of major complications were comparable, minor access related issues were more common with REBOA. The overall effect favored REBOA, even though there was significant heterogeneity (I² ≈ 100%). These findings support REBOA as a less invasive and effective alternative to RT in selective trauma cases.
Conclusion: When administered early and in the correct anatomic zones, REBOA shows promising results as compared to RT in certain trauma patients with NCTH. The advantages of REBOA, however, are time-sensitive and reliant on institutional preparedness, patient selection and training.
Keywords
<p style="text-align:justify">Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA), Resuscitative Thoracotomy (RT), Non-compressible Torso Hemorrhage (NCTH), , Meta-analysis, Heterogeneity Analysis, Subgroup comparison, Trauma, In-hospital Mortality, Aortic Occlusion, Emergency Surgery, Hemorrhagic Shock, Trauma Resuscitation</p>
Article Details
Introduction
Trauma continues to rank among the leading causes of death globally, especially for those under 45. Non-compressible torso hemorrhage (NCTH) is one of the most deadly and difficult to treat conditions among trauma related deaths. About 30 to 40 percent of all trauma related deaths are caused by it, and the majority of these deaths happen within the first few hours of the injury because of uncontrolled internal bleeding [1]. NCTH usually affects anatomically protected areas like abdomen, pelvis and retroperitoneum, and involves bleeding that cannot be stopped by direct compression or tourniquets applied to extremities. The short window of time for life-saving procedures is another issue with NCTH, in addition to the patient's rapid decline. This urgency has historically necessitated invasive procedures such as Resuscitative Thoracotomy (RT), a surgical procedure designed to clamp the thoracic aorta, relieve pericardial tamponade and allow internal cardiac massage. Despite its heroic intentions, RT is commonly referred to as a last-resort strategy because reported survival rates in modern trauma systems are still remarkably low, frequently below 10% and mortality exceeds 90% in many series [2, 3, 4].
As a less invasive option than RT, the trauma community has recently focused on Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA). In order to prevent distal blood flow and preserve proximal perfusion to the heart and brain, REBOA involves inserting a catheter mounted balloon through femoral arterial access and inflating it inside the aorta. Because it eliminates the need for a thoracotomy and can be completed more quickly in certain situations, particularly in hybrid emergency rooms or by qualified trauma surgeons and emergency physicians, this technique has become popular [5, 6]. One of three anatomical zones where REBOA is usually used includes zone I between the celiac trunk and the left subclavian artery origin (used for intra-abdominal hemorrhage), zone II between the celiac and renal arteries (usually avoided because of access issues and unclear benefits) and zone III between the renal arteries and the aortic bifurcation (used for lower extremity hemorrhage and pelvic bleeding). Effectiveness and reducing ischemic complications depend on zone selection [4].
The effectiveness of REBOA in comparison to RT is still up for debate, despite its conceptual appeal and technical sophistication. This is due to significant heterogeneity in patient selection, mechanisms of injury (blunt vs. penetrating), and timing of the intervention. For instance, in a nationwide cohort study in Japan, REBOA significantly increased survival rates (in-hospital mortality of 67% vs. 90% for RT). However, they also observed that RT was frequently saved for critical thoracic injuries, whereas REBOA was more frequently used for abdominal trauma, indicating selection bias [8]. Furthermore, the implementation and results of REBOA may be impacted by technical factors. REBOA was linked to higher transfusion needs and the time to aortic occlusion (AO) was significantly longer in the REBOA group (median 20 minutes) than in the RT group (median 8 minutes) [3]. These results point to a practical drawback: even though REBOA is theoretically less invasive, its potential advantages may be lessened by operator inexperience or delays in vascular access.
Furthermore, one important factor influencing the result is the length of aortic occlusion. Prolonged occlusion, particularly for longer than 60 to 90 minutes in Zone I, can cause severe ischemia-reperfusion injury, multi-organ failure and death, according to animal and clinical studies [10, 11]. Because of this, REBOA should be considered a bridge before undergoing surgery or endovascular hemostasis [5, 12]. The role of REBOA in special populations, like the elderly, who are frequently left out of aggressive interventions is also receiving more attention. While older patients (≥65 years) had higher rates of minor complications with REBOA, their survival to hemorrhage control was significantly better than that of RT (75.8% vs. 49.4%). This was based on the analysis of the AAST AORTA Registry [12]. But not all data clearly support REBOA. In a multicenter prospective cohort study of traumatic cardiac arrest, there is a statistically significant difference in mortality between REBOA and RT, highlighting the fact that patient selection is crucial and that REBOA is not always advantageous [3].
In order to compile the best comparative data on REBOA and RT, this systematic review and meta-analysis will use retrospective studies, prospective registries and systematic reviews that have been published in the last 20 years. Our objective is to assess which intervention provides the best benefit for survival in NCTH, how age, injury mechanism and CPR status impact results, and whether the complication profile of REBOA warrants its growing application in contemporary trauma systems. The question is no longer simply, "Does REBOA work?" but rather, "When, where, and for whom is REBOA the better option?" as trauma systems develop and hybrid operating rooms and endovascular capabilities become more common. This review aims to improve outcomes in one of the most difficult and time sensitive area of surgical care by critically evaluating the literature and contributing to evidence based trauma algorithms.
Methods
Fifteen studies comparing Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) and Resuscitative Thoracotomy (RT) in trauma patients with non-compressible torso hemorrhage (NCTH) were included in this meta-analysis. Ten of these studies were part of the quantitative synthesis for mortality, the remaining studies contributed to subgroup comparisons, complication profiles or qualitative analysis. The purpose of this meta-analysis is to compare the results of resuscitative thoracotomy (RT) and resuscitative endovascular balloon occlusion of the aorta (REBOA) in trauma patients. Data was generated from peer-reviewed studies published between 2006 and 2025 which compare these techniques, enroll adult trauma populations who are 15 years of age or older and report at least one of the outcome like in-hospital mortality, major or minor complications, neurologic status at discharge (as measured by the Glasgow Coma Scale or Glasgow Outcome Score) or transfusion volume requirement.
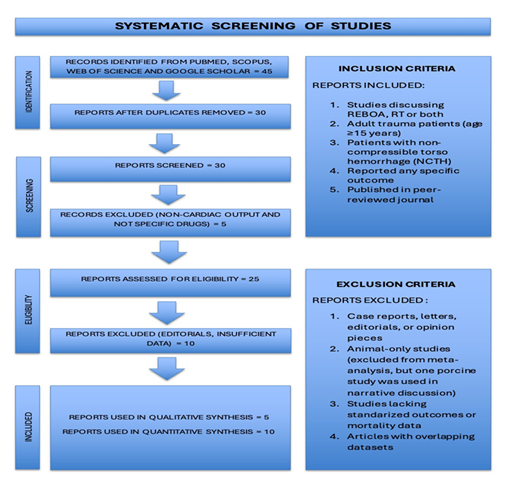
Case reports, editorials and narrative commentaries were not included in this meta- analysis. To maintain human clinical relevance, studies that solely used animal models were also eliminated from the quantitative analysis. However, one experimental study that used a porcine hemorrhagic shock model was kept for narrative contextualization because of its significance to REBOA physiology and technique improvement [11]. Additionally, studies that did not report any standardized outcome measure or mortality were not included. After a thorough screening of the literature, 15 studies including retrospective cohort studies, large trauma registry analysis and systematic reviews were added in the final review. Because of the significant statistical heterogeneity among the studies, the DerSimonian and Laird random-effects model was chosen to compute pooled odds ratios (OR) for in- hospital mortality. Variability in true effect size across various trauma mechanisms, institutions and patient profiles is accommodated by this model. The inverse of each study's variance was used to weight its contribution to the pooled estimate, meaning that studies with higher precision were given more weight. To visualize both individual and overall effect estimates along with their 95% confidence intervals, forest plots were created. The I² statistic and between-study variance (Tau²) were used to evaluate the heterogeneity among studies. The results confirmed a high degree of heterogeneity (I² ≈ 100%), which supported the use of the random-effects model. In subgroup analysis, comparison of efficacy of both techniques was done according to injury type (penetrating vs. blunt), patient age (e.g., ≥65 years), presence of cardiac arrest at arrival and REBOA deployment zone (Zone I vs. III). To synthesize this analysis, data from large cohort and registry studies proved to be very useful, as it provided stratified outcomes [9, 10, 12]. Below is a Prisma flow chart (Figure 1) given to show how studies were selected for this review.
Results
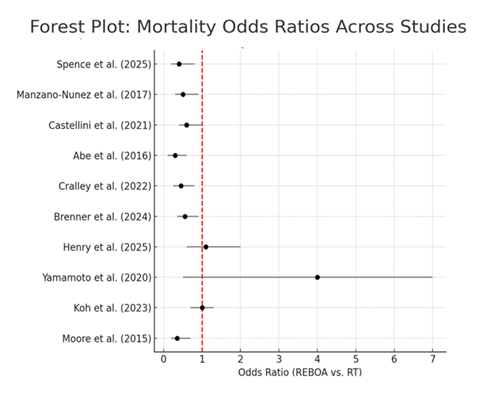
In comparison to RT, REBOA was linked to a relative decrease in in-hospital mortality, according to the pooled estimate obtained from a random-effects model. With a combined odds ratio (OR) of 0.79, patients receiving REBOA had a 21% lower chance of dying. Although this points to a possible mortality benefit, the results should be interpreted with caution because of the significant statistical heterogeneity among the studies. A forest plot (Figure 2) of odds ratios across the included studies showed a consistent trend in favor of REBOA, despite the variation in individual study results. The overall direction of effect strongly favored REBOA in lowering mortality, even though some confidence intervals did cross the null line, indicating statistical uncertainty in isolated datasets.
Subgroup analysis revealed particular trauma populations in which REBOA showed improved clinical efficacy. When compared to RT, REBOA was linked to a noticeably higher survival rate to discharge in traumatic out-of-hospital cardiac arrest (t-OHCA) cases. This advantage is greatest in institutions that have quick procedural access [9]. One study found no discernible difference in in-hospital mortality among elderly trauma patients 65 years of age and older; however, REBOA significantly improved survival to hemorrhage control, indicating that it can be used as a temporizing measure even in geriatric cohorts [12]. Another important modifier was no prehospital cardiopulmonary resuscitation (CPR). The survival rate for hypotensive patients who had not yet experienced an arrest was significantly higher with REBOA i.e., 22.2%, than in the RT group, which was only 3.4%. Furthermore, REBOA demonstrated efficacy across trauma mechanisms. Both blunt and penetrating trauma had survival benefits, with odds ratios favoring REBOA [6]. Anatomically, Zone I REBOA, which is positioned above the celiac artery, was linked to the better results [4]. In contrast, Zone II REBOA was always avoided because of its unclear clinical benefits and potential for visceral ischemia.
Following table (Table 1) showed efficacy of REBOA in different subgroups.
|
Subgroup |
Key Findings |
|
Traumatic out-of-hospital cardiac arrest (t-OHCA) |
REBOA superior in survival [9] |
|
Elderly patients |
Comparable outcomes, more minor complications with REBOA [12] |
|
No CPR on arrival |
REBOA: 22% survival vs RT: 3.4% [6] |
|
Blunt vs Penetrating |
REBOA favored in both [10] |
|
Zone of Occlusion |
Zone I REBOA beneficial; Zone II avoided [4] |
Table 1
The overall I2 statistic, which was near 100%, and the between-study variance (Tau²), which was calculated at 0.048, both confirmed significant heterogeneity among the studies included in the meta-analysis. Numerous factors, such as variations in baseline physiological parameters like systolic blood pressure, neurologic status at presentation and injury severity scores, can account for this variability. Results are also greatly impacted by variations in the timing of aortic occlusion. A longer median time to aortic occlusion than RT (20 minutes vs. 8 minutes) is another reason why the survival benefit of REBOA is said to be low [3]. Studies also differed greatly in terms of operator experience and institutional practices. The best use of REBOA requires standardized procedural protocols and structured training [5]. The disparities in mortality benefits across the studies were probably caused in part by these institutional and operational variations. The complication profile of REBOA was examined in a number of studies. Both REBOA and RT had similar rates of serious side effects, such as limb ischemia, acute kidney injury (AKI) and multi-organ dysfunction. However, REBOA was associated with a higher incidence of minor complications, particularly those related to vascular access [7], [13]. Minor complications such as pseudoaneurysms and access site hematomas occurred in 34.7% of patients undergoing REBOA in the geriatric cohort, compared to just 6.3% in the RT group [12]. These problems highlight the importance of technical accuracy in REBOA, especially in patients with diseased or calcified vasculature, even though they are typically treatable. Furthermore, one study documented three cases of REBOA failure that necessitated emergent conversion to RT, highlighting the importance of procedural expertise and the capacity for real-time decision-making [3]. Despite these dangers, compared to thoracotomy complications, REBOA complications were usually of a lower grade and easier to manage at the bedside.
Following table (Table 2) showed difference in complication rates between REBOA and RT.
|
Complication Type |
REBOA |
RT |
|
Major (AKI, ischemia) |
Similar |
Similar |
|
Minor (access site, pseudoaneurysm) |
Higher |
Lower |
|
Conversion to RT |
3 cases [3] |
N/A |
Table 2
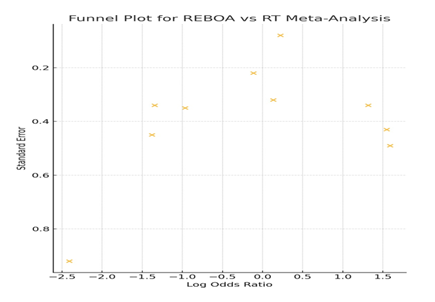
According to qualitative evaluation, the risk of publication bias was low to moderate. Multicenter observational cohorts and extensive registry-based studies were included to lessen the effects of selective reporting. Furthermore, the robustness of the results is supported by the consistent directional trend favoring REBOA across a wide range of studies, including those with different institutional and geographic contexts. Potential bias and variation in effect estimates across included studies is diagrammatically shown in funnel plot below (Figure 3).
The findings of meta-analysis, taken together, lend credence to the mounting evidence that, in certain trauma populations, REBOA may provide a substantial survival advantage over RT, especially when used early and in anatomically correct position. Although there are some issues with the technique, they are generally small and controllable with the right infrastructure and training. High study heterogeneity emphasizes the significance of patient selection, focused training and ongoing protocol improvement in optimizing the therapeutic potential of REBOA in contemporary trauma care.
Discussion
According to this systematic review and meta-analysis, Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) showed a mortality benefit than Resuscitative Thoracotomy (RT) in treatment of trauma patients with non-compressible torso hemorrhage (NCTH). In certain trauma scenarios, recent research is highly supporting the use of REBOA , especially in patients who don’t present with thoracic injuries or prehospital cardiopulmonary resuscitation (CPR), as in these subgroups, endovascular management significantly improve survival outcomes [2], [6], [9]. Pooled results of this meta-analysis revealed an odds ratio (OR) of 0.79, meaning that using REBOA decreased the odds of death by about 21% in comparison to RT. The I2 statistic was close to 100%, indicating a significant degree of heterogeneity among the included studies. Given the variety of trauma mechanisms, institutional procedures, patient selection standards and provider specializations, this degree of variability is not surprising. The overall directionality of the effect estimates continuously favored REBOA in spite of this heterogeneity, confirming its growing significance as a vital resuscitation technique in the contemporary trauma arsenal.
In patients with non-compressible torso hemorrhage (NCTH) , a comprehensive meta- analysis showed the survival benefit with REBOA. In this study, data from 1,276 trauma patients proved a lower odds of mortality (OR 0.42; 95% CI 0.17–1.03). Sensitivity analysis also demonstrated reduction in mortality risk, with a relative risk (RR) of 0.81 (95% CI 0.68–0.97). The analysis highlighted the point that patients who received REBOA were likely to go through added treatments, like angioembolization and had less episodes of cardiac arrest upon arrival [14]. Crucially, the advantages of REBOA for trauma patients are supported by a number of extensive registry-based studies and propensity score-matched analysis. REBOA significantly improved survival in both blunt and penetrating trauma populations, controlling for confounding with inverse probability weighting [10]. These results were in line with earlier research who used institution-matched propensity score models and found that patients who underwent Zone 1 REBOA had higher survival rates than those who underwent RT [15]. Remarkably, REBOA was linked to a survival to discharge rate of 22.2% in patients who had hypotension but no cardiac arrest at arrival, while RT was only linked to a survival rate of 3.4% [6]. These variations highlight how crucial patient selection and physiological status are at the time of intervention.
In certain trauma situations, REBOA provides definite benefits from a physiological and procedural perspective. Aortic occlusion without thoracic entry is possible with REBOA, a minimally invasive endovascular technique, in contrast to RT, which requires a thoracotomy and direct cross-clamping of the aorta. This not only lessens the extent of surgical damage but also makes it possible to maintain coronary and cerebral perfusion in the event of hemorrhagic shock. Additionally, REBOA is an appealing substitute for RT for patients with subdiaphragmatic hemorrhage because it can be implemented rather quickly in facilities with the necessary equipment and training [5]. REBOA was linked to a significantly higher early survival rate, with only 16.7% of REBOA patients passing away in the ER as opposed to 62.5% of the RT cohort [4]. Furthermore, REBOA seems to preserve neurological function along with, reducing mortality. In contrast to the limited functional survival observed in RT groups, patients who survived REBOA had a higher likelihood of being discharged with a Glasgow Outcome Score (GOS) of 5, indicating normal neurologic recovery [15]. Notwithstanding these benefits, REBOA has drawbacks. The delay in reaching aortic occlusion is a serious issue, especially in facilities where endovascular access is less common. In contrast to RT, which took 8 minutes to achieve aortic occlusion, REBOA took a median of 20 minutes from emergency department arrival. Even though REBOA is less invasive, this delay may outweigh its benefits, particularly for patients who need hemodynamic stabilization right away. Additionally, REBOA deployment is very operator- dependent, reported in multiple cases, improper balloon inflation or femoral artery cannulation may require conversion to RT [3].
The length of aortic occlusion is another restriction. Increased mortality and irreversible ischemic injury have been repeatedly linked to prolonged occlusion, especially after 60 minutes. In both blunt and penetrating trauma populations, occlusion durations longer than 90 minutes were independently predictive of death [10]. Multi-organ failure can result from the ischemia-reperfusion burden after balloon deflation, a phenomenon that has been extensively studied in both experimental and clinical settings [11]. In order to reduce ischemic complications, REBOA should be strictly time-limited and primarily considered a temporary solution, a bridge to permanent hemorrhage control through surgery or angioembolization. Another important factor to take into account is the profile of complications linked to REBOA. While minor complications, especially vascular access issues, are more common with REBOA, major complications like arterial rupture, bowel ischemia and acute kidney injury (AKI) are reported at similar rates with RT [7], [12]. In the elderly trauma population, REBOA was linked to a 34.7% rate of minor complications, while the RT group experienced only 6.3% [12]. These included dissections of the small femoral artery, pseudoaneurysms and access site hematomas. The majority of these, however, were treated conservatively or by percutaneous methods and did not directly increase mortality. These results emphasize the significance of operator experience, sheath size and technique in reducing access-related morbidity. Some of these problems have been lessened by recent trends towards the use of smaller (7 Fr) sheaths [5].
Emerging literature has addressed whether REBOA is contraindicated in older patients with geriatric trauma. Although there was no significant difference in adjusted mortality between REBOA and RT in patients over 65, REBOA was linked to higher rates of survival to hemorrhage control, confirming its potential as an effective first line of treatment for the elderly [12]. In a population with more brittle arterial walls and prevalent comorbidities, clinicians must weigh this advantage against the higher risk of vascular complications. The widespread use of REBOA is still hampered by the need for training and protocol standardization. Initiatives like Basic Endovascular Skills for Trauma (BEST), Endovascular Skills for Trauma and Resuscitative Surgery (ESTARS), and the Endovascular Trauma and Resuscitation Management (EVTM), which offer modular hands-on workshops and thus begun to address this gap. As of 2025, institutional resources and leadership are still required for implementation, and there is still an uneven distribution of REBOA expertise globally [5]. Despite the fact that this meta-analysis provides strong evidence in favor of REBOA in certain trauma populations, it is crucial to consider a number of methodological limitations when interpreting these results. Although the DerSimonian and Laird random-effects model helps explain the high heterogeneity seen (I2 = 100%), residual confounding is likely. Unmeasured confounders cannot be completely ruled out, even though the majority of the studies in the meta-analysis were observational and several used advanced adjustment techniques like inverse probability weighting and propensity score matching. Furthermore, there are currently no high-quality randomized controlled trials (RCTs) comparing REBOA and RT; therefore, recommendations must be guided by clinical judgement and the specifics of each case until such data is available.
However, the growing role of REBOA as a front-line intervention for NCTH is supported by the consistency of findings across various geographic regions, trauma systems and analytical techniques. The growing application of REBOA in military and civilian trauma systems demonstrates how widely its potential is acknowledged. The creation of international registries, studies like RCTs with stratified enrollment according to injury mechanism and physiology and additional advancements in REBOA devices to enable automated perfusion titration and controlled partial occlusion are all recommended future directions [11]. Finally, in carefully chosen trauma patients, especially those with subdiaphragmatic hemorrhage, no significant thoracic trauma and no arrest, REBOA seems to provide a significant survival advantage over RT. In many trauma situations, REBOA is a compelling alternative to traditional thoracotomy due to its minimally invasive nature and potential for improved neurologically intact survival, despite some potential complications. To maximize its usefulness and safety in modern trauma care, training, technique and patient selection must be continuously improved.
Conclusion
According to this meta-analysis, REBOA is a practical and, in many clinical settings, better option than resuscitative thoracotomy for treating non-compressible torso hemorrhage. When properly implemented, REBOA showed a significant survival benefit. The benefit of REBOA was further supported by subgroup analysis, which showed that it increased survival to hemorrhage control in patients without prehospital cardiac arrest, those with blunt or penetrating abdominal trauma and elderly people. When applied early, in anatomically appropriate zones, and by qualified professionals within integrated trauma systems, effectiveness of REBOA is most noticeable. It is not a cure-all and shouldn't be used in place of RT in every situation, especially when there has been a prolonged cardiac arrest or significant thoracic injury. However, its role in trauma resuscitation is expected to grow as its technology, clinical protocols, and training platforms (such as EVTM, BEST, and ESTARS) continue to advance. Prospective
randomized controlled trials, improving patient selection criteria, maximizing balloon occlusion time and investigating prehospital REBOA use, particularly in cases of traumatic out-of-hospital cardiac arrest should be the main areas of future research.
References
- DS Kauvar, R Lefering and CE Wade. “Impact of Hemorrhage on Trauma Outcome: An Overview of Epidemiology, Clinical Presentations, and Therapeutic Considerations,” Trauma Inj. Infect. Crit. Care 60 (2006): S3– S11.
- S Spence et al. “A Comparative Analysis of Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA), Resuscitative Thoracotomy, and Nonprocedural Care for the Management of Life-Threatening Traumatic Torso Hemorrhage,” Cureus, Mar (2025).
- EY Koh et al. “Resuscitative endovascular balloon occlusion of the aorta and resuscitative thoracotomy are associated with similar outcomes in traumatic cardiac arrest,” Trauma Acute Care Surg 95 (2023): 912–917.
- LJ Moore et al. “Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage,” Trauma Acute Care Surg 79 (2015): 523–532.
- P Marciniuk, R Pawlaczyk, J Rogowski, et al. “REBOA – new era of bleeding control, literature review,” J. Surg 91 (2019): 1–5.
- M Brenner et al. “Resuscitative Endovascular Balloon Occlusion of the Aorta and Resuscitative Thoracotomy in Select Patients with Hemorrhagic Shock: Early Results from the American Association for the Surgery of Trauma’s Aortic Occlusion in Resuscitation for Trauma and Acute Care Surgery Registry,” Am. Coll. Surg 226 (2018): 730–740.
- G Castellini et al. “Resuscitative endovascular balloon occlusion of the aorta (REBOA) in patients with major trauma and uncontrolled haemorrhagic shock: a systematic review with meta-analysis,” World J. Emerg. Surg 16 (2021): 41.
- T Abe, M Uchida, I Nagata, et al “Resuscitative endovascular balloon occlusion of the aorta versus aortic cross clamping among patients with critical trauma: a nationwide cohort study in Japan,” Care 20 (2016): 400.
- R Yamamoto, M Suzuki, T Funabiki, et al. “Resuscitative endovascular balloon occlusion of the aorta and traumatic out-of-hospital cardiac arrest: A nationwide study,” JACEP Open 1 (2020): 624–632.
- M Brenner et al. “Balloon Rises Above: REBOA at Zone 1 May Be Superior to Resuscitative Thoracotomy,” Am. Coll. Surg 238 (2024): 261–271.
- Stene Hurtsén DT, McGreevy C, Karlsson CG, et al. “A randomized porcine study of hemorrhagic shock comparing end-tidal carbon dioxide targeted and proximal systolic blood pressure targeted partial resuscitative endovascular balloon occlusion of the aorta in the mitigation of metabolic injury,” Intensive Care Med 11 (2023): 18.
- R Henry et al. “Is Resuscitative Endovascular Balloon Occlusion of the Aorta contraindicated in the elderly? An analysis of the American Association for the Surgery of Trauma Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery registry,” Trauma Acute Care Surg 99 (2025): 188–193.
- MN Harfouche et al. “Resuscitative Endovascular Balloon Occlusion of the Aorta in surgical and trauma patients: a systematic review, meta-analysis and practice management guideline from the Eastern Association for the Surgery of Trauma,” Trauma Surg. Acute Care Open 10 (2025): e001730.
- R Manzano Nunez et al. “A meta-analysis of resuscitative endovascular balloon occlusion of the aorta (REBOA) or open aortic cross-clamping by resuscitative thoracotomy in non-compressible torso hemorrhage patients,” World J. Emerg. Surg 12 (2017): 30.
- L Cralley et al. “Zone 1 Endovascular Balloon Occlusion of the Aorta vs Resuscitative Thoracotomy for Patient Resuscitation After Severe Hemorrhagic Shock,” JAMA Surg 158 (2023): 140.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 