No Association Between Fever and Uninfected Hematoma in Postoperative Orthopedic Surgery and Traumatology
Ilke Ilgaz1, Joris Paccaud2, Blaise Wyssa2,3, Ilker Uçkay2,4*
1Medical Research Center, University of Geneva, Geneva, Switzerland
2Orthopaedic Surgery Service, Geneva University Hospitals, Geneva, Switzerland
3Général Beaulieu Hospital, Geneva, Switzerland
4Balgrist University Hospital, Zurich, Switzerland
*Corresponding Author: Ilker Uçkay, Balgrist University Hospital, Forchstrasse 340, 8008 Zurich/Switzerland
Received: 05 March 2019; Accepted: 18 March 2019; Published: 21 March 2019
Article Information
Citation: İlke Ilgaz, Joris Paccaud, Blaise Wyssa, İlker Uçkay. No Association Between Fever and Uninfected Hematoma in Postoperative Orthopedic Surgery and Traumatology. Journal of Surgery and Research 2 (2019): 20-25.
View / Download Pdf Share at FacebookAbstract
Objective: According to widespread belief or clinical experience, uninfected hematoma can cause fever. However, epidemiological data regarding this assumption are scant. We assess the epidemiology of hematoma and fever in the postoperative orthopedic context, in the context of surgical indications for revision surgery.
Methods: Single-center prospective observational study among adult orthopedic patients. All patients have anti-inflammatory medication and many have blood transfusions. Fever is defined as any axillary temperature ≥ 38°C (104°F), subfebrile temperatures as ≥ 37.2°C.
Results: Among 405 patients in the study, 164 had (40%) fever, 221 (55%) subfebrile temperatures, and 166 (41%) yielded visible hematomas. Overall, fever was not associated with hematoma (67/164 vs. 99/241; Pearson-χ², p=0.96). We equally found no association when analyzing only the subfebrile level (156/385 vs. 10/18; p=0.21) or when analyzing the temperatures only on Day 4 (p=0.95), Day 7 (p=1.00), or solely for cases requiring surgical re-intervention (4/10 vs. 6/9; Fisher-exact-test, p=0.37). As continuous variables, the maximum temperatures on each of the seven postoperative days were not higher for patients with hematoma (Wilcoxon-ranksum-tests; all p>0.10).
Conclusion: Within the time frame of one week postoperatively and real-life conditions, we failed to establish an epidemiological association between postoperative fever and the presence of hematoma in a large prospective observational study among adult orthopedic patients under anti-inflammatory drugs.
Keywords
Postoperative fever, Orthopedic surgery, Hematoma
Postoperative fever articles Postoperative fever Research articles Postoperative fever review articles Postoperative fever PubMed articles Postoperative fever PubMed Central articles Postoperative fever 2023 articles Postoperative fever 2024 articles Postoperative fever Scopus articles Postoperative fever impact factor journals Postoperative fever Scopus journals Postoperative fever PubMed journals Postoperative fever medical journals Postoperative fever free journals Postoperative fever best journals Postoperative fever top journals Postoperative fever free medical journals Postoperative fever famous journals Postoperative fever Google Scholar indexed journals Orthopedic surgery articles Orthopedic surgery Research articles Orthopedic surgery review articles Orthopedic surgery PubMed articles Orthopedic surgery PubMed Central articles Orthopedic surgery 2023 articles Orthopedic surgery 2024 articles Orthopedic surgery Scopus articles Orthopedic surgery impact factor journals Orthopedic surgery Scopus journals Orthopedic surgery PubMed journals Orthopedic surgery medical journals Orthopedic surgery free journals Orthopedic surgery best journals Orthopedic surgery top journals Orthopedic surgery free medical journals Orthopedic surgery famous journals Orthopedic surgery Google Scholar indexed journals Hematoma articles Hematoma Research articles Hematoma review articles Hematoma PubMed articles Hematoma PubMed Central articles Hematoma 2023 articles Hematoma 2024 articles Hematoma Scopus articles Hematoma impact factor journals Hematoma Scopus journals Hematoma PubMed journals Hematoma medical journals Hematoma free journals Hematoma best journals Hematoma top journals Hematoma free medical journals Hematoma famous journals Hematoma Google Scholar indexed journals Traumatology articles Traumatology Research articles Traumatology review articles Traumatology PubMed articles Traumatology PubMed Central articles Traumatology 2023 articles Traumatology 2024 articles Traumatology Scopus articles Traumatology impact factor journals Traumatology Scopus journals Traumatology PubMed journals Traumatology medical journals Traumatology free journals Traumatology best journals Traumatology top journals Traumatology free medical journals Traumatology famous journals Traumatology Google Scholar indexed journals blood transfusions articles blood transfusions Research articles blood transfusions review articles blood transfusions PubMed articles blood transfusions PubMed Central articles blood transfusions 2023 articles blood transfusions 2024 articles blood transfusions Scopus articles blood transfusions impact factor journals blood transfusions Scopus journals blood transfusions PubMed journals blood transfusions medical journals blood transfusions free journals blood transfusions best journals blood transfusions top journals blood transfusions free medical journals blood transfusions famous journals blood transfusions Google Scholar indexed journals Pyrogenic cytokines articles Pyrogenic cytokines Research articles Pyrogenic cytokines review articles Pyrogenic cytokines PubMed articles Pyrogenic cytokines PubMed Central articles Pyrogenic cytokines 2023 articles Pyrogenic cytokines 2024 articles Pyrogenic cytokines Scopus articles Pyrogenic cytokines impact factor journals Pyrogenic cytokines Scopus journals Pyrogenic cytokines PubMed journals Pyrogenic cytokines medical journals Pyrogenic cytokines free journals Pyrogenic cytokines best journals Pyrogenic cytokines top journals Pyrogenic cytokines free medical journals Pyrogenic cytokines famous journals Pyrogenic cytokines Google Scholar indexed journals tumor necrosis factors articles tumor necrosis factors Research articles tumor necrosis factors review articles tumor necrosis factors PubMed articles tumor necrosis factors PubMed Central articles tumor necrosis factors 2023 articles tumor necrosis factors 2024 articles tumor necrosis factors Scopus articles tumor necrosis factors impact factor journals tumor necrosis factors Scopus journals tumor necrosis factors PubMed journals tumor necrosis factors medical journals tumor necrosis factors free journals tumor necrosis factors best journals tumor necrosis factors top journals tumor necrosis factors free medical journals tumor necrosis factors famous journals tumor necrosis factors Google Scholar indexed journals phlebitis articles phlebitis Research articles phlebitis review articles phlebitis PubMed articles phlebitis PubMed Central articles phlebitis 2023 articles phlebitis 2024 articles phlebitis Scopus articles phlebitis impact factor journals phlebitis Scopus journals phlebitis PubMed journals phlebitis medical journals phlebitis free journals phlebitis best journals phlebitis top journals phlebitis free medical journals phlebitis famous journals phlebitis Google Scholar indexed journals
Article Details
1. Introduction
According to widespread belief or clinical experience, uninfected hematoma in orthopedic surgery can cause (resorption) fever. Pyrogenic cytokines such as interleukins or tumor necrosis factors have been described after traumatic conditions, even though there is no infection [1-3]. For example, author groups describe fever, even shaking chills [4, 5], after uninfected aortic dissection [5], embolisms, allergy, intracerebral hemorrhage [6, 7], rectus sheet hematoma [8], renal biopsy-related hematoma [9, 10], post-caesarian hematoma [11], or soft-tissue hematoma [12]. We do not doubt that in selected cases, postoperative fever is provoked by uninfected hematoma. However, epidemiological data linking surgical hematomas to fever are very scant. We advocate an investigation on this topic, because fever often leads to unnecessary antibiotic prescriptions, and invasive work-ups, for suspicion of postoperative infections [13]. Moreover, it is worth to investigate possible medical myths, let alone for academic reasons.
2. Methods
In 2011, we published a one-year’s prospective, observational study assessing postoperative fever [14] in the context of the epidemiology of postsurgical wound complications [13]. We now use this database to link postoperative temperature with the occurrence of hematoma (retrospective analysis of a prospectively assessed cohort). All patients have anti-inflammatory medication (mostly ibuprofen and paracetamol) and many have blood transfusions. We notified the occurrence of hematoma and daily temperatures for up to one week postoperatively and defined fever as any axillary temperature ≥ 38°C (104°F) and subfebrile temperatures as ≥ 37.2°C; independent of antipyretic medication. Exclusion criteria were: infection in the surgical site and/or remote (excluding infected hematomas), skin rash, malignant hyperthermia, thrombosis, phlebitis, withdrawal syndromes, allergy, atelectasis, pancreatitis, acute crystal-related inflammations such as gout, and incomplete data.
We performed a literature search using the English MeSH terms “hematoma”, “surgery” and “fever” in PubMed and internet. For group comparisons, we used the Pearson-χ², Fisher-exact or the Wilcoxon-ranksum-tests. Because of potential confounding, we added a multivariate logistic regression analysis with the outcome fever. P values ≤ 0.05 (two-tailed) were significant. We used STATA™ software (9.0, STATA Corp, College Station, USA).
3. Results
Among 405 patients in the study, 164 had (40%) fever, 221 (55%) subfebrile temperatures, and 166 (41%) yielded visible hematomas. Overall, fever was not associated with hematoma (67/164 vs. 99/241; Pearson-χ², p=0.96). We equally lacked association when analyzing only the subfebrile level (156/385 vs. 10/18; p=0.21), when analyzing the temperatures day by day (Table 1, Figure 1), or solely for cases requiring surgical re-intervention (4/10 vs. 6/9; Fisher-exact-test, p=0.37). As continuous variables, the maximum temperatures on each of the seven for hematoma postoperative days were not higher for patients with hematoma (Wilcoxon-ranksum-tests; all p>0.10).
|
n=405 |
Fever (≥ 38.0°C) |
No fever |
Total |
|
Visible hematoma |
67 |
99 |
166 |
|
No hematoma |
97 |
142 |
239 |
|
Total |
164 |
241 |
404 |
All patients and throughout the hospitalisation (Pearson-χ-test; p=0.96)
|
n=403 |
Subfebrile (≥ 37.2°C-38.0°C) |
No subfebrile temperatures |
Total |
|
Visible hematoma |
156 |
10 |
166 |
|
No hematoma |
229 |
8 |
237 |
|
Total |
385 |
18 |
19 |
All patients and throughout the hospitalisation (Pearson-χ-test; p=0.21)
|
n=138 |
Fever (≥ 38.0°C) |
No fever |
Total |
|
Visible hematoma |
11 |
42 |
53 |
|
No hematoma |
18 |
67 |
85 |
|
Total |
29 |
109 |
138 |
Assessment at Day 4 post-surgery (Pearson-χ-test; p=0.95)
|
n=76 |
Fever (≥ 38.0°C) |
No fever |
Total |
|
Visible hematoma |
5 |
40 |
45 |
|
No hematoma |
3 |
28 |
31 |
|
Total |
8 |
68 |
76 |
Assessment at Day 7 post-surgery (Pearson-χ-test; p=1.00)
|
n=19 |
Fever (≥ 38.0°C) |
No fever |
Total |
|
Visible hematoma |
4 |
6 |
10 |
|
No hematoma |
6 |
3 |
9 |
|
Total |
10 |
9 |
19 |
All patients re-operated for lavage (Pearson-χ-test; p=0.37)
Table 1: Patients with and without fever or hematoma (exclusion of infections).
Left vertical axis- Fever (axillary) in °C (Celsuis); Bottom horizontal axis-Days; The thin lines on top of the columns represent the 95% confidence intervals
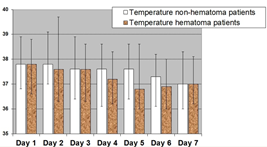
Figure 1: Occurrence of fever and hematoma during each of seven days postoperatively.
In multivariate analysis (Table 2), no parameter was associated with fever, including hematoma (odds ratio 0.9, 95%CI 0.3-2.3), emergency surgery (0.8, 0.3-2.3), or the Charlson co-morbidity index [15] (0.7, 0.3-1.9). Of note, the goodness-of-fit value of our final model was insignificant (p=0.19) and the Receiver-Operating-Curve (ROC) value was 0.75; highlighting an acceptable accuracy of our final model.
|
n=405 |
Univariate results |
Multivariate results |
|
Female sex |
0.9, 0.6-1.3 |
n.d. |
|
Age* |
1.0, 1.0-1.0 |
n.d. |
|
Body mass index* |
1.0, 0.9-1.1 |
1.0, 0.9-1.1 |
|
Surgery in winter time |
0.8, 0.5-1.4 |
n.d. |
|
ASA-Score [16]* |
1.0, 0.5-1.9 |
n.d. |
|
Fracture surgery |
1.1, 0.8-1.7 |
n.d. |
|
Duration of surgery |
1.0, 1.0-1.0 |
1.0, 1.0-1.0 |
|
Charlson morbidity index [15]* |
0.8, 0.6-1.3 |
0.7, 0.3-1.9 |
|
Emergency surgery |
1.0, 0.7-1.6 |
0.8, 0.3-2.3 |
|
Visible hematoma |
1.0, 0.7-1.5 |
0.9, 0.3-2.3 |
n.d.=not done; ASA=American Society of Anesthesiologists Score [16]; * as continuous variables
Table 2: Multivariate unmatched logistic regression analysis with outcome fever (≥ 38.0°C axillary; results are displayed as odds ratios, with 95% confidence intervals).
4. Discussion
We failed to establish an epidemiological relation between postoperative fever and hematoma in a large prospective study of adult orthopedic patients under anti-inflammatory drugs. Even if we stratified upon different postoperative days, between fever and subfebrile temperatures, or according the clinical need for surgical revisions of hematoma, we lacked association. We think that this lack is genuine, in as much as we performed our study in the postoperative setting with 19% of postoperative fever; regardless of hematoma [14]. Scientifically speaking, hematomas certainly provoke inflammation [1-3]. But is this enough to provoke fever under anti-inflammatory medication? Except for publications basing on single illustrative cases, surgical literature almost entirely lacks large-scale epidemiological data regarding this topic. The information has to be sought “between the lines” and, if it exists, rather supports our findings. For example, we published another prospective surveillance among polytrauma patients hospitalized in Intensive Care Units [17]. This is a population clearly suffering from severe trauma, multiple hematomas and need for blood transfusions. And yet, on a large scale, fever was only associated with true infection, but not with non-infectious causes such as hematomas or blood transfusions [17]. Gemer et al. investigated the occurrence of post-caesarian fever in the context of fifteen pelvic hematomas. Only five cases with superficial subfascial hematomas were associated with fever, while the majority of ten deep episodes of bladder-flap hematomas were not [11].
Our study has several limitations: We did not measure the hematoma size (the diagnosis was made visually and not by radiology), nor its evolution over time (e.g. progressive hematoma). Moreover, we assessed only the first postoperative week among adult uninfected patients hospitalized in our orthopedic and traumatology wards. Hence, we cannot pronounce on fever in infected hematomas, adolescents or other surgical disciplines. Finally, we are not investigating hematoma outside of the surgical site. For example, intracerebral [4, 6, 7] or subdural [2] hemorrhage is a classic example of (central) fever, which additionally might also be explained by the vicinity to the thermosensitive neurons in the preoptic area of the hypothalamus [2, 7].
5. Conclusion
In conclusion, our prospective database of adult orthopedic patients fails to link surgical hematoma and fever on a large epidemiological scale. Clearly, additional epidemiological studies are needed to drive firm conclusions. These studies should not be difficult to perform.
Funding
There was no funding for this study.
Conflict of Interest
All authors declare that they have no conflict of interest.
References
- Anochie PI. Mechanism of fever in humans. Internat J Microbiol Immun Res 2 (2013): 37-43.
- Frati A, Salvati M, Mainiero F, et al. Inflammation markers and risk factors for recurrence in 35 patients with a posttraumatic chronic subdural hematoma: a prospective study. J Neurosurg 100 (2014): 24-32.
- Kolar P, Schmidt-Bleek K, Schell H, et al. The early fracture hematoma and its potential role in fracture healing. Tissue Eng Part B Rev 16 (2010): 427-434.
- Honig A, Michael S, Eliahou R, et al. Central fever in patients with spontaneous intracerebral hemorrhage: predicting factors and impact on outcome. BMC Neurol 15 (2015): 6.
- Terada N, Tokuda Y. Acute aortic dissection as a cause of shaking chills. J Gen Fam Med 18 (2017): 293-294.
- Deogaonkar A, De Georgia M, Bae C, et al. Fever is associated with third ventricular shift after intracerebral hemorrhage: pathophysiologic implications. Neurol India 53 (2005): 202-206.
- Rincon F, Lyden P, Mayer SA. Relationship between temperature, hematoma growth, and functional outcome after intracerebral hemorrhage. Neurocrit Care 18 (2013): 45-53.
- Hamid NS, Spadafora PF, Khalife ME, et al. Pseudosepsis: rectus sheath hematoma mimicking septic shock. Heart Lung 35 (2006): 434-437.
- Hausmann MJ, Kachko L, Basok A, et al. Prolonged fever following kidney biopsy: a case report. Int Urol Nephrol 41 (2009): 423-425.
- Hu T, Liu Q, Xu Q, et al. Absorption fever characteristics due to percutaneous renal biopsy-related hematoma. Medicine (Baltimore) 95 2016: 37.
- Gemer O, Shenhav S, Segal S, et al. Sonographically diagnosed pelvic hematomas and postcesarean febrile morbidity. Int J Gynaecol Obstet 65 (1999): 7-9.
- Chmel H, Palmer JA, Eikman EA. Soft tissue hematoma as a cause of fever in the adult. Diagn Microbiol Infect Dis 11 (1998): 215-219.
- Uçkay I, Agostinho A, Belaieff W, et al. Noninfectious wound complications in clean surgery: epidemiology, risk factors, and association with antibiotic use. World J Surg 235 (2011): 973-980.
- Uçkay I, Agostinho A, Stern R, et al. Occurrence of fever in the first postoperative week does not help to diagnose infection in clean orthopaedic surgery. Int Orthop 35 (2011): 1257-1260.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40 (1987): 373-383.
- Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology 49 (1978): 239-243.
- Steinmetz S, Uçkay I, Cohen C, et al. Fever and its Association with Infection in Severely Injured Polytrauma Patients. M J Orth 1 (2016): 11.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 