Orthopaedic surgeons' perception and acceptance of augmented reality for PSI placement and implant positioning: A user-based evaluation
Borja Lara-Galdón1*, Tanya Fernández-Fernández2,3, Javier Orozco-Martínez1, Elena Aguilera-Jimenez4, Carla de Gregorio-Bermejo4, Amaia Iribar-Zabala4, Lydia Mediavilla-Santos2,3,5, Mónica García-Sevilla4, Rubén Pérez-Mañanes2,3,5,6, Javier Pascau4,6, José Antonio Calvo-Haro2,3,5,6
1Department of Orthopaedic Surgery and Traumatology. Hospital General Universitario Gregorio Marañón. Dr. Esquerdo 46, 28007. Madrid, Spain
2Department of Orthopaedic Surgery and Traumatology – Musculoskeletal Oncology Division. Hospital General Universitario Gregorio Marañón. Dr. Esquerdo 46, 28007. Madrid, Spain
3Faculty of Medicine, Universidad Complutense. Madrid, Spain
4Department of Bioengineering. Universidad Carlos III de Madrid. 28911. Leganés, Spain
5Advanced Planning and 3D Manufacturing Unit (UPAM 3D). Hospital General Universitario Gregorio Marañón. Madrid, Spain
6Instituto de Investigación Sanitaria Gregorio Marañón. Dr. Esquerdo 46, 28007. Madrid, Spain
*Corresponding Author: Borja Lara-Galdón, Department of Orthopaedic Surgery and Traumatology. Hospital General Universitario Gregorio Marañón. Dr. Esquerdo 46, 28007. Madrid, Spain
Received: 03 June 2025; Accepted: 10 June 2025; Published: 29 July 2025
Article Information
Citation: Borja Lara-Galdón, Tanya Fernández- Fernández, Javier Orozco-Martínez, Elena Aguilera- JimeÌnez, Carla de Gregorio-Bermejo, Amaia Iribar- Zabala, Lydia Mediavilla-Santos, Mónica García- Sevilla, Rubén Pérez-Mañanes, Javier Pascau, José Antonio Calvo-Haro. Orthopaedic surgeons' perception and acceptance of augmented reality for PSI placement and implant positioning: A user-based evaluation. Journal of Surgery and Research. 8 (2025): 358-364.
View / Download Pdf Share at FacebookAbstract
Background: Augmented reality (AR) has emerged as a promising tool to enhance precision and workflow in orthopaedic surgery. Its application in patient-specific instruments (PSI) placement and implant positioning is particularly relevant for improving spatial understanding and decisionmaking.
Methods: This cross-sectional, mixed-methods study evaluated the perception and acceptance of AR among 45 orthopaedic surgeons with varying experience levels. Participants used Microsoft HoloLens 2 to perform PSI placement and implant alignment tasks on a 3D-printed pelvic phantom. Performance metrics, structured Likert-scale questionnaires, and open-ended feedback were collected and analyzed.
Results: Participants reported high confidence levels in anatomical visualization and precision of PSI placement using AR. Significant differences in perceived usability and task completion time were observed between experienced and naïve users (p<0.05). Most participants highlighted the immersive interface, real-time guidance and personalization features as key advantages, while headset weight and visual lag were noted as areas for improvement.
Conclusions: AR was perceived as an intuitive and effective PSI placement and implant alignment tool. Its ability to integrate surgical planning directly into the operative field without external monitors offers a valuable alternative to conventional navigation systems. These findings support AR’s clinical applicability and suggest strong translational potential for routine use in orthopaedic workflows.
Keywords
<p>Augmented reality, Patient-specific instrument, Surgical navigation, Implant positioning, HoloLens, User perception, Mixed reality, Pelvic osteotomy</p>
Article Details
Introduction
The increasing demand for surgical precision, coupled with technological advancements in medical imaging and digital planning, has significantly transformed the landscape of orthopaedic surgery. In recent years, the incorporation of computer-assisted surgical techniques—ranging from 3D preoperative planning to navigation and robotic systems—has become a cornerstone in enhancing outcomes, particularly in complex cases requiring high anatomical accuracy, such as osteotomies and implant positioning [1-3].
One of the most promising evolutions in this digital transformation is the application of augmented reality (AR). AR directly overlays virtual 3D anatomical reconstructions, surgical guides or intraoperative plans onto the surgeon's field of view. This is achieved without diverting visual attention to external monitors or interrupting the sterile workflow, thereby improving focus and potentially reducing cognitive load [4]. Compared to other visualization modalities like 2D fluoroscopy or external screen-based navigation, AR provides a more intuitive, immersive experience that integrates digital planning into real-time surgical execution [5].
Recent advances in AR head-mounted displays, particularly Microsoft HoloLens and Magic Leap, have facilitated the translation of AR technology from experimental to clinical environments. Applications in spine surgery, neurosurgery, maxillofacial reconstruction and orthopaedic surgery have already demonstrated AR’s potential to enhance intraoperative navigation, increase surgeon confidence and reduce procedure time [6-8]. However, its use in tasks like patient-specific instruments (PSI) placement and personalized implant positioning - especially in orthopaedic trauma and joint reconstruction — remains relatively underexplored.
Patient-specific instruments, which are typically fabricated based on preoperative CT or MRI data, have demonstrated high potential in achieving accurate bone resections and optimal implant alignment in procedures such as high tibial osteotomy (HTO), total hip arthroplasty (THA) and periacetabular osteotomies [9,10]. Nevertheless, the challenge remains in ensuring that these guides are placed precisely on often-irregular bony anatomy, particularly in cases of deformity, poor exposure or soft-tissue interference. Conventional approaches rely heavily on tactile feedback and visual estimation, which can be limited in accuracy and repeatability.
In this context, AR offers a significant advantage: it allows the real-time visualization of cutting planes, implant trajectories and anatomical landmarks superimposed on the patient's body or a surgical phantom. Furthermore, AR platforms enable dynamic control over elements such as transparency, guide visibility and double-check verification steps, providing a personalized experience tailored to the surgeon's needs.
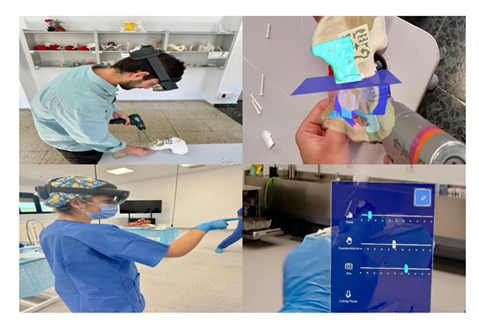
The current study aims to evaluate orthopaedic surgeons' perception and acceptance of AR-assisted PSI placement and implant positioning, focusing on user experience. Using a custom-designed AR software implemented through Microsoft HoloLens (Figure 1), we assessed the experience of 45 orthopaedic surgeons —ranging from AR novices to experienced users— on a pelvic surgical phantom. Our goal was to gather quantitative and qualitative data regarding usability, ergonomics, precision and surgeon preference. We hypothesize that AR improves spatial understanding, procedural control, and confidence, thereby positioning itself as a viable alternative or complement to current navigation and robotic systems.
Figure 1: Application of a novel AR-guidance system for PSI and implant positioning in orthopaedic surgery.
(A) User interacting with a 3D-printed pelvic model while wearing an AR headset to assist in PSI placement.
(B) AR overlay visualization showing anatomical structures, planned PSI guides, and cutting planes during simulated drilling.
(C) Clinical simulation where a surgeon uses the AR interface for intraoperative guidance.
(D) Example of the AR user interface displaying on/off bottoms and transparency adjustment bars for bones, PSIs, implant and cutting planes.
Materials and Methods
Study design and participants
A cross-sectional observational study with a mixed-methods approach (quantitative and qualitative) was conducted to evaluate users' and clinicians' perceptions of an augmented reality (AR) system for patient-specific instrumentation, osteotomy guidance and implant positioning in orthopaedic surgery, with potential clinical implications. The study was performed under controlled laboratory conditions simulating realistic surgical scenarios using a full-scale, anatomically accurate pelvic model.
A total of 45 orthopaedic surgeons voluntarily participated in practical sessions conducted in specialized hospital workshops. Among them, 23 had no previous exposure to AR technologies, 9 had previous contact as observers and 13 had previous direct use of AR. Participants represented various orthopaedic subspecialties, including trauma, reconstructive surgery, hip and pelvic arthroplasty and senior residents.
Procedure and AR System
The AR system was built on the Microsoft HoloLens 2 platform, featuring depth sensors, front-facing cameras and a stereoscopic holographic display. A custom Unity 3D application enabled accurate registration of CT-based anatomical models onto physical objects. Core functionalities included projection of virtual PSIs aligned with pelvic anatomy, visualization of osteotomy cutting planes, dynamic real-time guidance for implant placement, adjustable transparency, overlay toggling, and a built-in double-check mechanism using a color-coded system to visually confirm correct implant positioning during the procedure.
Each participant received a standardized 10-minute introduction to the AR interface, followed by 30 minutes to perform two tasks: (1) positioning of three PSIs (supra-acetabular, pubic and ischial) following the AR-projected PSI plan visualized over the phantom; and (2) alignment of a custom acetabular implant using visual cues. A 3D-printed pelvic phantom created from anonymized CT data allowed realistic anatomical constraint simulation. The PSIs were printed in high precision Rigid 10K resin Formlabs, Somerville, MA), which was selected for its dimensional stability, biocompatibility and suitability for surgical simulation, with anatomical locking geometries. Technical staff were present for support without interfering with task execution. Placement errors and interaction patterns were documented.
Evaluation Tools
After completing the hands-on session, participants answered a structured questionnaire consisting of: (1) Likert-type items (1 to 5) assessing perceived precision, usability, integration, ergonomics, learning curve and comparison to conventional methods, and (2) open-ended questions about advantages, limitations and suggestions for improvement. All responses were anonymous and analyzed through descriptive statistics and thematic coding.
Results
Quantitative outcomes
|
Evaluation Metric |
1 (Strongly Disagree) |
2 (Disagree) |
3 (Neutral) |
4 (Agree) |
5 (Strongly Agree) |
Positive Response (% answers 4–5) |
|
Improved anatomical understanding |
0 |
0 |
0 |
0 |
100 |
100 |
|
Ergonomic and visual comfort |
0 |
0 |
5 |
28 |
67 |
95 |
|
Integration of virtual and real elements |
0 |
0 |
14 |
52 |
34 |
86 |
|
Enhanced PSI placement precision |
0 |
0 |
37 |
48 |
15 |
63 |
|
Utility of AR-guided osteotomy visualization |
0 |
1 |
47 |
41 |
12 |
53 |
|
Utility of implant positioning guidance |
0 |
0 |
65 |
25 |
10 |
35 |
|
Usefulness of double-check confirmation |
0 |
0 |
22 |
57 |
21 |
78 |
|
Minor technical issues reported |
0 |
0 |
7 |
74 |
17 |
91 |
|
Discomfort due to HoloLens weight |
0 |
0 |
33 |
42 |
25 |
67 |
|
Perceived decalage (virtual-physical offset) |
0 |
26 |
42 |
31 |
0 |
24 |
Survey responses revealed high levels of satisfaction across key domains (Table 1). All participants (100%) agreed or strongly agreed that the system improved anatomical understanding, with 95% also reporting ergonomic and visual comfort. Integration of virtual and real elements received 86% positive responses, while perceived improvements in PSI placement precision reached 63%.
Table 1: Summary of key survey results evaluating user experience with the AR-guidance system for PSI and implant positioning in orthopaedic surgery.
Participants rated various aspects of the system on a 5-point Likert scale (1 = Strongly Disagree, 5 = Strongly Agree). High levels of agreement were reported for improved anatomical understanding (100%), ergonomic comfort (95%), and the integration of virtual and real elements (86%). Metrics such as PSI placement precision (63%) and osteotomy visualization (53%) received moderate agreement, while perceived decalage showed lower positive responses (24%), indicating an area for further optimization.
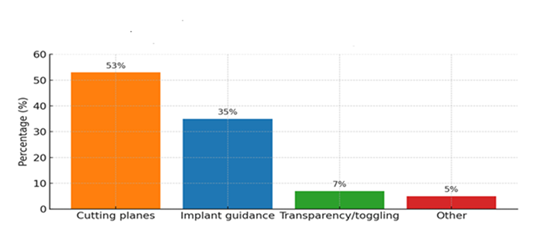
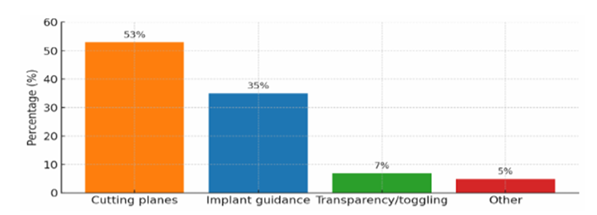
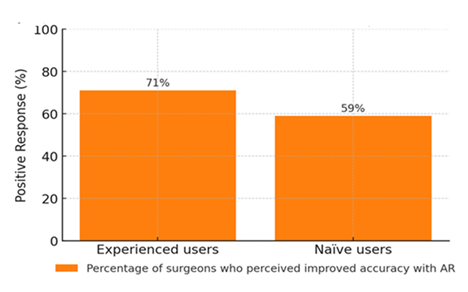
Regarding specific AR features, the most frequently cited as most useful was cutting plane visualization (53%), followed by implant guidance (35%) (Figure 2). Transparency/toggling features and other tools were less frequently mentioned (7% and 5%, respectively). Differences in perceived impact on surgical accuracy were noted between user groups: 71% of experienced AR users reported improved accuracy, compared to 59% of naïve users (Figure 3).
Survey respondents identified the most beneficial components of the AR platform for orthopaedic surgical planning and execution. The majority selected cutting plane visualization (53%) as the most useful feature, followed by implant guidance (35%). Fewer participants highlighted transparency/toggling features (7%) or other functionalities (5%) as most impactful. These findings highlight the critical role of precise anatomical and osteotomy plane representation in AR-assisted surgical workflows.
A comparison of subjective responses from surgeons with prior AR experience versus those without (naïve users) regarding the perceived enhancement in surgical accuracy provided by the AR system. A higher proportion of experienced users (71%) reported improved accuracy, compared to naïve users (59%), indicating a generally favourable perception of AR's utility across both user groups, with a trend toward greater confidence among those more familiar with the technology.
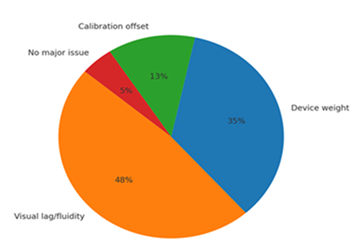
Despite the overall positive feedback, users identified several challenges (Figure 4). The most common issues were visual lag or limited fluidity (48%) and device weight (35%). Calibration offset was cited by 13%, while only 5% reported no significant issues.
Participants were asked to report any technical or ergonomic issues encountered while using the AR platform. The most cited challenge was visual lag or limited fluidity (48%), followed by device weight (35%) and calibration offset (13%). Only a small percentage of users (5%) reported no major issues, highlighting areas for improvement in future iterations of AR systems for surgical applications.
Task performance
Participants completed the two assigned tasks-PSI placement and implant positioning-in a mean time of 17.8 minutes (range: 13-26 minutes). Surgeons with prior AR experience performed significantly faster (mean: 15.2 minutes) compared to AR-naïve participants (mean: 19.6 minutes), indicating a potential learning curve effect associated with system familiarity.
Qualitative feedback
Analysis of open-ended responses revealed several consistent themes. Participants described the system as intuitive and immersive, emphasizing the benefit of aligning virtual planning elements directly within the surgical field without the need to divert gaze. Features such as adjustable transparency and toggleable visualization layers were identified as particularly useful, offering enhanced customization. Suggested improvements included reducing headset weight, improving system fluidity and stabilizing hologram anchoring.
User experience and expertise
Surgeons with prior AR experience (n = 13) provided higher ratings across multiple dimensions, including perceived precision, control, and overall utility. Notably, a majority of AR-naïve users (>60%) also reported improvements in performance and visualization when compared to conventional techniques.
Statistical analysis
Group-wise comparisons using Mann–Whitney U-tests revealed statistically significant differences between experienced and inexperienced users in perceived usability (p < 0.05) and confidence in PSI placement (p < 0.01).
Discussion
Findings highlight the optimal acceptance in orthopaedic surgery of this technology, and, therefore, its applicability. Compared to traditional techniques and alternative technologies, AR offers a unique balance between precision, visual contextualization, and workflow integration. Our study supports this claim with significant user-reported improvements in anatomical visualization, confidence in PSI placement, and satisfaction with user interface and ergonomic parameters.
AR was particularly valued for its ability to enhance intraoperative orientation through real-time superimposed guidance, minimizing reliance on external monitors, tactile anatomical estimation or repeated fluoroscopic verification. These features position AR as a strong candidate to complement or replace conventional navigation systems, especially in procedures requiring high precision, such as periacetabular osteotomy, acetabular reconstruction, and custom implant positioning [1,3].
When compared to computer-assisted navigation (CAN), AR presents several advantages. CAN systems typically rely on external screens that require the surgeon to look away from the operative field, disrupting focus and ergonomics. Moreover, setup time and calibration demands can increase intraoperative duration. A 2022 meta-analysis by Domb et al. demonstrated that while CAN improved component alignment in hip arthroplasty, it did not significantly reduce operative time or complications [11]. These findings are consistent with those of Bruschi et al., who in a 2023 systematic review comparing patient-specific instrumentation and navigation in bone tumour resections, found that PSI was associated with shorter operative times and comparable accuracy, while offering greater preoperative planning efficiency [12].
Robotic-assisted systems, although extremely accurate, present another set of limitations. Robotic platforms provide precision within millimetric tolerances, but they require high initial costs, complex maintenance, and extensive training. Studies by Batailler et al. and Parratte et al. have shown that while robotics increases reproducibility in total hip and knee arthroplasty, clinical superiority over manual or navigated techniques remains controversial [13,14]. In our study, AR allowed for dynamic guidance without robotic infrastructure, offering a more accessible yet effective solution.
Smartphone- or tablet-based AR systems have been proposed as low-cost alternatives, but lack immersive visualization, depth perception and hands-free operation, limiting their utility in actual surgical environments [15]. Head-mounted displays like HoloLens overcome these limitations, offering a stereoscopic, spatially anchored projection that maintains surgeon autonomy and sterility.
An additional advantage emphasized by our participants was the customization of the visual interface. The ability to adjust the transparency of overlays, activate or deactivate guidance elements and verify PSI or implant position using a "double-check" mode was highly appreciated. These features empowered surgeons to tailor the interface to their own visual and cognitive preferences, enhancing surgical confidence.
Nonetheless, some challenges remain. The weight of the headset and its impact during long procedures were a common concern. The current HoloLens model, despite being more balanced than its predecessor, may still introduce neck strain or discomfort during prolonged use, as reported by 67% of participants. Additionally, decalage-a slight misalignment between virtual content and real anatomy-was observed in 24% of cases. This misalignment appears to occur primarily when viewing holograms obliquely, likely due to the headset's camera being centrally aligned with the user's eyes. This central alignment can lead to perceptual discrepancies when the user shifts their gaze away from the direct line of sight, as the system's calibration may not fully account for angular deviations. Such findings are consistent with observations in other AR applications, where viewing angle and distance from virtual models significantly impact localization accuracy and user comfort [16,17].
Our results are consistent with those of Condino et al. who reported improved accuracy and reduced mental workload using AR for PSI placement in a preclinical setting [4]. Similarly, Gregory et al. emphasized that AR can significantly reduce task completion time and error rates when used for intraoperative navigation [7].
While this study focused on simulation using a pelvic phantom, the overwhelmingly positive feedback from participants, including those without prior AR experience, suggests a high translational potential for real surgical environments. Future clinical studies are needed to confirm these results in live surgeries and across varied orthopaedic procedures.
Conclusion
This study assessed surgeon perceptions of a novel AR-guidance system developed to support PSI placement and implant positioning in orthopaedic surgery. Participants reported a generally positive experience, citing enhanced anatomical visualization, intuitive interaction and improved procedural awareness.Although technical limitations-such as headset weight and visual latency-were identified, the system was widely perceived as a valuable tool with potential to support surgical planning and intraoperative decision-making. These findings indicate strong user acceptance and perceived benefit, underscoring the relevance of continued development and clinical implementation of AR technologies in orthopaedic surgery.
Conflicts of interest
The authors declare that they have no competing interests.
Acknowledgments
This study was performed with the financial support of the following projects: TED2021-132200B547 I00, TED2021-129392B-I00, PID2023-149604OB-I00 (Ministerio de Ciencia e 548 Innovación/AEI/10.13039/501100011033 and European Union 549 “NextGenerationEU”/PRTR).
References
- Wong KC. 3D-printed patient-specific applications in orthopedics. Orthop Res Rev 8 (2016): 57-66.
- Kendoff D. Computer-assisted surgery in orthopedics: current state and future perspectives. Expert Rev Med Devices 7 (2010): 529-535.
- Van Duren BH, et al. Clinical application of preoperative planning using 3D imaging. J Orthop Surg Res 15 (2020): 115.
- Condino S. Augmented reality in orthopedic surgery. Expert Rev Med Devices 18 (2021): 271-282.
- Farfalli GL. Augmented reality in bone tumor resection: a case report. J Orthop Case Rep (2020): 67-70.
- Cho JH. AR-assisted total knee arthroplasty: accuracy and efficiency. Comput Assist Surg 27 (2022): 27-34.
- Gregory TM. Augmented reality in orthopedic surgery: a systematic review. Orthop Traumatol Surg Res 104 (2018): 529-535.
- Sugano N. Computer-assisted orthopaedic surgery. J Orthop Sci 8 (2003): 442-448.
- Lonner JH. Robotics in knee arthroplasty: current concepts and future directions. J Bone Joint Surg Am 102 (2020): 472-478.
- Jenny JY, Picard F. Accuracy of computer-assisted surgery. Clin Orthop Relat Res 426 (2004): 160-165.
- Domb BG. Accuracy and outcomes of computer-assisted hip arthroplasty: a systematic review. J Am Acad Orthop Surg 30 (2022): 289-298.
- Bruschi A. What to choose in bone tumour resections? Patient specific instrumentation versus surgical navigation: a systematic review. Orthop Rev (Pavia).
- Batailler C. Robotic assistance in total hip arthroplasty: current concepts. EFORT Open Rev 6 (2021): 77-84.
- Parratte S. Robotic vs conventional total knee arthroplasty: a randomized clinical trial. Lancet 398 (2021): 676-684.
- Marques G, et al. Smartphone-based AR in surgery: A scoping review. Surg Innov 28 (2021): 344-351.
- Kriechling P. Augmented reality and shoulder replacement: a state-of-the-art review. Journal of Shoulder and Elbow Surgery 32 (2023): 1-10.
- Fotouhi J. Reflective-AR Display: An Interaction Methodology for Virtual-Real Alignment in Medical Robotics. arXiv preprint arXiv (2019): 1907.10138.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 