Realising Ideal Home Practice Models for Surgical Skill Development
Ayush Balaji1,2, Rishab Makam2,3*, Akshay Balaji1,2, Amir Moktari4, David O’Regan1,5*
1Blackbelt Academy of Surgical Skills (BBASS)
2Hull York Medical School, University of York, York, UK
3Hull University Teaching Hospitals Trust, Hull, UK
4Leeds University Teaching Hospitals Trust, Leeds, UK
5Medical Education Research and Development Unit (MERDU), Faculty of Medicine, Universiti Malaya, Kuala Lumpur, Malaysia
*Corresponding Author: David O’Regan, Medical Education Research and Development Unit (MERDU), Faculty of Medicine, Universiti Malaya, Kuala Lumpur, Malaysia
Received: 13 July 2025; Accepted: 22 July 2025; Published: 05 September 2025
Article Information
Citation: Ayush Balaji, Rishab Makam, Akshay Balaji, Amir Moktari, David O’Regan. Realising Ideal Home Practice Models for Surgical Skill Development. Journal of Surgery and Research. 8 (2025): 437-441.
View / Download Pdf Share at FacebookAbstract
Objective: The development of proficient skills in surgical education is essential. This paper realises ideal home practice models for enhancing surgical skills, stitching and dissection, emphasizing that these low fidelity models are realistic, cost-effective, accessible, enjoyable, and sustainable. The discussion is supported by a review of the literature, insights from courses, and anecdotal experiences.
Design: We investigated models for surgical training utilizing CT scans to identify their advantages such as haptic and real time feedback as well as practical application.
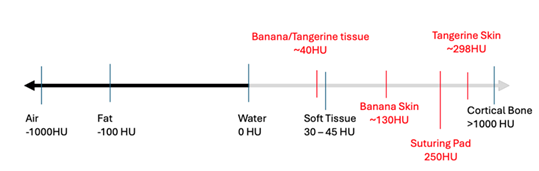
Results: Synthetic material does not compare to human tissue in the CT scanner. The banana and tangerine compare favourably to human tissue and offer real time haptics and feedback.
Conclusion: Organic models provide a cost-effective and sustainable option for home-based surgical practice.
Keywords
<p>Simulation, Surgical Education, Training Models, Feedback, Fidelity</p>
Article Details
Highlights
- • Common fruit and vegetables offer affordable, and accessible models for practice
- • Haptic feedback from these models is more appropriate for practice.
Introduction
The introduction of competency-based training requires that we need reliable and accurate models to develop surgical proficiency [1]. Traditional methods of surgical training have relied heavily on cadavers and animal models, but these methods can be costly, ethically challenging with limited availability and accessibility [2,3]. With an increasing emphasis on patient safety a there is a growing demand for alternative, ethical, and effective training models that can be easily integrated into surgical education. Practicing at home with realistic, inexpensive model [4], supplemented with expert assessment, can overcome these challenges.
There has been a surge in synthetic models, but they are expensive, non-recyclable, offer no feedback, and are not sustainable. While recent technological advancements such as 3D printing and virtual reality have been introduced to simulate surgical procedures, these models often lack the tactile feedback and realistic tissue response necessary for mastering surgical techniques. These challenges emphasize the need for low-cost, sustainable, and efficient training models [5].
Background
The educational paradigm in surgery is shifting towards the integration of Simulation-Based Education (SBE) as a supplementary, and in some cases, primary modality for skill acquisition. This transition is especially pertinent in surgery where, despite the diversity of specialisms, they all share fundamental skill sets [6,7]. The evolution of surgical simulation has been marked by a progression from low-fidelity models such as benchtop suture kits and laparoscopic boxes to high-fidelity, technologically advanced platforms, including 3D printing and augmented reality [8]. These advancements reflect an ongoing effort to address the limitations of traditional training methods while enhancing the educational experience for residents and students. A recent review in the field of urology emphasizes the crucial role of SBE in achieving proficiency, highlighting the emergence of immersive simulation tools with real-time feedback as essential [9]. There is also increasing discussion regarding the ethical and financial barriers associated with cadaveric and animal models [7]. We have previously addressed our concerns about benchtop skills acquisition, as this does not address the ergonomics of the standing surgeon and the functional anatomy of the upper limb [10].
Parallel research has explored the effectiveness of various suturing models (SM) in imparting basic surgical skills (BSS) to trainees. Studies examining different SMs, such as animal skin, commercial pads, and non-animal tissue, have highlighted the importance of intrinsic model characteristics—such as resistance, consistency, elasticity, feedback, and challenge—in skill acquisition [11,12]. Most commercially available suture pads are made of PTFE and silicone-based products. A survey of different surgical trainers, found a common theme regarding the ideal model: the model should offer realistic haptics and, if anything, be more difficult than the real scenario. The model should simulate the environmental and ergonomic factors, such as operating at depth and provide real-time haptics and feedback that engages the operator, fostering motivation to improve. Lastly, the models should be available, sustainable. Tactile and responsive visual feedback, an essential component of surgical training, is often absent in synthetic models, further highlighting the necessity of exploring more realistic, affordable alternatives like organic models.
Methods
We evaluated density differences different models using Computed Tomography (CT) scanning. We compared a standard silicon suture pad (type and origin) against the tangerine / orange and the banana, our typically used home models, against structures like the aorta and skin. To ensure accuracy and comparability of our CT scan results, a calibration test of the CT scanner, using a standardized Hounsfield units (HU) phantom, was used. This step was crucial to account for potential variances between different CT scanners and to establish a baseline for HU measurements across all models.
Results
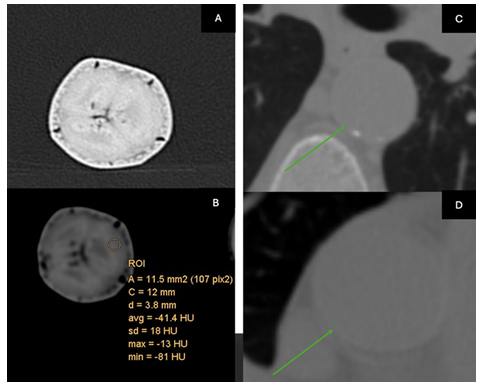
The banana compares will with aortic tissue (Figure 1)
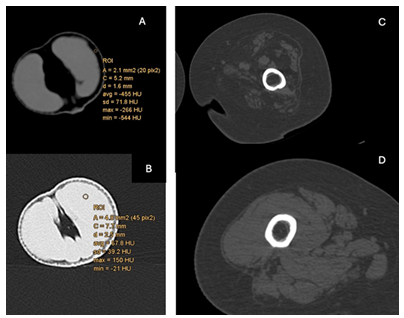
The tangerine compares well with the structures of the femoral canal (Figure 2)
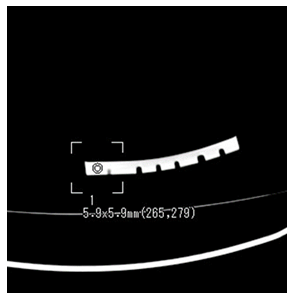
The suture pad’s density was recorded at approximately 265HU (Figure 3), the banana skin a was recorded at a maximum value of approximately 77HU, and the orange skin at a maximum value of approximately 304HU.
We mapped the standard deviation of HU values within each model to understand how uniformly density was distributed and to identify any areas of significant deviation from the reference tissue. This step was critical for evaluating the realism of each model in terms of tissue simulation (Figure 4)
Surgical educators were consulted to interpret the data in the context of surgical training. Their feedback focused on the relevance of the HU measurements to real-life surgical scenarios and how well each model's density range prepares trainees for handling human tissues.
Discussion
The choice of organic models was based on their unique textures and the immediate feedback they provide. For example, the banana offers a pliable yet resistant surface that mimics the initial tissue penetration and resistance encountered in real surgical scenarios [6], especially the stitching arteries. The failure to rotate the needle cleanly through the tissues is easily identified by skids and tears in the banana skin.
The tangerine spills juice if the membranes are breached; the separation of the skin from the flesh, the segments from each other and then the skin from the segment, needs increasing skill and dexterity with the dissecting scissors. The appearance of juice, and maceration of the flesh offer immediate feedback.
The organic models were selected not only for their ease of access and cost-effectiveness but also because they provide a diverse range of tactile experiences that closely mimic various tissue types. We believe the ideal model must be available, cost-effective, sustainable, reusable or recyclable, and, most importantly, offer real-time feedback. The trainers felt the models should be more challenging than real tissue to encourage good tissue handling techniques [12].
Organic suture models offer better haptic feedback and have been used in many disciplines [13,14]. Meat products, although relevant have a limited shelf life compared to vegetables [15] and may not be culturally acceptable. Training on low fidelity models has been shown to be as effective as training on high fidelity models [16].
The diagram in our study highlights the HU of different tissues and the limitations of plastic models. Plastic models, while useful for some basic skills, lack the variability and feedback that organic models provide, which are critical for effective learning. The real-time feedback from organic models, such as the blackening of a banana and the juice of an orange or tangerine when cutting or dissecting, indicates that the user is in the wrong plane, providing immediate feedback [5]. The shape and geometry of organic material challenge the operator in all spatial domains, requiring an appreciation of body habitus and the function of the upper limb [10].
One of the pivotal, but not surprising, findings from our CT scan comparison is the variation in tissue density across different organic models. We are drawn to those exhibiting lower density levels, such as the banana. This characteristic renders the tissue less forgiving, necessitating delicate and more deliberate handling by the trainee. Such a trait is invaluable in surgical training as it mirrors the intricacies involved in managing human tissue during critical procedures [5]. A prime example highlighted in our study is the application of these handling principles to the aorta, especially in aortic dissection. The tissues are very friable and not forgiving of poor needle rotation. Likewise, in corneal transplant, irregular, poorly spaced interrupted sutures will result in blurred vision [17]. Precision and care are imperative. Low-fidelity models offer the nuanced understanding and application of these principles that significantly elevate a trainee's skill set and prepare them for the complexities of real-world surgical scenarios [18].
The sensory feedback from these models, such as the tactile feel of needle resistance or the visual cue from the banana's oxidation, provides immediate and tangible reinforcement of correct or incorrect technique, which is crucial for developing muscle memory in surgical trainees [12].
Similarly, the tangerine model, with its unique structure, allows for the practice of dissection in subtle planes. These planes can be explored with dissecting scissors at various levels: removal of the skin, removal of a segment, and then removal of the segment skin to expose the flesh. The spilling of juice indicates transgression of tissue planes
The immediate feedback provided by the organic models offer direct learning benefits, encouraging trainees to correct their technique in real-time, thereby accelerating the learning process [19]. Self -controlled feedback has been found to be more effective than externally controlled practice [20] with self-directed practice schedules being more conducive to learning [21,22]. The essence of a good learning model must be that the operator can see when things are not correct; just watching a video and using intestines of a pig does not enable that learning [23].
Models do not have to mimic real anatomy or be anatomically positioned. It is more important to define the intended learning outcome (ILO) for the model or part of the model. We believe this is summarized into two domains: ergonomics (how to position the body, upper limb, and instrument) and haptics (mimicking the feel of the tissue). Both require knowledge of the different types of instruments available for the task and proper instruction on how to hold the instrument [24]. These fundamentals are appreciated in sports and the acquisition of motor skills but are, we believe, poorly applied to surgery. Martial arts is a good example. It is called an art because it requires study, a growth mindset, and a lifetime of mastery. Technique triumphs over speed and power. In Karate, it is emphasized to practice the correctness of every move and nuance until you cannot get it wrong. This is true of surgery, but we should teach in this manner.
Our methodology provides a rigorous, quantifiable basis for evaluating and recommending surgical training models, as evidenced by the HU density comparison of human tissue and simple organic models. There is a striking similarity in tissue density between our selected organic models and human tissue, offering a promising avenue for realistic hands-on practice and tools for education [8].
A noteworthy aspect of our training models is their sustainability. This focus aligns with global efforts to reduce waste and promote environmentally friendly practices in medical training [19]. All the models described here are organic and can even be eaten or used as compost following their use.
Delegates who have practiced using these models report that they become absorbed in the task, fuelled to improve their skills. It is fun and challenging, fostering a growth mindset. We have observed this at the successful walk-in skills labs held at the annual general meetings of the Association of Surgeons in Training in 2023, 2024 and 2025. (These were sponsored by B. Braun, and the marketing ‘Can you feel it?’ and ‘It is in your hands’ was very apt).
Low fidelity models that offer immediate visual feedback, encourage persistent practice, and foster self-directed learning and mastery [24]. Intrinsic motivation and the growth mindset, pivotal in sports psychology, with the drive to perform an activity for its inherent satisfaction, are crucial for maintaining long-term engagement and perseverance. The thought process behind coaching and training in sports is equally transferable to surgery. The growth mindset, the belief that abilities can be developed through dedication and hard work, fosters resilience, a habit of practice and a passion for learning [19].
Conclusion
Our findings illuminate the potential of organic models as valuable tools in the repertoire of surgical training. The similarity in tissue density between these models and human tissue, particularly those of lower density, accentuates the importance of precision and care in surgical procedures. The real-time feedback provided by these models, such as the blackening of a banana and the juice of an orange or tangerine, is essential for effective learning and skill refinement [5,19]. We believe these models challenge surgical techniques and offer an opportunity to rethink the trainer-trainee paradigm in surgery.
References
- Gawad N, Fowler A, Mimeault R, et al. The Inter-Rater Reliability of Technical Skills Assessment and Retention of Rater Training. Journal of surgical education 76 (2019): 1088-1093.
- Denadai R, Saad-Hossne R, Todelo AP, et al. Low-fidelity bench models for basic surgical skills training during undergraduate medical education. Revista do Colégio Brasileiro de Cirurgiões 41 (2014): 137-145.
- Sharma D, Agrawal V, Biyani CS, et al. Low-cost Simulation in Urology. Switzerland: Springer International Publishing AG 11 (2022): 267-287.
- Hosain MM. Microsurgery Training: Are the Live Models Era Coming in to the Tail? – A Literature Review. Journal of Advances in Medicine and Medical Research 8 (2021): 97-109.
- Cardoso SA, Suyambu J, Iqbal J, et al. Exploring the Role of Simulation Training in Improving Surgical Skills Among Residents: A Narrative Review. Cureus (Palo Alto, CA) 15 (2023): e44654-e44654.
- Murphy G, Khan MA, Lathif A, et al. A banana a day keeps wound failure away: comparing the utility of fruit, pig, and synthetic skins for suturing practice. Medical journal of Australia 215 (2021): 536-540.
- Kneebone RL, Scott W, Darzi A, et al. Simulation and clinical practice: strengthening the relationship. Medical education 38 (2004): 1095-1102.
- Badash I, Burtt K, Solorzano CA, et al. Innovations in surgery simulation: a review of past, current and future techniques. Annals of translational medicine 4 (2016): 453-453.
- Singh A. Simulation-based training in laparoscopic urology - Pros and cons. Indian journal of urology 34 (2018): 245-253.
- O'Regan D. Making a Stand. Journal of surgical education 81 (2024): 167-171.
- Gonzalez-Navarro AR, Quiroga-Garza A, Acosta-Luna AS, et al. Comparison of suturing models: the effect on perception of basic surgical skills. BMC medical education 21 (2021): 250-259.
- Ayache N, Cotin S, Delingette H, et al. Surgery simulation with visual and haptic feedback. London: Springer London 12 (1998): 311-316.
- Denadai R, Souto LRM. Organic bench model to complement the teaching and learning on basic surgical skills. Acta cirúrgica brasileira 27 (2012): 88-94.
- Shah S, Shah S, Das JD, et al. Proposing a novel organic bench model utilizing vegetable to enhance basic vitiligo surgery skills. Journal of cutaneous and aesthetic surgery 18 (2025): 58-60.
- Denadai R, Oshiiwa M, Saad-Hossne R. Teaching elliptical excision skills to novice medical students: a randomized controlled study comparing low- and high-fidelity bench models. Indian journal of dermatology. 59 (2014): 169-175.
- Bafna RK, Kalra N, Asif MI, et al. Suturing large therapeutic corneal grafts based on donor size: A simplified technique for the novice corneal surgeon. European journal of ophthalmology 31 (2021): 1417-1421.
- Chahal B, Aydin A, Ahmed K. Virtual reality vs. physical models in surgical skills training. An update of the evidence. Current opinion in urology 34 (2024): 32-36.
- Taraporewalla K, Barach P, Van Zundert A. Teaching Medical Procedural Skills for Performance. Clinics and practice 14 (2024): 862-869.
- Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance: a review of influential factors. Medical education 44 (2010): 75-84.
- Chiviacowsky S, Wulf G. Self-Controlled Feedback: Does it Enhance Learning Because Performers Get Feedback When They Need It? Research quarterly for exercise and sport 73 (2002): 408-415.
- Lessa HT, Chiviacowsky S. Self-controlled practice benefits motor learning in older adults. Human movement science 40 (2015): 372-380.
- Chartrand G, Soucisse M, Dubé P, et al. Self-directed learning by video as a means to improve technical skills in surgery residents: a randomized controlled trial. BioMed Central Ltd 12 (2021).
- Frischknecht AC, Kasten SJ, Hamstra SJ, et al. The objective assessment of experts' and novices' suturing skills using an image analysis program. Academic Medicine 88 (2013): 260-264.
- Jiang J, Xing Y, Wang S, et al. Evaluation of robotic surgery skills using dynamic time warping. Computer methods and programs in biomedicine 152 (2017): 71-83.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 