Missed Diagnosis: Infantile Hemangioma or Arteriovenous Malformation? Clinical Case
Safin Dinar*, Onlasynov Aziz, Amatov Daniiar
Bishkek Prime Heart Clinic, 720017, Kyrgyzstan
*Corresponding author: Safin Dinar, Bishkek Prime Heart Clinic, 720017, Kyrgyzstan
Received: 14 November 2023; Accepted: 22 November 2023; Published: 07 December 2023
Article Information
Citation: Safin Dinar, Onlasynov Aziz, Amatov Daniiar. Missed Diagnosis: Infantile Hemangioma or Arteriovenous Malformation? Clinical Case. Fortune Journal of Health Sciences. 6 (2023): 517-520
View / Download Pdf Share at FacebookAbstract
Infantile hemangioma (IH) is represented by proliferation of endothelium pathological vessels in infants. This tumor occurs in 5-10% of children of the first life. Frequent localization on the skin is the area of the head and neck. IH is characterized by certain periods: the period of growth, stabilization of growth and involution of tumor. External manifestations are quite typical and depend on the type of IH. For diagnosis, it is enough to take into account the data of anamnesis, clinical picture and sonography. However, due to the similarity of the external manifestations of vascular anomalies, erroneous diagnoses and incorrect treatment are possible. Arteriovenouse malformation (AVM) is one of the diseases with which it is necessary to carry out differential diagnosis. Unlike IH, AVM it requires more aggressive invasive treatment. The purpose of the publication is to present a clinical observation of a patient with an erroneous diagnosis of "infantile hemangioma".
Keywords
<p>Infantile hemangioma, arteriovenous malformation, vascular malformation, vascular tumor</p>
Article Details
1. Introduction
Infantile hemangioma (IH) is the most common benign vascular tumor in children under the age of 1 year [1]. According to various authors, the frequency of occurrence reaches 5-10% of the total number of vascular skin tumors [2, 3]. IH is characterized by certain successive periods of development: the growth period is an increase in the size of the tumor due to uncontrolled proliferation of pathological vessels of hemangioma, the period of growth stabilization when growth processes slow down and the period of involution is reverse lysis of tumor tissue and replacement of residues with fibrous–adipose tissue [4]. Depending on the depth of the skin lesion, the following types of IH: superficial (when IH located on the surface of the skin), deep (the tumor tissue is located in the thickness of subcutaneous fat, without skin manifestations), mixed (a combination of superficial and deep appearance) [5]. The correct diagnosis is based on the data of anamnesis and clinical manifestations. In most cases, IH is located in the head and neck area, the number of elements on the skin can vary from a single hemangioma to multiple (more than 100 formations – hemangomatosis) [6]. Clinical manifestations depend on the type of IH: the superficial appearance is represented by a rounded structure on the skin in the form of a red plaque rising slightly above the skin or in the form of multiple telangiectasias; deep hemangioma is represented by a blue-purple subcutaneous formation, warm on palpation; mixed hemangioma has both red skin elements, with expanded telangiectasias around, and subcutaneous a component deforming the tumor location area [7]. Ultrasound examination is used to visualize the subcutaneous components of IH and to assess the dynamics of the course of the pathological process [8]. With typical manifestations, the diagnosis of IH is simple and does not require additional diagnostic methods. In rare cases, it is possible to conduct an immunohistochemical study to verify the diagnosis, for this purpose the GLUT-1 marker produced by IH cells is used [9]. It should be taken into account that conducting this study requires a biopsy of the tumor tissue under general anesthesia.
2. Clinical case
A full-term boy from the first pregnancy, which proceeded without peculiarities. At birth, there was a red spot on the skin of the right cheek, local hyperthermia was noted on palpation (Fig. 1).
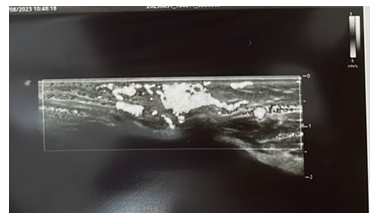
According to clinical manifestations, the child was diagnosed with "Infantile hemangioma of the right cheek" and at the age of 4 months was started local therapy with propranolol ointment. The duration of application of the ointment was 1.5 months, but the formation began to grow and bleed. In this regard, therapy with anaprilin 4 mg twice a day, a course of 4 months, was started. Against the background of therapy, the growth stopped, the swelling decreased, but the vascular spot did not go away. After a consultation at another medical clinic, it was decided to change therapy to atenolol and perform laser correction. The duration of taking atenolol was 14 months, 4 sessions of laser correction were performed, but without significant changes (Fig. 2). During ultrasound examination with color-doppler, two "feeding" vessels were revealed, the blood flow rate in arterial vessels was 20 cm / sec (Fig. 3).
On medical examination 6 months after the cancellation of atenolol, the formation did not change in size (Fig. 4), but palpation revealed pulsation in the area of the vascular spot, ultrasound with color-doppler revealed an arteriovenous fistula (Fig. 5). The found changes in the clinical picture made it possible to establish a clinical diagnosis of "Arteriovenous malformation, type 1".
3. Discussion
Vascular anomalies, especially IH, may have similar clinical manifestations, which complicates differential diagnosis and leads to wrong treatment. In most cases, to make a correct diagnosis, it is enough to take into account the data of anamnesis and clinical examination, ultrasound picture of the disease. To diagnose IH, it is necessary to take into account the change in the size and color of the formation – during the growth period there is an increase in size both in area and in depth, the color becomes more saturated, during involution the color fades, and the formation itself becomes flabby and gradually begins to decrease in size. With a large volume, local hyperthermia is possible due to active vascularization of tumor tissue. Ultrasound can determine a hypoechoic structure with a multitude of vessels with low resistance to blood flow in the growth phase, which becomes hyperechoic during the transition to the involution phase, with a gradual decrease in the number of vessels and a decrease in blood flow rate. IH is not characterized by the presence of pulsation in the area of the tumor location. Bleeding is also not a typical complication, it usually occurs during the active growth of the tumor, accompanied by the appearance of an ulcer on the surface of the hemangioma [10]. In the presented clinical observation, ultrasound monitoring was not carried out at the very beginning of the child's treatment, which currently does not allow to reliably determine the timing of the formation of an arteriovenous fistula and ultimately made it difficult to make a correct diagnosis. The appearance of bleeding after the use of local therapy also raises a number of questions, since there was no ulcer or any skin defect on the surface of the hemangioma. And finally, the lack of dynamics while taking beta-blockers should also have alerted doctors in terms of an incorrectly established diagnosis.
4. Conclusion
The presented clinical case demonstrates the complexity of differential diagnosis of vascular anomalies, which may have similar clinical manifestations. To make a correct diagnosis, it is necessary to take into account not only the anamnesis data, the clinical picture, but also to compare them with ultrasound data. In the presence of atypical manifestations that are not characteristic of the results of ultrasound, it is necessary to conduct an in-depth differential diagnosis, possibly with an immunohistochemical examination to confirm the diagnosis.
References
- Munden A, Butschek R, Tom WL, Marshall JS, Poeltler DM, Krohne SE, et al. Prospective study of infantile haemangiomas: incidence, clinical characteristics and association with placental anomalies. Br J Dermatol 170 (2014): 907-13.
- Sipkova Z, Xue K, Mudhar HS, Wagner B, Hildebrand GD. Early and Late Histological and Ultrastructural Findings in Resected Infantile Capillary Hemangiomas Following Treatment with Topical Beta-Blocker Timolol Maleate 0.5. Ocul Oncol Pathol 4 (2018): 100-106.
- Price A, Rai S, Mcleod RWJ, Birchall JC, Elhassan HA. Topical propranolol for infantile haemangiomas: a systematic review. J EurAcad Dermatol Venereol 32 (2018): 2083-2089.
- Haggstrom AN, Baselga E, Chamlin SL, Drolet BA, Garzon MC, Holland KE, et al. Localized infantile hemangiomas of the face and scalp: Predilection for the midline and periorbital and perioral skin. PediatrDermatol 35 (2018): 774-779.
- Barreau M., Dompmartin A. Hémangiomesinfantilescutanés. Archives de Pédiatrie 24 (2017): 592-596.
- Hamouda S, Soussan J, Haumonté JB, Bretelle F. In utero embolization for placental chorioangioma and neonatal multifocal hemangiomatosis. J GynecolObstet Hum Reprod 48 (2019): 689-694.
- Martin JM, Sanchez S, González V, Cordero P, Ramon D. Infantile hemangiomas with minimal or arrested growth: A retrospective case series. PediatrDermatol 36 (2019): 125-131.
- Weber FC, Greene AK, Adams DM, Liang MG, Alomari MH, Voss SD, et al. Role of imaging in the diagnosis of parotid infantile hemangiomas. Int J PediatrOtorhinolaryngol 102 (2017): 61-66.
- Brockman RM, Humphrey SR, Moe DC, North PE, King DM, Jensen JN, et al. Mimickers of Infantile Hemangiomas. Pediatr Dermatol 34 (2017): 331-336.
- Darrow DH, Greene AK, Mancini AJ, Nopper AJ; SECTION ON DERMATOLOGY, SECTION ON OTOLARYNGOLOGY–HEAD AND NECK SURGERY, and SECTION ON PLASTIC SURGERY. Diagnosis and Management of Infantile Hemangioma. Pediatrics 136 (2015): e1060-104.





 Impact Factor: * 6.2
Impact Factor: * 6.2 Acceptance Rate: 76.33%
Acceptance Rate: 76.33%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks