Acute Obstructive Anural after an Allograft Kidney Biopsy: An Unusual Complication
Rida Touab1,*, Youness Khdach2, Mohammed R Andaloussi1, Larbi Hamdoune2, Abderrahmene Elwali1, Mustapha Bensghir1
1Department of anesthesiology and critical care, Military Training Hospital Mohamed V, Rabat, Morocco
2Department of urology, Military Training Hospital Mohamed V, Rabat, Morocco
*Corresponding Author: Dr Rida Touab, Department of anesthesiology and critical care, military training hospital Mohamed V, Rabat, Morocco
Received: 11 January 2021; Accepted: 20 January 2021; Published: 27 January 2021
Article Information
Citation: Rida Touab, Youness Khdach, Mohammed R Andaloussi, Larbi Hamdoune, Abderrahmene Elwali, Mustapha Bensghir. Acute Obstructive Anural after an Allograft Kidney Biopsy: An Unusual Complication. Journal of Surgery and Research 4 (2021): 35-38.
View / Download Pdf Share at FacebookAbstract
Introduction: The hemorrhagic complications after percutaneous kidney biopsy are known, and patients are informed below procedure. In our observation, we describe an unusual evolution of hematuria post allograft kidney biopsy.
Case report: 45-year-old patient, hospitalized for acute renal failure. He had a history of left renal allograft. Kideney biopsy was formed in order to find an etiology, complicated by hematuria and bladder hematoma. The last one had causing an obstructive anuria with worsening in the kidney function. A success endoscopic resection of hematoma was performed following by favorable evolution.
Conclusion: We describe a therapeutic option for bladder hematoma secondary to kidney biopsy.
Keywords
<p>Allograft; Biopsy; Bladder; Hematoma</p>
Article Details
1. Introduction
Kidney biopsy is a diagnostic and prognostic procedure that has been used for more than fifty years [1]. It is a gold standard in diagnosis of multiples kidney disorders [2], and plays an important role in clinical research [3]. The hemorrhagic complications after percutaneous kidney biopsy are known, and patients are informed below procedure. The aim of our observation is describing an unusual evolution of hematuria post allograft kidney biopsy inducing an obstructive anuria and the therapeutic options.
2. Case Report
45-year-old patient, hospitalized for acute renal failure. He had a history of left renal allograft for 11 years under mecophenolate mophetil, following chronic renal failure dialysis of unknown etiology. The patient presented an asymptomatic deterioration of his biological renal function revealed on a check-up, hence his hospitalization for exploration. The physical examination found a pale patient, with arterial hypertension at 175/95 mmHg, slightly tachycardic at 105 beats per minute with a functional systolic murmur, eupneic, presenting a pulsed saturation at 98% without oxygen, with a soft abdomen seat of lumbotomy scar, the urinary strip objected a leukocyturia, with proteinuria.
The biologic workup showed blood creatinine at 112 mg/l, urea at 1.09 g/l, alkaline reserves at 12mmol/l, a correct blood ionogram, normocytic normochromic anemia at 8 g/dl, a correct haemostasis workup: platelet level at 305 G/l, prothrombin level at 75% and activated partial thromboplastin time ratio at 1. The urine culture was sterile and the renal ultrasound was normal. The patient was treated with hydration and dual antihypertensive therapy including a calcium channel blocker and alpha methyl dopa.
A ultrasound guided percutaneous biopsy was performed after one week of admission, complicated by a macroscopic hematuria, hence the insertion of a bladder catheter with irrigation, a reservation of labile blood products and a biological assessment which confirmed correct hemostasis and a worsening of the anemia to 7 g/dl. 6 hours after the procedure, the patient is anuric with the need to unblock several times. At H 12 a worsening of the biological renal insufficiency was noted with creatinine at 134 mg/l, and a reno-vesical ultrasound showed a large intra-bladder haematoma taking almost all the bladder, without any abnormality on the renal graft at the site of the biopsy, hence the decision to carry out an endoscopic resection of the haematoma.
The pre-anaesthetic evaluation found an ASA 3u patient who was hemodynamically and respiratory stable, conscious, unalgesic, with signs of anemia. The course was from his admission to the emergency room in an aseptic room, with a second 16 gauge peripheral venous line, monitoring, antibiotic prophylaxis with cefazolin 2 g slow intravenous, spinal anesthesia with 10 mg of bupivacaine and 25 ug of fentanyl, without hypotension, with the start of a transfusion of two phenotypically leukocyte-depleted red blood cell concentrates.
After installation in the lithotomy position, endoscopic exploration revealed a coagulated hematoma of pseudotumoral appearance filling the entire bladder, with resection by monopolar catheter using 15 liters of glucocolla and bladder lavage with saline (Figure 1).
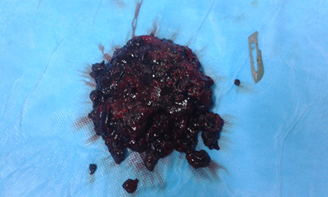
Figure 1: hematoma after resection.
Resection of the entire hematoma was achieved after 60 min, with irrigation catheterization and monitoring. The evolution was favourable with the resumption of a clear correct diuresis, and improvement of the blood creatinine level.
3. Discussion
Kidney biopsy is necessary for the diagnosis and evaluation of renal pathologies, it is burdened with low morbidity, including haemorrhagic complications which are rarely serious [5] requiring blood transfusion in 1% of cases and recourse to interventional angiography in 0.6% of cases in outpatients [5] removed to 8% and 2% respectively in inpatients [6] due to greater severity and risk factors. An objective Japanese cohort found an incidence of macroscopic hematuria of 3.1%, need for transfusion 0.7%, arterial embolization 0.2%, and death attributed to biopsy of 0.006% [4]. 90% of these hemorrhagic complications occur within 24 hours of biopsy [7, 8]. Risk factors have been identified such as high urea levels, thrombocytopenia or anemia [5].
In our case, hematuria was abundant to form total bladder hematoma compressing the ureters, leading to worsening of obstructive renal failure, a situation not described in the cohorts evaluating the safety and complications of percutaneous renal biopsy for either native or allograft kidneys. Compressive bladder haematoma has been reported in literature secondary to neoplastic [9] or infectious disease [10].
The therapeutic option was transurethral resection of the hematoma, which was effective and safe since other means including irrigation was not effective and performing a nephrostomy to remove the obstacle is only a waiting solution, even if it carries a significant risk. Pharmacological means such as in situ thrombolysis were contraindicated in our situation.
4. Conclusion
Endoscopic resection of bladder hematoma complicating an allograft kidney biopsy can save renal function.
Conflicts of Interest
All authors declare no conflicts of interest.
References
- Melissa Schorr, Pavel S Roshanov, Matthew A Weir, Andrew A. House, Frequency, Timing, and Prediction of Major Bleeding Complications From Percutaneous Renal Biopsy Canadian Journal of Kidney Health and Disease Volume 7: 1-10.
- Waikar SS, McMahonGM. Expanding the role for kidney biopsies in acute kidney injury. Semin Nephrol 38 (2018): 12-20.
- National Institute of Diabetes and Digestive and Kidney Diseases: Kidney precision medicine project (2016).
- Akehiko Kawaguchi, Tasuku Nagasawsa, Kazuhiko Tsuruya, Kenichiro Miura, Takayuki Katsuno,et al. A nationwide survey on clinical practice patterns and bleeding complications of percutaneous native kidney biopsy in Japan; Clinical and Experimental Nephrology 24 (2020): 389-401.
- Corapi KM, Chen JL, Balk EM, Gordon CE. Bleeding complications of native kidney biopsy: A systematic review and metaanalysis. Am J Kidney Dis 60 (2012): 62-73.
- Dennis G Moledina, Randy L Luciano, Lidiya Kukova, Lili Chan, Aparna Saha, et al. Kidney Biopsy-Related Complications in Hospitalized Patients with Acute Kidney Disease, Clin J Am Soc Nephrol 13 (2018): ccc-ccc.
- Whittier WL, Korbet SM. Timing of complications in percutaneous renal biopsy. J Am Soc Nephrol 15 (2004): 142-147.
- Simard-Meilleur MC, Troyanov S, Roy L. Risk factors and timing of native kidney biopsy complications. Nephron Extra 4 (2014): 42-49.
- Anurag Jain, Abhishek Mahato, Mattakarotu Joseph Jacob, Madan Gopal Vishnoi, Aniruddha Govind Pandit, et al. Hematoma in Urinary Bladder Masqueradin g as Neoplastic Mass Indian J Nucl Med 33 (2018): 253-254.
- Ing-Luen Shyu, Peng-Hui Wang, Ben-Shian Huang. A large bladder hematoma resulting from infectious hemorrhagic cystitis after pelvic reconstruction with transvaginal mesh: An unusual complication SAGE Open Medical Case Reports 7 (2019): 1-4.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 