Procedures Never Explained in Textbooks: How to Correctly Convert a Closed-Suction Drain to a Closed-Gravity Drain, and How to Correctly Remove a Closed-Suction Drain Off Suction
Jenna Stelmar1,2,§, Shannon M Smith1,2, ,§, Andrew Chen1, John M Masterson1, Vivian Hu3, Maurice M Garcia1,2,4*
1Cedars-Sinai Medical Center, Los Angeles, Division of Urology; Los Angeles, CA.
2Cedars-Sinai Transgender Surgery and Health Program; Los Angeles, CA.
3University of California Los Angeles, School of Medicine; Los Angeles, CA.
4University of California San Francisco; Department of Urology and Department of Anatomy; San Francisco, CA.
§Equal authorship contribution
*Corresponding Author: Maurice M. Garcia, M.D., MAS, Cedars-Sinai Medical Center, Los Angeles, Division of Urology, 8635 W. Third Street, Suite 1070W, Los Angeles, CA 90048, USA
Received: 10 June 2022; Accepted: 17 June 2022; Published: 07 July 2022
Article Information
Citation:
Jenna Stelmar, Shannon M Smith, Andrew Chen, John M Masterson, Vivian Hu, Maurice M Garcia. Procedures Never Explained in Textbooks: How to Correctly Convert a Closed-Suction Drain (CSD) To A Closed-Gravity Drain (CGD), and How To Correctly Remove A CSD Off Suction. Journal of Surgery and Research 5 (2022): 423-430.
View / Download Pdf Share at FacebookAbstract
Objective
To describe a novel method to convert a closed-system suction drain to a highly efficient closed-system gravity-dependent drain and demonstrate its efficacy in an ex-vivo model.
Methods
We reviewed the 5 top-selling urology and surgery text/reference books for information on drainage systems. An ex-vivo model was designed with a reservoir of fluid connected to a Jackson-Pratt bulb drain. We measured the volume of fluid drained from the reservoir into the bulb while on-suction and off-suction. This was repeated using a novel modified bulb, where the bulb’s outflow stopper was replaced with a one-way valve oriented to allow release of pressure from the bulb.
Results
With the bulb on-suction, drainage was maintained regardless of the height of the drain relative to the reservoir. With the bulb off-suction, closed passive gravity-dependent drainage occurred only when the drain was below the fluid reservoir; drainage ceased at minimal volumes. With addition of a one-way valve and maintenance of the bulb below the level of the reservoir, drainage proceeded to completion.
Conclusion
How surgical drains work is not described in the leading urology and general surgery textbooks/reference books. Closed-system suction drains cannot be used to achieve passive gravity-dependent drainage without allowing release of displaced air from the bulb-lumen. The novel modified drain we describe affords reversible closed-system suction and passive drainage.
Keywords
<p>Surgical drain, Suction drainage, Gravity drainage, Post-operative management, Medical device design</p>
Article Details
1. Introduction
The use of drains is widespread across virtually all surgical specialties and has been practiced for centuries in medicine [1]. Prophylactic placement is used to prevent fluid collections, such as urinomas, seromas, abscesses, ascites, from forming post-operatively. Additionally, they allow for interrogation of the intracorporeal environment during evaluation of post-operative complications [2]. However, drains have been hypothesized to also increase risk of surgical site infection through retrograde migration of bacteria through the drain [3,4]. With modern improvement in surgical instruments and technique, the necessity of drain placement after various procedures has become increasingly questioned [2,5-8]. Nonetheless, certain surgical procedures continue to rely on wound drains to reduce the risk of post-surgery complications such as: leakage across a suture line after urethroplasty, urinoma after pyeloplasty or other urinary tract repairs, and seroma or hematoma beneath a skin graft in the neovaginal canal with gender affirming vaginoplasty [2,9]. Two types of drains are commonly employed: open-system passive drains, such as Penrose drains, which serve as a “wick” to allow drainage fluid to leak out of the body passively, and closed-system suction drains, such as Jackson-Pratt (JP) or Blake drains which create a pressure gradient into the drain lumen to evacuate fluid into a sealed reservoir. It is thought that closed systems confer less risk of contamination and subsequent infection of the surgical site, which accounts for their common use [10,11]. Nonetheless, in certain circumstances it is useful to convert closed-suction systems to passive gravity drainage. For example, in the context of an anastomotic leak where urine or another fluid is being aspirated across the anastomosis by a nearby suction drain, continued flow hinders healing of the anastomosis and risks development of a chronic fistula [2]. Because the suction drain cannot be removed post-operatively and replaced with a passive drain, the only option is to convert the closed-system suction drain to a closed-system passive drain. How to convert a closed-system wound drain from suction to passive drainage is not readily obvious [12]. Medical literature that focuses on techniques and outcomes related to the use of closed-system suction and open-system passive drainage in post-operative management appears to be sparse. Review of available medical-product wound drain devices finds no device that allows conversion from closed-suction to closed-passive gravity drainage. Furthermore, we reasoned that an additional challenge to converting a closed-system bulb-suction drain to closed-system passive gravity-dependent drainage is the bulb itself: when capped, it is filled with air that exerts pressure. Intuitively, in order for a given volume of fluid to enter the bulb, an approximately equal volume of air must be displaced from the bulb which current drain suction-bulbs are not designed to afford. We hypothesized that simply releasing suction inside a wound drain bulb but maintaining the bulb “closed” (stoppered), would not permit appreciable passive drainage into the bulb. The aims of this work are to: 1. Gain a better understanding of published educational content on how surgical drains function in textbooks or pocket-handbooks; 2. Test our hypothesis that conversion of a closed-system bulb-suction wound drain to passive gravity-dependent drainage by simply releasing suction within the closed bulb is inefficient; 3. Design a modified closed-system suction surgical wound drain that can be easily converted to closed-system passive drainage.
2. Methods
We identified the 5 top-selling urology and surgery textbooks, and the 5 top-selling surgery pocket reference handbooks listed on Amazon.com. We then searched each book for any discussion about surgical drains such as closed-system versus open-system, mechanism of function, recommended techniques for maintenance or removal, and preferred methods of drainage of fluid collections. A focused review of each book was made by searching the chapter and sub-chapter outline, to identify potentially relevant sections where surgical drains might be mentioned. We also searched the index of each book for key-words: “surgical drain,” “wound drain,” “suction,” “drainage,” “gravity-dependent,” and “bulb-suction”. We devised and tested an ex-vivo wound-drain model of closed-suction and closed-passive drainage using currently available drain products and by a technique commonly employed to convert a closed-system suction drain to closed-system passive drainage. We connected the tubing of a closed-system drain that normally resides inside the patient in an end-to-side fashion to the bottom-end of a 100 mL plastic graduated cylinder (Figure 1A). To accomplish this, we used a disposable Bovie® thermal-cautery pen to burn a hole in the graduated cylinder’s wall equal in diameter to the tubing. The drain tubing was inserted into the graduated cylinder and the insertion site was sealed with ethylene-vinyl acetate to prevent fluid leakage. Next, the graduated cylinder was filled with 100 mL of water and the drain was allowed to empty into the suction drain-bulb as the drain-bulb was held at various heights relative to the bottom of the graduated cylinder: 10 cm above the bottom, 0 cm from the bottom, 10 cm below the bottom, and 20 cm below the bottom. We performed multiple measurements with the system set to suction drainage with the bulb outflow-port capped. These measurements were repeated, but with the bulb “off-suction” (i.e. bulb was opened to allow re-pressurization to atmospheric pressure) without first squeezing it to create suction. Next, we repeated the same two measurements above, with the bulb set to suction and with the bulb off-suction, but with a one-way check-valve inserted into the bulb outflow-port. The one-way valve was oriented such that air/fluid can pass only from the drain-bulb to outside of the bulb (Figure 1B). For each of the four conditions, five measurements were taken at each height, and then averaged.
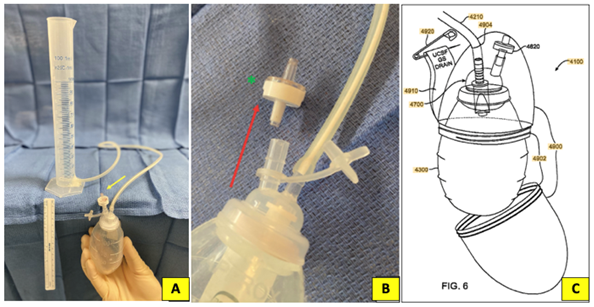
Figure 1: A. Model of closed system drainage system with one way valve attached to outflow port (yellow arrow. B. When a one- way check valve (green asterisk; harvested from an IV tubing kir) is attached to the uncapped outflow port, only unidirectional flow permitted: from inside to bulb to ourside (red arrow). C. Wearable rigid- walled container for the modified closed- system gravity drainage (CGD) wound drain described. (Figure from U.S. Patent #766,866,B2)
3. Results
3.1 Review of urology and surgery textbooks and pocket reference book
The 5 top selling urology textbooks, general surgery textbooks, and surgery pocket reference handbooks, sold on Amazon were identified, and reviewed (Table 1). None of the textbooks and pocket reference books searched discussed surgical drain options in any detail. Regarding use of surgical drains, most of the books reviewed mentioned following drain output to guide when to remove the drain. However, no reference text discussed selection between different surgical drain to achieve either suction or passive drainage, or which scenarios to choose active suction versus passive drainage using a surgical drain.
|
Rank |
Urology Textbooks |
|
1 |
Campbell-Walsh-Wein Urology, 12e.; Partin, Alan W., et al.; Elsevier, 2020. |
|
2 |
Smith's Urology, 19e.; J. McAninch & T. Lue; McGraw-Hill, Lange, 2020. |
|
3 |
Hinman's Atlas of Urologic Surgery, 4e.; J. Smith, S. Howards, G. Preminger, and R. Dmochowski; Elsevier, 2019. |
|
4 |
The Nurse Practitioner in Urology; M. Lajiness & S. Quallich; Springer, 2016. |
|
5 |
Textbook of Female Urology and Urogynecology, 4e.; L. Cardozo and D. Staskin; CRX Press, 2017. |
|
Rank |
Surgery Textbooks |
|
1 |
Current Surgical Therapy, 13e.; Cameron, John L. and Andrew M. Cameron; Elsevier, 2019. |
|
2 |
Schwartz’s Principles of Surgery, 11e.; Brunicardi, F. Charles, et al.; McGraw-Hill Education, 2019. |
|
3 |
Trauma, 9e; David Felicano, Kenneth Mattox et al., McGraw-Hill, 2021. |
|
4 |
Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice, 20e.; Townsend Jr., Courtney M., et al.; Elsevier, 2017. |
|
5 |
Zollinger's Atlas of Surgical Operations, 10e; McGraw-Hill, 2016. |
|
Rank |
Surgery Pocket-Reference Books |
|
1 |
Surgical Recall, 8e.; Blackbourne, Lorne.; Lippincott Williams & Wilkins, 2018. |
|
2 |
Dr. Pestana’s Surgery Notes, 5e.; Pestana, Carlos.; Kaplan Medical Test Prep, 2020. |
|
3 |
The Mont Reid Surgical Handbook, 7e.; Makley, Amy; Elsevier, 2017. |
|
4 |
The Washington Manual of Surgery, 8e; M. Klingensmith & P. Wise; Wolters-Kluwer, 2020. |
|
5 |
Surgery: A Case Based Clinical Review, 2e.; De Virgilio, Christian and Areg Grigorian; Springer, 2020. |
Table 1: Top-selling urology and surgical text and reference books reviewed
3.2 Ex-vivo model of close-system suction drainage
Closed passive-gravity drainage by opening the outflow port (allowing it to re-pressurize to atmospheric pressure) prior to re-capping the outflow port permitted only a small fraction of the 100 mL of water in the graduated cylinder to drain into the bulb: 4.2 mL at -10 cm bulb height relative to the reservoir and 7.6 mL at -20 cm (Figure 2A, blue columns). When the bulb was positioned at the bottom of the reservoir (0 cm) or above the bottom (i.e. +10 cm), there was no passive drainage of water into the bulb. Drainage with the drain bulb set to suction and with the outflow capped (i.e. normal use for a closed-system bulb suction wound drain) resulted in complete and uninterrupted drainage of all 100 mL of water inside the graduated cylinder, regardless of whether the drain bulb was positioned above or below the bottom of the graduated cylinder (Figure 2B, blue columns).
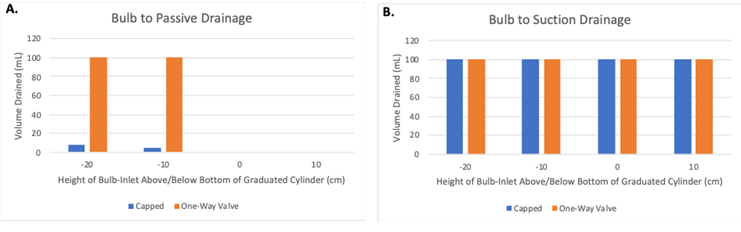
Figure 2: Drainage outcomes with drain off-suction, with outflow port closed with either the drain cap (blue bars) or with the drainage port plugged with our one- way valve oriented to allow drainage or air and/or fluid from inside of the bulb, to the outside (orange bars). B. Drainage outcomes when the bulb is set to active suction and placed at vaious heights above (+) or below the bottom of the graduated cylinder (-), with the drainage port either capped (blue bars) or occluded with a one-way value oriented to allow drainage of air/or fluid from inside the bulb, to the outside (orange bars).
3.3 Drainage with a one-way valve inserted into the bulb outflow port
Insertion of a one-way valve into the outflow port oriented such that it only allowed fluid and air passage from inside the bulb to outside resulted in spontaneous complete and uninterrupted drainage of all 100 mL of water from the graduated cylinder at any height below the bottom of the reservoir (Figure 2A, orange columns). Setting the bulb to suction with the one-way valve inserted into the outflow port resulted in complete and un-interrupted drainage of all 100 mL water into the bulb at all heights (Figure 2B, orange columns). With the drain bulb set to passive drainage as described above, squeezing the bulb resulted in expulsion of air through the one-way valve, which effectively returned the system from passive drainage to suction drainage.
4. Discussion
The decision to place a surgical drain at completion of surgery is based mostly on surgeon discretion. While the utility of suction versus passive gravity dependent drainage is debated in different clinical scenarios, effectively transitioning between the two forms of drainage remains an important and useful option for surgeons. In the present study we developed an experimental model that demonstrates how a closed-system one-way suction drain can be converted to a closed-system one-way passive (gravity-dependent) drain. We did not identify any literature that describes other techniques for the surgeon to easily convert a closed suction bulb drainage system into a gravity drain at bedside. In comparison to drains that are intended for use in gravity drainage systems, JP and Blake drain bulbs are not designed to expand and accommodate additional inflow of volume. The bulb consists of a one-way inflow port where the drainage tubing is attached, and an outflow port that is sealed with a cap after suction is applied. If the outflow port is sealed while the drain is released from suction, the air pressure within the bulb quickly increases with inflow of new fluid. Because displaced air in the bulb cannot escape and is forced to occupy a smaller volume, air pressure within the bulb quickly increases and opposes any fluid inflow from the wound drain. Instead, fluid begins to accumulate within the wound. Placement of our one-way valve on the outflow port allows air in the bulb to be displaced by incoming wound fluid. This maintains low, near atmospheric pressure inside the bulb. As expected, our modification allowed for immediate and complete gravity drainage when the drain was at any height below the reservoir (Figure 2A). One consequence of using the modified suction drain bulb for passive drainage is that if the bulb is accidentally squeezed, it automatically reverts again to a suction drain, which may not be desirable. Air and/or fluid inside the bulb is evacuated through the one-way valve and a negative pressure is re-established inside the bulb. A solution to prevent the bulb from being inadvertently squeezed is to simply place the bulb inside of a rigid-walled container. It also serves to collect any fluid that might drain from the bulb if overfilled while maintaining a closed system. We fashioned such a rigid container by re-purposing a plastic container and cutting a hole in its top for passage of the drain tubing. We attached a strap to the container, which could be pinned to a patient’s nightgown, so that the drain-bulb, set to passive drainage, could be positioned upright at all times (to avoid drain-fluid spillage via the one-way valve) below the level of the wound drain inside the patient’s body. We designed a working prototype that was filed under the United States Patent and Trademark Office (U.S. Patent Number 7,766,886,B2). The major limitation of our ex-vivo model is that our reservoir may not accurately model drainage of a fluid collection inside the human body, where drainage can be complicated by intercalation of fine tissues into the lumen of the drain. However, the fact that body tissues can naturally obstruct any closed-system wound drain should not be expected to affect or change the key findings of this study.
5. Conclusions
Educational literature regarding the function and selection of various wound drainage systems is lacking. We found that modifying a closed-system wound drain by inserting a one-way inflow valve into the outflow port significantly increases efficiency of passive gravity drainage within a closed system. The modification also offers easy conversion between suction and passive drainage and expands the surgeon’s toolkit for post-operative management options.
Author contributions
M.G. conceived of the presented idea. J.S. S.S., A.C., J.M., V.H., M.G. contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript.
Conflicts of interest
The authors disclose that Dr. Maurice Garcia patented a surgical drainage device system, US Patent # 7,766,886,B2. The authors have no financial conflicts of interest and the patent is not licensed with any product.
Acknowlegements
None
References
- Petrowsky H, Demartines N, Rousson V, et al. Evidence-based Value of Prophylactic Drainage in Gastrointestinal Surgery. Ann Surg 240 (2004): 1074-1085.
- Cecka F, Lovecek M, Jon B, et al. DRAPA trial-closed-suction drains versus closed gravity drains in pancreatic surgery: study protocol for a randomized controlled trial. Trials 16 (2015): 207.
- Felippe WAB, Werneck GL, Santoro-Lopes G. Surgical site infection among women discharged with a drain in situ after breast cancer surgery. World J Surg 31 (2007): 2293-2299.
- Vilar-Compte D, Mohar A, Sandoval S, et al. Surgical site infections at the National Cancer Institute in Mexico: a case-control study. Am J Infect Control 28 (2000): 14-20.
- Tsujinaka S, Konishi F. Drain vs No Drain After Colorectal Surgery. Indian J Surg Oncol 2 (2011): 3-8.
- Hoffmann J, Shokouh-Amiri MH, Damm P, et al. A prospective, controlled study of prophylactic drainage after colonic anastomoses. Dis Colon Rectum 30 (1987): 449-452.
- Urbach DR, Kennedy ED, Cohen MM. Colon and rectal anastomoses do not require routine drainage: a systematic review and meta-analysis. Ann Surg 229 (1999): 174-180.
- Chow SH, LaSalle MD, Stock JA, et al. Ureteroneocystostomy: to drain or not to drain. J Urol 160 (1998): 1001-1003.
- Kosins AM, Scholz T, Cetinkaya M, et al. Evidence-based value of subcutaneous surgical wound drainage: the largest systematic review and meta-analysis. Plast Reconstr Surg 132 (2013): 443-450.
- Dougherty SH, Simmons RL. The biology and practice of surgical drains. Curr Probl Surg 29 (1992): 559-623.
- Reiffel AJ, Barie PS, Spector JA. A Multi-Disciplinary Review of the Potential Association between Closed-Suction Drains and Surgical Site Infection. Surg Infect 14 (2013): 244-269.
- Akhtar N, Greenbaum AR, Thompson WRE, et al. Devac-ing a drain-the science of non-compliance. Br J Plast Surg 58 (2005): 81-83.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 