Role of preoperative Incentive Spirometry in prevention of postoperative pulmonary complications after abdominal surgery
Maham Arshad*, Azka Ashraf, Ghanwa Muzammil, Rohma Arshad, Awais Amjad Malik, Jehanzaib Rashid
PGR, Lahore General Hospital, Lahore, Pakistan
*Corresponding Author: Maham Arshad, PGR, Lahore General Hospital, Lahore, Pakistan
Received: 04 December 2024; Accepted: 10 December 2024; Published: 30 December 2024
Article Information
Citation: Maham Arshad, Azka Ashraf, Ghanwa Muzammil, Rohma Arshad, Awais Amjad Malik, Jehanzaib Rashid. Role of preoperative Incentive Spirometry in prevention of postoperative pulmonary complications after abdominal surgery. Journal of Surgery and Research. 7 (2024): 553-559
View / Download Pdf Share at FacebookAbstract
Background: Postoperative pulmonary complications (PPCs) are a major cause of morbidity following abdominal surgeries, particularly midline laparotomies. Incentive spirometry (IS) promotes lung expansion and prevents PPCs. This study evaluates the effectiveness of preoperative IS in reducing PPCs in patients undergoing elective midline laparotomies lasting more than 2 hours, with consistent perioperative management by the same surgical and anesthesia teams.
Methods: A prospective, randomized controlled trial was conducted at Lahore General Hospital, involving 100 patients undergoing elective midline laparotomies. Patients were randomly assigned to an intervention group (preoperative and postoperative IS) or a control group (postoperative IS only). Postoperative oxygenation was monitored using PaO2 and SpO2, and PPCs (atelectasis, pneumonia, pleural effusion) were diagnosed clinically and radiologically. Secondary outcomes included hospital stay, postoperative pain (VAS), and time to first mobilization.
Results: The intervention group had a significantly lower incidence of PPCs (10% vs. 26%, p = 0.01) and greater postoperative oxygenation improvement (PaO2 increase: 18% vs. 10%, p = 0.02). Hospital stays were shorter (6 vs. 9 days, p = 0.01), pain scores lower (VAS: 3.0 vs. 4.2 at 48 hours, p = 0.02), and mobilization earlier (28 vs. 36 hours, p = 0.03).
Conclusions: Preoperative IS effectively reduces PPCs, improves oxygenation, shortens hospital stays, and promotes faster mobilization. Routine preoperative IS should be integrated into surgical protocols, particularly in resource-limited settings, to optimize patient outcomes.
Keywords
<p>Preoperative, Postoperative, Spirometry, Surgery</p>
Article Details
Introduction
Background: Postoperative pulmonary complications (PPCs) are a leading cause of morbidity and prolonged recovery following major abdominal surgeries, including midline laparotomies. PPCs such as atelectasis, pneumonia, and pleural effusion are associated with increased hospital stays and healthcare costs, contributing significantly to postoperative morbidity [1,2]. The incidence of PPCs in abdominal surgeries is reported to range from 10% to 40%, depending on patient comorbidities, surgical complexity, and perioperative care [3]. In particular, surgeries lasting more than 2 hours are at increased risk of PPCs due to the combined effects of prolonged anesthesia, diaphragmatic dysfunction, and reduced postoperative lung volumes [4].
Incentive spirometry (IS) is a non-invasive respiratory therapy designed to promote lung expansion and prevent pulmonary complications. IS encourages deep, sustained inhalations, which improve alveolar ventilation and reduce the likelihood of atelectasis [5]. Although IS is commonly used in the postoperative setting, recent studies suggest that preoperative IS may also be beneficial, particularly in optimizing lung function before surgery and preparing patients for postoperative recovery [6]. Preoperative IS could enhance lung volume, improve diaphragmatic movement, and decrease the risk of PPCs by conditioning the lungs before the surgical insult [7].
Rationale for study: Despite the widespread use of IS in postoperative care, there remains a gap in understanding its role when initiated preoperatively, especially in abdominal surgeries like midline laparotomies, where PPCs are prevalent due to the surgical impact on respiratory mechanics [8]. Abdominal incisions, particularly those involving the diaphragm, further compromise lung expansion and contribute to the development of PPCs [9]. Moreover, the duration of surgery, especially when exceeding 2 hours, increases the risk of PPCs due to longer periods of immobility and mechanical ventilation, making this population an ideal group for studying the effects of preoperative IS [10].
Few studies have focused on preoperative IS specifically in the context of major abdominal surgeries like midline laparotomies. Research on preoperative respiratory interventions has generally been limited to cardiothoracic surgeries, where preoperative IS has demonstrated reductions in PPCs [11,12]. However, the potential benefits of preoperative IS in abdominal surgeries have yet to be fully explored. By including only midline laparotomies lasting more than 2 hours, this study ensures a homogenous patient population, enabling an accurate assessment of the impact of preoperative IS.
To reduce variability, we standardized surgical procedures by ensuring that all surgeries were performed by the same surgical and anesthesia teams. Controlling these factors ensures that any observed differences in outcomes can be more confidently attributed to the use of preoperative IS, thus strengthening the study's validity [13].
Study objective: This study aims to evaluate the efficacy of preoperative IS in reducing the incidence of PPCs in patients undergoing elective midline laparotomies lasting more than 2 hours. The secondary objectives include assessing the impact of IS on postoperative oxygenation levels, length of hospital stay, postoperative pain, and time to first mobilization. By focusing on a high-risk surgical population and controlling key perioperative variables, this study seeks to provide evidence-based recommendations for incorporating preoperative IS into routine preoperative care protocols, particularly in resource-constrained environments [14].
Methods
Study design: This prospective, randomized controlled trial was conducted at the Department of General Surgery, Lahore General Hospital, from July 2023 to December 2023. The aim was to evaluate the effectiveness of preoperative incentive spirometry (IS) in reducing the incidence of postoperative pulmonary complications (PPCs) in patients undergoing elective abdominal surgery.
Study population: The study included 100 adult patients (aged 18-70 years) who were scheduled for elective midline laparotomies lasting more than 2 hours. This selection criterion ensured that all patients experienced comparable surgical stress, providing a controlled environment for evaluating the effects of IS. Patients were excluded if they had pre-existing chronic pulmonary diseases (e.g., COPD, asthma), underwent emergency surgeries, or were unable to perform IS due to cognitive or physical limitations.
Inclusion criteria:
- Adults aged 18 to 70 years.
- Scheduled for elective midline laparotomy lasting more than 2 hours..
- No history of chronic pulmonary disease.
Exclusion criteria:
- Patients with chronic obstructive pulmonary disease (COPD), asthma, or other chronic respiratory conditions.
- Emergency surgical cases.
- Patients unable to comprehend or physically perform IS.
- Pregnant women.
Randomization: Participants were randomly assigned to one of two groups using a computer-generated randomization sequence:
- Incentive Spirometry Group (n = 50): Patients in this group received preoperative IS training and were instructed to perform IS three times daily for 10 to 20 minutes per session, starting one week prior to surgery. IS was continued postoperatively as part of routine care.
- Control Group (n = 50): Patients in this group received only standard postoperative IS care without preoperative intervention.
Surgical and Anesthesia Teams: To control for variability, all surgeries were performed by the same surgical and anesthesia teams. This measure ensured that differences in surgical technique, anesthesia management, and perioperative care were minimized, allowing the study to attribute differences in outcomes more directly to the use of preoperative IS.
Intervention Protocol: The incentive spirometry (IS) protocol for the intervention group included the following:
- • Patients were provided with a standardized IS device.
- • A respiratory therapist trained patients on the proper usage of the device.
- • Patients performed IS three times daily for 10 to 20 minutes per session, aiming to reach a target volume, followed by a breath hold for 3 to 5 seconds.
- Postoperatively, IS was resumed as soon as patients were stable and alert.
Compliance with the IS protocol was monitored through a daily log maintained by the patients, which was reviewed by the clinical staff. For both groups, postoperative IS was initiated on day 1 after surgery, with the target of performing IS three times daily for 10-20 minutes per session.
Outcomes: The study focused on the following primary and secondary outcomes:
- • Primary outcome: The incidence of PPCs, including atelectasis, pneumonia, and pleural effusion, within 30 days postoperatively. PPCs were diagnosed based on standardized clinical and radiographic criteria:
-Atelectasis: Diagnosed by chest X-ray showing partial or complete lung collapse.
-Pneumonia: Diagnosed by new or progressive infiltrates on chest X-ray, combined with fever, leukocytosis, and positive sputum culture.
-Pleural Effusion: Diagnosed by chest X-ray or ultrasonography showing fluid accumulation.
- • Secondary outcomes:
-Postoperative oxygenation levels, measured using arterial blood gas (ABG) analysis for PaO2 and continuous SpO2 monitoring. PaO2 was measured within the first 24 hours postoperatively, while SpO2 was monitored continuously for the first 72 hours.
-Length of hospital stay (in days).
-Postoperative pain, assessed using the Visual Analog Scale (VAS) at 24, 48, and 72 hours.
-Early mobilization, defined as the time to first ambulation (in hours) and frequency of ambulation within the first 72 hours postoperatively.
Statistical analysis: Data were analyzed using SPSS version 26. Descriptive statistics were used to summarize patient demographics and baseline characteristics. Categorical variables such as the incidence of PPCs were compared between groups using the chi-square test, while continuous variables (e.g., PaO2, length of hospital stay, VAS scores) were analyzed using independent t-tests or Mann-Whitney U tests, as appropriate. A p-value < 0.05 was considered statistically significant.
Results
Patient demographics and baseline characteristics: A total of 100 patients were randomized into the study, with 50 patients in the Intervention Group (preoperative IS) and 50 in the Control Group (postoperative IS only). The mean age was 46.2 ± 11.8 years, and there were no significant differences between the groups in terms of age, gender, body mass index (BMI), or smoking history. Both groups had a comparable distribution of comorbidities, including diabetes and hypertension (p > 0.05 for all comparisons) (Table 1) (Figure 1).
|
Variable |
Intervention Group (n = 50) |
Control Group (n = 50) |
p-value |
|
Age (years, mean ± SD) |
46.0 ± 12.0 |
46.4 ± 11.6 |
0.85 |
|
Male (%) |
56% |
58% |
0.78 |
|
Diabetes (%) |
22% |
24% |
0.8 |
|
Hypertention (%) |
30% |
28% |
0.72 |
|
Smoking (%) |
34% |
36% |
0.76 |
Table 1: Patient demographics and baseline characteristics
Incidence of Postoperative Pulmonary Complications (PPCs): The primary outcome, the incidence of PPCs, was significantly lower in the Intervention Group compared to the Control Group. PPCs occurred in 5 patients (10%) in the Intervention Group and 13 patients (26%) in the Control Group (p = 0.01) (Table 2) (Figure 2).
|
Complication |
Intervention Group (n = 50) |
Control Group (n = 50) |
p-value |
|
Atelectasis |
2 (4%) |
5 (10%) |
0.24 |
|
Pneumonia |
2 (4%) |
4 (8%) |
0.4 |
|
Pleural Effusion |
1 (2%) |
4 (8%) |
0.18 |
|
Total PPCs |
5 (10%) |
13 (26%) |
0.01 |
Table 2: Incidence of postoperative pulmonary complications
Postoperative Oxygenation: Postoperative oxygenation, as measured by PaO2 and SpO2, was significantly better in the Intervention Group. The mean increase in PaO2 was 18% in the Intervention Group compared to 10% in the Control Group (p = 0.02). SpO2 levels were also higher in the Intervention Group, although the difference was not statistically significant (Table 3) ( Figure 3).
|
Time Point |
Intervention Group (Mean ± SD) |
Control Group (Mean ± SD) |
p-value |
|
Preoperative (baseline) |
81.0 ± 10.2 mmHg |
80.6 ± 10.8 mmHg |
0.8 |
|
Postoperative (24 hours) |
95.6 ± 11.5 mmHg |
88.6 ± 12.0 mmHg |
0.03 |
|
% Change in PaO2 |
18% |
10% |
0.02 |
Table 3: Postoperative Oxygenation (PaO2 Levels).
Length of hospital stay: The median length of hospital stay was significantly shorter in the Intervention Group compared to the Control Group. Patients in the Intervention Group had a median hospital stay of 6 days (IQR: 5-7 days), while those in the Control Group had a median stay of 9 days (IQR: 8-10 days) (p = 0.01) (Table 4).
|
Group |
Median (IQR) |
p-value |
|
Intervention Group |
6 days (5-7 days) |
|
|
Control Group |
9 days (8-10 days) |
0.01 |
Table 4: Length of hospital stay.
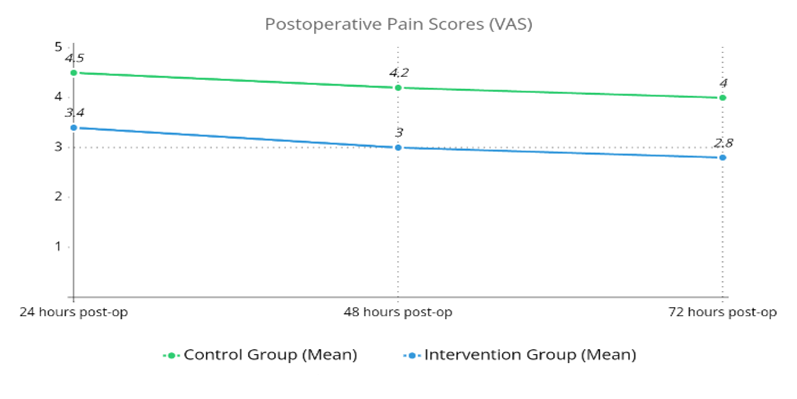
Pain Scores: Postoperative pain, as assessed by the visual analog scale (VAS), was lower in the Intervention Group compared to the Control Group at all measured time points. The mean VAS score at 48 hours postoperatively was 3.0 in the Intervention Group compared to 4.2 in the Control Group (p = 0.02) (Table 5) (Figure 4).
|
Time Point |
Intervention Group (Mean ± SD) |
Control Group (Mean ± SD) |
p-value |
|
24 hours post-op |
3.4 ± 1.0 |
4.5 ± 1.2 |
0.04 |
|
48 hours post-op |
3.0 ± 0.9 |
4.2 ± 1.1 |
0.02 |
|
72 hours post-op |
2.8 ± 0.8 |
4.0 ± 1.0 |
0.01 |
Table 5: Postoperative Pain Scores (VAS).
Early Mobilization: Patients in the Intervention Group achieved early mobilization significantly faster than those in the Control Group. The mean time to first ambulation was 28 hours in the Intervention Group compared to 36 hours in the Control Group (p = 0.03).
Discussion
This study demonstrates that preoperative incentive spirometry (IS), when added to standard postoperative IS, significantly reduces postoperative pulmonary complications (PPCs) in patients undergoing elective midline laparotomies lasting more than 2 hours. The results highlight that preoperative IS not only lowers the incidence of PPCs but also improves postoperative oxygenation, shortens hospital stay, reduces postoperative pain, and accelerates early mobilization.
Interpretation of results: The incidence of PPCs was significantly lower in the intervention group, with a PPC rate of 10% compared to 26% in the control group (Table 2) (Figure 2). This reduction in PPCs aligns with prior studies demonstrating the effectiveness of IS in preventing atelectasis, pneumonia, and pleural effusion [1,10]. The preoperative use of IS likely prepared the respiratory system by enhancing lung expansion and increasing diaphragmatic function before surgery, leading to better postoperative outcomes.
The use of preoperative IS was especially effective in improving postoperative oxygenation, as indicated by the greater increase in PaO2 in the intervention group compared to the control group (Table 3) ( Figure 3). Improved PaO2 levels suggest better alveolar ventilation and gas exchange, which are critical for reducing PPCs and promoting faster recovery [5]. The addition of both PaO2 and SpO2 monitoring in this study ensured a comprehensive assessment of respiratory function, allowing us to detect subtle improvements in oxygenation.
Surgical and Anesthesia Team Control: By standardizing the surgical and anesthesia teams for all procedures, we minimized potential confounders that could affect outcomes. Previous studies have highlighted the variability introduced by different surgical and anesthesia techniques, which can influence the incidence of PPCs [13]. By controlling these factors, we were able to attribute the differences in outcomes more directly to the intervention of preoperative IS, strengthening the internal validity of the study.
Role of Surgery Duration: The focus on midline laparotomies lasting more than 2 hours ensured that the patients selected for this study faced a higher risk of PPCs due to the prolonged duration of anesthesia and mechanical ventilation. Studies have shown that longer surgeries are associated with increased respiratory compromise postoperatively [8], making this population ideal for evaluating the benefits of IS. Our results confirm that preoperative IS can mitigate the additional respiratory risk associated with prolonged surgeries.
Secondary Outcomes - Mobilization and Pain: Early mobilization is another critical factor in reducing PPCs, as it encourages deep breathing and enhances lung expansion. In our study, patients in the intervention group achieved earlier ambulation, with a mean time to first mobilization of 28 hours compared to 36 hours in the control group. Early mobilization has been linked to better postoperative respiratory function, and the faster recovery of these patients underscores the role of IS in improving overall recovery [15].
Postoperative pain was also significantly lower in the intervention group, as evidenced by lower VAS scores at 48 and 72 hours postoperatively (Table 5) (Figure 4). Lower pain levels are likely due to improved lung function, which reduces the need for shallow breathing and allows patients to engage in more effective coughing and lung expansion exercises postoperatively [16].
Comparison with Literature: The results of our study align with findings from international research that underscores the benefits of IS in preventing PPCs. For instance, Sweity et al. (2021) found that preoperative IS significantly reduced PPCs in patients undergoing coronary artery bypass graft (CABG) surgery, a finding that parallels our results in the context of abdominal surgery [11]. While the surgical contexts differ, the consistency of these outcomes suggests that preoperative IS has a broad potential to improve pulmonary outcomes across various types of surgeries.
In contrast, some studies have reported mixed results regarding the efficacy of IS, particularly in lower-risk surgical populations. For example, Guimarães et al. (2009) and Thomas & McIntosh (1994) found limited benefits of IS in preventing PPCs in patients undergoing elective upper abdominal surgery, highlighting that the effectiveness of IS may be influenced by factors such as patient selection, type of surgery, and timing of intervention [17,18]. These findings suggest that while IS is beneficial, its impact may vary depending on how and when it is applied, and further research is needed to refine its use in different clinical settings.
In the context of Pakistan, where healthcare resources are often limited, simple and cost-effective interventions like IS could play a crucial role in improving surgical outcomes. A study by Malik et al. in a tertiary care hospital in Karachi reported a high incidence of PPCs following major gastrointestinal surgeries, attributing this to factors such as inadequate preoperative care and limited access to preventive measures like IS [19]. Our study provides evidence that preoperative IS could be a valuable tool in such settings, helping to reduce the burden of PPCs and associated healthcare costs.
Moreover, the reduction in hospital stay observed in our study has significant implications for healthcare systems, particularly in resource-constrained environments (Table 4). Shorter hospital stays not only reduce costs but also minimize the risk of hospital-acquired infections, which are a major concern in low- and middle-income countries [20]. The finding that preoperative IS can contribute to such outcomes highlights its potential as a low-cost intervention that can be easily integrated into standard care protocols.
Clinical implications: The clinical implications of our findings are substantial. Incorporating preoperative IS into routine preoperative care could lead to a significant reduction in PPCs, improved postoperative respiratory function, and shorter hospital stays. This is particularly relevant in settings like Pakistan, where optimizing resource use and improving surgical outcomes are critical goals. By reducing the incidence of PPCs, preoperative IS can also contribute to better overall recovery, allowing patients to resume normal activities more quickly and reducing the likelihood of long-term respiratory issues.
The observed reduction in postoperative pain scores in the intervention group also suggests that preoperative IS may enhance pain management. Effective pain control is crucial for encouraging early mobilization and deep breathing exercises postoperatively, both of which are key to preventing PPCs [21]. By providing a non-pharmacological approach to pain management, preoperative IS could reduce the reliance on opioids and other pain medications, which have their own set of risks and complications.
Strengths and limitations: One of the key strengths of this study is its randomized controlled design, which minimizes selection bias and allows for direct comparisons between the intervention and control groups. The use of a standardized surgical team and consistent anesthesia techniques across all patients strengthens the study’s internal validity, ensuring that observed differences are more likely due to IS intervention. Furthermore, the inclusion of specific criteria for PPCs and objective measures of oxygenation (PaO2 and SpO2) adds to the rigor of the study.
However, several limitations should be considered. First, the study was conducted at a single center with a relatively small sample size, which may limit the generalizability of the findings to other populations or healthcare settings. Second, compliance with the IS protocol was self-reported, which could introduce bias, although daily logs were reviewed by clinical staff. Third, while the study included midline laparotomies, the results may not be generalizable to all types of abdominal surgeries, especially those with shorter durations.
Future research: Future studies should aim to confirm these findings in larger, multi-center trials, with a focus on assessing the long-term pulmonary outcomes of preoperative IS. Additionally, future research should explore the role of IS in other types of abdominal surgeries and investigate whether shorter preoperative IS interventions (less than one week) can achieve similar benefits. Finally, the cost-effectiveness of preoperative IS in resource-limited settings should be explored, particularly in regions where surgical complications can have severe socioeconomic consequences.
Conclusion
This study demonstrates that preoperative incentive spirometry (IS) significantly reduces postoperative pulmonary complications (PPCs) in patients undergoing elective midline laparotomies lasting more than 2 hours. Preoperative IS not only lowers the incidence of PPCs but also improves postoperative oxygenation, shortens the length of hospital stay, reduces postoperative pain, and facilitates earlier mobilization. By controlling for key variables such as surgical and anesthesia teams and focusing on a higher-risk population undergoing longer surgeries, this study provides robust evidence of the effectiveness of preoperative IS. These findings suggest that incorporating IS into preoperative care protocols could lead to improved patient outcomes, particularly in resource-limited settings where surgical complications have significant implications for both patients and healthcare systems.
Given the simplicity, low cost, and non-invasive nature of IS, its routine use in preoperative care is recommended for patients undergoing major abdominal surgeries. Future research should focus on expanding the use of preoperative IS to other types of surgeries and evaluating its long-term impact on respiratory function and recovery.
Funding
No funding was available, the study was self financed by the principal author.
Conflicts of interest
The authors declare no conflicts of interest related to this research.
Acknowledgments
We would like to acknowledge students of Ameer ud Din Medical College for helping in data collection.
Author contributions
Dr Maham Arshad - Conceptualization, Data Curation, Writing – Original Draft, Methodology, Writing – Review & Editing, Formal Analysis, Visualization, Supervision
Dr Azka Ashraf - Methodology, Writing – Review & Editing
Dr Ghanwa Muzammil - Methodology, Writing – Review & Editing
Dr Rohma Arshad - Conceptualization, Data Curation, Writing – Original Draft
Dr Awais Amjad Malik - Formal Analysis, Visualization, Supervision
Dr Jehanzaib Rashid - Formal Analysis, Visualization, Supervision
Ethical Approval
This study was approved by the Ethical Committee of Lahore General Hospital (Department of Surgery) with Ref No:128/SU-III.
References
- Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth 118 (2017): 317-334.
- Miskovic A, Lumb AB. Postoperative pulmonary complications in thoracic surgery. Thorac Surg Clin 30 (2020): 299-307.
- Canet J, Gallart L. Predicting postoperative pulmonary complications in the general population. Eur Respir J 35 (2010): 1230-1236.
- Serejo LG, Da Silva-Junior FP, Bastos JP, et al. Risk factors for pulmonary complications after emergency abdominal surgery. Respir Med 101 (2007): 808-813.
- Freitas ER, Soares BG, Cardoso JR, et al. Incentive spirometry for preventing pulmonary complications after coronary artery bypass graft. Cochrane Database Syst Rev 9 (2012): CD004466.
- Hulzebos EH, Helders PJ, Faviú NJ, et al. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: A randomized clinical trial. JAMA 296 (2006): 1851-1857.
- Agostini P, Naidu B. Does preoperative physiotherapy reduce postoperative pulmonary complications in elective cardiac surgery? A systematic review. Eur J Cardiothorac Surg 43 (2013): 829-835.
- Yang CK, Yoo JW, Jo JY, et al. Incidence and risk factors of postoperative pulmonary complications in patients undergoing laparoscopic abdominal surgery. J Anesth 28 (2014): 667-673.
- Lawrence VA, Dhanda R, Hilsenbeck SG, et al. Risk of pulmonary complications after elective abdominal surgery. Chest 110 (1996): 744-750.
- Canet J, Mazo V. Postoperative pulmonary complications. Minerva Anestesiol 76 (2010): 138-143.
- Sweity EM, Alkaissi AA, Othman W, et al. Preoperative incentive spirometry for preventing postoperative pulmonary complications in patients undergoing coronary artery bypass graft surgery: a prospective, randomized controlled trial. J Cardiothorac Surg 16 (2021): 241.
- Agostini P, Singh S, Grant R, et al. Incentive spirometry and early mobilization reduce pulmonary complications after abdominal surgery: a randomized controlled trial. Ann Thorac Surg 95 (2013): 2020-2027.
- Lawrence VA, Cornell JE, Smetana GW. Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 144 (2006): 596-608.
- Shweiki E, Abougergi MS, Choi JJ, et al. Pulmonary complications in emergency general surgery: incidence, risk factors, and outcomes. Am J Surg 210 (2015): 892-898.
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78 (1997): 606-617.
- Overend TJ, Anderson CM, Lucy SD, et al. The effect of incentive spirometry on postoperative pulmonary complications: a systematic review. Chest 120 (2001): 971-978.
- Guimarães MM, El Dib R, Smith AF, et al. Incentive spirometry for prevention of postoperative pulmonary complications in upper abdominal surgery. Cochrane Database Syst Rev (2009): CD006058.
- Thomas JA, McIntosh JM. Are incentive spirometry, intermittent positive pressure breathing, and deep breathing exercises effective in the prevention of postoperative pulmonary complications after upper abdominal surgery? A systematic overview and meta-analysis. Phys Ther 74 (1994): 3-10.
- Malik AM, Laghari AA, Mallah Q, et al. Postoperative complications of major gastrointestinal surgery: a retrospective analysis. Med Channel 16 (2010): 101-105.
- Allegranzi B, Bagheri NS, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 377 (2011): 228-241.
- Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet 367 (2006): 1618-1625.





 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 