Giant Pelvic Sarcoma. A Challenge for the General Surgeon
Sánchez Martínez Gustavo Eduardo*, Szymanski Florencia Luis Ramón, Muñiz Calderón Mario Emmanuel, Juárez Mendoza Diana Sofía, Bermudez Ayala Julieta, De León Rosas Diego Andrés
General Surgery Department Hospital General, Dr. Carlos Canseco. Tampico, Tamaulipas, Mexico
*Corresponding Author: Gustavo Eduardo Sánchez Martínez, General Surgery Department Hospital General, Dr. Carlos Canseco. Tampico, Tamaulipas, Mexico
Received: 26 July 2024; Accepted: 05 August 2024; Published: 14 August 2024
Article Information
Citation: Sánchez Martínez Gustavo Eduardo, Szymanski Florencia Luis Ramón, Muñiz Calderón Mario Emmanuel, Juárez Mendoza Diana Sofía, Bermudez Ayala Julieta, De León Rosas Diego Andrés. Giant Pelvic Sarcoma. A Challenge for the General Surgeon. Case report. Journal of Surgery and Research. 7 (2024): 343-345
View / Download Pdf Share at FacebookAbstract
Pelvic sarcomas represent a rare group of tumors, which can be divided into 2 groups. Soft tissue sarcomas, including liposarcoma, leiomyosarcoma, gastrointestinal stromal tumors, malignant peripheral nerve sheath tumors, and solitary fibrous tumors. The most common bone sarcomas include osteosarcoma and chondrosarcoma.
Multidisciplinary treatment at a center experienced in the treatment of sarcoma is essential. Management is dictated by histologic type and grade. Surgical resection with wide margins is the cornerstone of treatment for pelvic sarcomas, although this is often challenging due to anatomic constraints of the pelvis. Multimodal treatment is critical due to the high risk of local recurrence in the pelvis.
Keywords
<p>Oncosurgery, Sarcoma, Emergency surgery, Laparotomy</p>
Article Details
Introduction and Importance
Uterine sarcomas comprise less than 1% of gynecologic malignancies and 2-5% of all uterine malignancies. These tumors arise from three types of tissue: Carcinosarcomas, which originate in the endometrium and account for 40-50% of all uterine sarcomas. Leiomyosarcomas, originating in the myometrium, peak in incidence at age 50, and comprise 30% of all uterine sarcomas. Sarcomas arising in the endometrial stroma have their peak incidence before menopause for low-grade tumors and after menopause for high-grade tumors, comprising 15% of all uterine sarcomas. These three distinct entities are often grouped under uterine sarcomas; however, each tumor type is currently studied in separate clinical trials.
The only documented etiological factor in 10% to 25% of these malignant neoplasms is a history of pelvic radiation, which was previously administered for benign uterine bleeding starting between 5 to 25 years prior. The rise in uterine sarcomas has been associated with the use of tamoxifen for breast cancer treatment. Subsequently, increases were also observed with tamoxifen administration for breast cancer prevention in women at increased risk, possibly due to the estrogenic effects of tamoxifen on the uterus. Because of this increase, patients receiving tamoxifen should undergo regular pelvic examinations and consider endometrial biopsy if they experience any abnormal uterine bleeding.
Case Presentation
42-year-old female patient. No history of chronic degenerative diseases or prior surgeries.
She reports symptoms starting one month ago, including abdominal distension followed by dyspnea and colicky pain localized in the epigastrium with radiation to the hypochondria in the dorsal region. She denies nausea, vomiting, or fever. She has experienced unintentional weight loss of 5 kilograms. She initially sought medical attention with a private physician due to dyspnea on moderate exertion, who started her on treatment with Furosemide tablets without improvement. Therefore, she decided to seek care at this facility.
Laboratory results show: WBC 18.6, Neutrophils 16.7, Lymphocytes 1.1, Hemoglobin 11.2, Hematocrit 36.4, Platelets 532, MPV 4.38. Urinalysis reports: amber color, turbid appearance, density 1.025, pH 5.5, negative glucose, 15 protein, 200 blood, 2-4 leukocytes, moderate epithelial cells, moderate uric acid crystals.
Abdominal ultrasound reveals a complete abdominopelvic mass, predominantly solid with vascular areas and necrotic cystic areas, exerting a significant mass effect on intra-abdominal organs. Consider infiltrative neoplastic process of adnexal origin, with the differential diagnosis favoring cystadenoma. No free intra-abdominal fluid or collections identified. Bilateral renal pelvicaliectasis present.
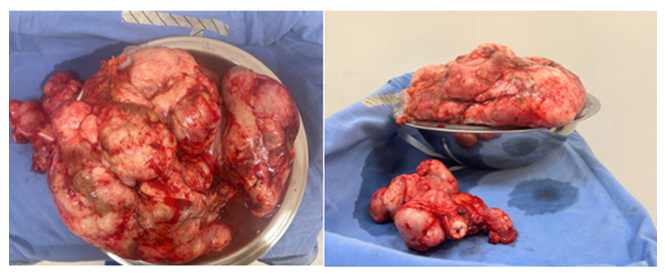
Tumor resection, hysterectomy, and bilateral oophorectomy were performed, dissecting layer by layer until reaching the cavity where a mass occupied almost the entire space. A peroral puncture was performed, extracting approximately 7 liters of fluid. Subsequently, the mass was dissected, revealing adhesions to the small intestine and sigmoid colon. The tumor's origin from the uterus was confirmed, and initially, partial tumor resection was performed, removing most of the tumor. Later, under direct vision, the remaining tumor was excised, necessitating bilateral oophorectomy.
Clinical Discussion
Pelvic extraperitoneal soft tissue sarcomas represent 18% of all cases. In this location, it is essential to assess the tumor's characteristics and its relationship with the multiple anatomical structures of the pelvis. Adequate surgical planning and accurate staging through abdominopelvic CT and/or pelvic MRI are necessary. Individualized surgery should be designed for each case since surgery forms the cornerstone of treatment, aiming to improve survival rates and reduce recurrence.
These sarcomas can pose a diagnostic challenge in early stages due to their location and the absence of specific symptoms, despite their often significant size. Diagnosis frequently occurs incidentally. Patients may experience general symptoms such as abdominal or lower back pain, which are commonly misattributed to more common causes. As the sarcoma grows, it may cause a palpable mass in the abdomen and more pronounced symptoms such as unexplained weight loss, fatigue, and fever. In advanced cases, it can affect adjacent organs, leading to additional symptoms.
Methods
This case report has been reported in line with the SCARE Criteria.
Conclusion
Uterine sarcomas are a group of rare, heterogeneous, and aggressive uterine neoplasms that frequently metastasize distantly, leading to a lower survival rate compared to other uterine malignancies. Total abdominal hysterectomy with bilateral salpingo-oophorectomy is the treatment of choice as it provides accurate staging and allows for pathological evaluation of prognostic factors, identifying high-risk patients who may benefit from adjuvant therapies and potentially curative treatment, especially in early stages of the disease.
For mixed mesodermal tumors, due to a high incidence of positive peritoneal cytology, adnexal, peritoneal, and nodal metastases, surgical treatment should include peritoneal lavage, omentectomy, and primarily pelvic lymphadenectomy.
In cases of uterine leiomyosarcomas, which have a low incidence of nodal and adnexal metastases and positive peritoneal cytology, nodal sampling is not indicated for patients with macroscopically confined disease to the uterus, but rather consideration of biopsy for clinically suspicious lymph nodes. Routine re-operation solely for nodal assessment is not recommended. Due to the low incidence of microscopic ovarian metastases and uncertain benefit of oophorectomy, routine bilateral salpingo-oophorectomy is not recommended for premenopausal patients wishing to preserve ovarian function. In postmenopausal women undergoing hysterectomy, ovarian preservation should not be recommended for those requiring the procedure.
Chemotherapy options for uterine sarcoma are limited by the lack of adequately designed controlled studies. Palliative chemotherapy may be considered for patients with medically inoperable, advanced, or recurrent disease who are symptomatic, selected based on overall health status, associated comorbidities, and age.
Sources of funding
This study did not receive any specific support from funding agencies, in the public, commercial or non-profit sector.
Conflict of interest
The authors declare that they have no conflict of interest in the writing of this manuscript.
Ethical considerations
Confidentiality of data: The authors state that they have followed their workplace protocols on the publication of patient data.
Protection of people and animals: The authors state that no experiments have been carried out on humans or animals for this research.
Right to privacy and informed consent
The authors declare that no patient data appears in this article.
Acknowledge
The authors acknowledge all the staff of the Honorable General Hospital Dr. Carlos Canseco in Puerto de Tampico, Tamaulipas and honorable Dr. Benigno Piña Rodriguez oncosurgeon.
Authors contribution
Gustavo Eduardo Sanchez-Martinez: Patient care, clinical case, writing
Diana Sofía Juárez-Mendoza: Translation.
References
- Vargas HVM, Hernández RA, Jiménez Villanueva x Sarcoma de útero en Vargas-Hernández VM. Cáncer en la Mujer 1ª. Ed. Edit. Alfil 2011 México 12 (2011): 1039-1042
- Asencio PJM, Fernandez HJA, Blanco FG, et al. Actualización en el manejo de sarcomas retroperitoneales y pélvicos; el papel de la cirugía compartimental. Cir Esp 97 (2019): 480-488.
- PDQ database. Uterine sarcoma. Bethesda, Md: National Cancer Institute (2012).
- Vargas Hernández VM, Hernández Rubio A, Jiménez Villanueva x Sarcoma de útero en Vargas-Hernández VM. Cáncer en la Mujer 1ª. Ed. Edit. Alfil México (2011): pp.1039-1046.
- Hardisson D. Patología de los sarcomas uterinos (2024).
- Tratamiento del sarcoma uterino (PDQ®) [Internet]. Cancer.gov (2024).
- Sampath S, Schultheiss TE, Ryu JK, et al. The role of adjuvant radiation in uterine sarcomas. Int J Radiat Oncol Biol Phys 76 (2010): 728-734.
- Fletcher CDM, Bridge JA, Hogendoorn PCW, et al. WHO classification of tumours of soft tissue and bone. (4th edtn). Lyon, France: IARC (2013): 10-11.
- Mullen JJ, Houdt WY. Soft tissue of the pelvis: Technical and histological considerations. J.Surg Oncol 117 (2018): 48-55.
- Horn LC, Schierle K, Schmidt D, et al. Current TNM/FIGO classification for cervical and endometrial cancer as well as malignant mixed müllerian tumors. Facts and background. Pathologe 32 (2011): 239-243.
- National Comprehensive Cancer Network. Uterine Neoplasms (2014).



 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 