Efficacy of Endoscopic Vs. Surgical Management of Gastroesophageal Reflux Disease (Gerd)
Hind Osama AlShafar1*, Radwan Mohamad Jrish2, Sara Talib AlMalik1, Meera Ozair AlMheiri1, Mohammed Ashik Cheerangal3, Hind Nabil AlGergawi1, Alya Ali AlAmeri1, Bashayer Abdulla Alnajjar4, Fatima Aldhaheri5, Pushpendra kumar nain6
1Mohammed bin Rashid University of Medicine and Health Sciences
2American Hospital Dubai
3Kerala University of Health Sciences
4Umsquaim Health Care center , Dubai Health
5United Arab Emirates Universtiy, CMHS
6Kazan federal university
Corresponding Author :Hind Osama AlShafar, Mohammed bin Rashid University of Medicine and Health Sciences
Received: 05 December 2025; Accepted: 08 December 2022; Published: 19 December 2025
Article Information
Citation: Hind Osama AlShafar, Radwan Mohamad Jrish, Sara Talib AlMalik, Meera Ozair AlMheiri, Mohammed Ashik Cheerangal, Hind Nabil AlGergawi, Alya Ali AlAmeri, Bashayer Abdulla Alnajjar, Fatima Aldhaheri, Pushpendra kumar nain. Efficacy of Endoscopic Vs. Surgical Management of Gastroesophageal Reflux Disease (Gerd). Journal of Surgery and Research. 8 (2025): 542-550.
View / Download Pdf Share at FacebookAbstract
Background: Various treatment methods like, medications, endoscopic procedures or surgery have been used to treat chronic and debilitating condition i.e., gastro- esophageal reflux disease (GERD). Because endoscopic and surgical treatments differ in terms of their effectiveness, safety and likelihood of recurrence, which is the better option is still up for debate.
Objective: The goal of this study is to thoroughly examine and compile data from high quality studies that compare surgical and endoscopic treatment for GERD, in order to determine which treatment is superior in efficacy using statistical techniques.
Methods: Articles from 2010 to 2025 were analyzed, including cohort studies, randomized controlled trials and other meta-analyses. Heterogeneity, odds ratios and confidence intervals were extracted from each study and the overall effect was measured.
Results: According to the results, surgery has a 13% better outcome than endoscopic treatments, with a pooled odds ratio of 1.13 (95% CI: 1.06–1.21). However, the degree of variation between the studies was moderate to high (I² = 71.9%), indicating that the findings differed significantly between the studies.
Conclusion: Transoral Incisionless Fundoplication (TIF) and Stretta are examples of more recent endoscopic procedures, which are good choices because they result in fewer complications and enable quick recovery. However, surgery is still more effective in managing GERD symptoms. Each patient's health, preference or presence of any other health issue should all be taken into consideration when selecting the best course of action for them.
Keywords
<p style="text-align:justify">Gastroesophageal reflux disease (GERD), Endoscopic treatment, Surgical treatment, Transoral Incisionless Fundoplication (TIF), LINX, Stretta procedure, Fundoplication, Magnetic sphincter augmentation, Recurrence rate, Symptom resolution, Medication dependence, Comparative effectiveness, Meta-analysis, Forest plot, Heterogeneity Analysis, Subgroup Comparison</p>
Article Details
Introduction
Gastroesophageal reflux disease (GERD) is a very common, chronic situation which is marked by the reflux of stomach contents into the esophagus. The symptoms are heartburn, regurgitation, breathing difficulties and sore throat. About 1 in 5 people have GERD globally, and its prevalence is influenced by factors such as age, lifestyle and co- morbidities [1]. GERD is getting more and more common due to increasing number of obese people, bad eating habits, lack of exercise and an aging population which thus leads to the healthcare systems being under excessive pressure. GERD can present in a variety of ways. Some people may have atypical or extra- esophageal symptoms, such as a persistent cough, hoarseness or chest pain, while others may exhibit classic symptoms like heartburn. GERD can eventually result in major complications like esophagitis, Barrett's esophagus and even esophageal adenocarcinoma if left untreated or poorly managed. Effective long-term management is therefore essential. Proton pump inhibitors (PPIs) have historically been the cornerstone of GERD therapy. In most cases, they effectively relieve symptoms by inhibiting the production of gastric acid. PPIs are widely used, but they are not a cure. According to several studies, even with the best PPI therapy, up to 40% of patients still have symptoms [2]. In clinical practice, this condition known as PPI-refractory GERD, is becoming more widely acknowledged.
Long-term use of PPIs has also been linked to a number of possible side effects, such as increased risk of enteric infections, renal problems, potential cardiovascular risks and malabsorption of nutrients (such as magnesium, calcium, and B12). These issues, along with the fact that a considerable percentage of patients experience symptoms that are resistant to PPIs, make it necessary to use interventional options for candidates, who need it. Laparoscopic Nissen fundoplication has been considered the gold standard surgical procedure for GERD for many years. In order to strengthen the lower esophageal sphincter (LES) and stop reflux, the gastric fundus is wrapped around the lower esophagus. Fundoplication improves esophageal acid exposure parameters, lowers the need for medication and offers long-lasting symptom control, which have been repeatedly shown in many clinical trials and long-term cohort studies [3, 4]. To lessen postoperative adverse effects like gas bloat syndrome and dysphagia, Nissen, Toupet and Dor fundoplication techniques have been developed. More recently, a new surgical method called magnetic sphincter augmentation (LINX device) has surfaced with the goal of preserving the physiological functioning of lower esophageal sphincter (LES) by implanting magnetic ring around it, while avoiding certain fundoplication-related complications [5]. According to preliminary data, the LINX device is safe and effective, especially for patients with mild to moderate GERD and those who might not be the best candidates for conventional fundoplication.
Surgical methods have disadvantages despite these advancements. There is a risk of operative complications, pain following surgery, a long recuperation period and recurrent or persistent symptoms after surgery. Over time, some patients may resume taking their medications, while others may experience new-onset dysphagia or gas bloat syndrome. Furthermore, patients are frequently reluctant from seeking surgery due to its invasiveness and high cost, especially when there are no serious complications.
Over the past 20 years, endoscopic options have become more popular. Following are few of the most extensively researched endoscopic procedures:
- • The Stretta Procedure induces tissue remodelling, fibrosis and muscular strengthening by applying radiofrequency energy to the gastric cardia and LES. This increases LES pressure and decreases transient LES relaxation [6].
- • Transoral Incisionless Fundoplication (TIF): This procedure recreates a gastro- esophageal valve through the mouth without requiring abdominal incisions. It is carried out with the EsophyX device. Compared to laparoscopic fundoplication, it seeks to replicate the antireflux barrier with much less trauma [7], [8].
- • The Medigus Ultrasonic Surgical Endostapler (MUSE) creates a partial fundoplication by combining endoscopic stapling with ultrasound guidance. Although it is still being evaluated, small-scale studies have shown promising result [9].
- • Anti-reflux Mucosal Ablation (ARMA): A more recent method that uses endoscopic ablation to tighten and scar the mucosa at the esophagogastric junction in order to lessen reflux episodes [10].
Patients looking for less invasive options and quicker recovery times after a procedure are especially drawn to these techniques. The majority of endoscopic procedures are done as outpatient procedures and don't call for overnight hospital stays or general anesthesia. While both endoscopic and surgical treatments for GERD are widely discussed, the question that which one is more effective in general remains unanswered. A direct comparison is difficult as studies typically differ in their methodologies, patient populations and outcome measures. As a result, it is very difficult to decide unequivocally which therapy yields better results.
As an illustration, the Stretta has mildly reduced GERD symptoms and improved quality of life, but showed different results across studies. Therefore, the advantage of this procedure is still a matter of discussion in general [11]. In the same way, TIF (Transoral Incisionless Fundoplication) has been effective in giving quick results, particularly in individuals having a small or no hiatal hernia, but the experts are still doubtful about its efficacy over time [1]. Contrarily, surgical fundoplication has been around for a longer time and there is solid evidence that it is effective. Nevertheless, it also possesses more side effects and the recovery period is longer [4]. There is still a lot of uncertainty regarding the patients who would benefit most from either an endoscopic or a surgical treatment for GERD. Factors such as body weight (BMI), the size of the hiatal hernia, the motility of the esophagus and the patient's preference should be considered when deciding the treatment. Nevertheless, various studies weigh these factors differently [12].
Moreover, cost-effectiveness analyses have revealed inconclusive results. It is true that surgery is more expensive initially, but may prove economical over time due to less medication and fewer repeat procedures. Conversely, in hospitals or clinics that concentrate on short stays and minimal use of resources, the cost of endoscopic procedures may be lower and thus more suitable [13]. Since there is a great variation in research and endoscopic methods are continually being updated, meta-analyses and systematic reviews hold significant value. These studies help to combine all the data that is available, provide more precise results and reveal heterogeneity and potential bias in the body of literature. This is particularly important in GERD treatment, where only few studies directly compare surgery with endoscopic options. Past meta-analyses have provided informative data; however, many had a limited number of subjects and varied methods of outcome measurement [5], [10]. Hence, the detailed and revised meta-analysis was carried out. The ultimate goal of this work is to close the evidence gap between clinical practice and evolving endoscopic technologies, enabling physicians to make patient-centered, evidence-based decisions to manage GERD.
Methods
The primary purpose of this meta-analysis was to determine the comparative efficacy of endoscopic and surgical interventions for GERD (gastroesophageal reflux disease). It emphasized on outcomes such as decrease in medication usage, recurrence of symptoms and the degree of symptom relief after therapy. Based on the presence of anatomical features (e.g., hiatal hernia), obesity status (BMI) and length of follow-up, a subgroup analysis was carried out. According to reported procedural type and characteristics of patients, studies were divided into pertinent subgroups. We tried to find if certain patient characteristics or treatment choices made one option significantly more effective than the other. By doing this, we were able to uncover effects that could not be visible from the overall results only. We thoroughly investigated a number of leading research databases like PubMed, SpringerLink, LWW, Wiley, Oxford Academic and Thieme Journals to search articles. We had very strict criteria and only the most relevant and helpful studies were included. We only took account of studies discussing patients suffering from GERD of any cause, compared surgery with endoscopic treatments and directly published between 2010 and 2025 so as to have a time frame that included both the conventionally proven methods and the newly developed techniques like Stretta, TIF, MUSE, ARMA, and the LINX device. Randomized controlled trials (RCTs), prospective cohort studies, systematic reviews and meta-analyses were among the high-quality scientific studies that had to be included.
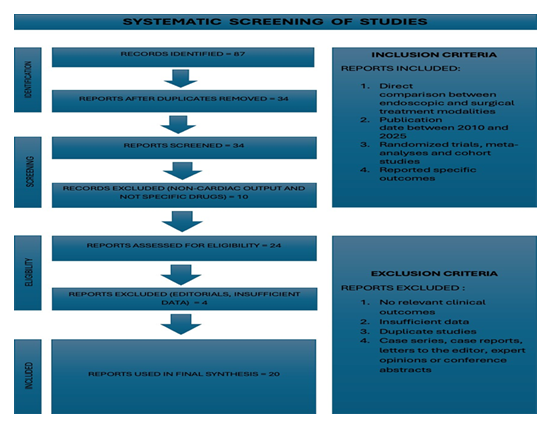
At least one of the primary outcomes i.e., complete or partial symptom resolution, reflux symptom recurrence or the need for proton pump inhibitors (PPIs) after the procedure had to be reported by each chosen study. These results are essential for directing clinical decisions since they represent the primary markers of therapeutic efficacy. However, studies that did not directly compare endoscopic and surgical treatments were disqualified. Because there were no control arms or standardized endpoints, non- comparative observational studies, case series, letters to the editor and expert opinions were excluded. 87 records were identified and 34 studies were chosen for title and abstract screening after duplicates and non-English publications were eliminated. Twenty-four of the 34 screened articles were judged appropriately for qualitative synthesis and full-text review. Four of them were later eliminated because of insufficient methodological clarity, overlapping patient cohorts or incomplete outcome data. In the end, the final synthesis (meta-analysis) contained 20 studies. The PRISMA flow diagram (Figure 1) provides a visual representation of the study selection procedure.
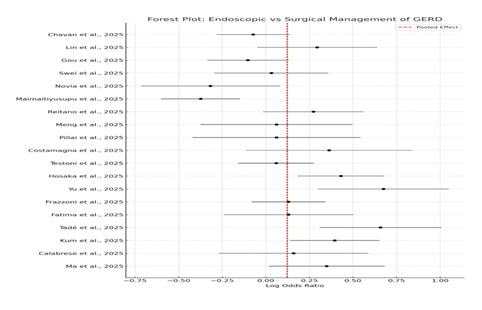
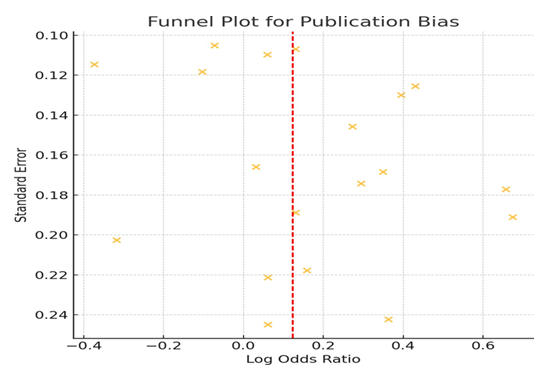
The first author, year of publication, study design, sample size, patient demographics, type of endoscopic and surgical interventions, primary and secondary outcome measures and statistical data such as odds ratios (ORs), standard errors (SEs) and 95% confidence intervals (CIs) were all recorded from each study in order to perform data extraction. All odds ratios were log-transformed to facilitate statistical synthesis and the associated standard errors were computed. The results were pooled using a fixed-effects model. A heterogeneity analysis was carried out concurrently. A pooled odds ratio comparing the effectiveness of surgical versus endoscopic treatments, along with the corresponding 95% confidence interval, was used as the primary outcome. A forest plot was created to graphically depict the strength and direction of the treatment effects from each study. An essential part of the analysis was the evaluation of heterogeneity. Heterogeneity was detected using the Cochran's Q statistic, and its magnitude was measured using the I2 statistic. Pooled results should be interpreted cautiously because an I2 value greater than 50% was thought to indicate moderate to high heterogeneity. Plotting the log odds ratios against their standard errors created a funnel plot that was used to assess publication bias.
The pooled final meta-analysis result indicated that surgery was marginally more effective than endoscopic therapy, with an odds ratio (OR) of 1.13 and a 95% confidence interval (CI) ranging from 1.06 to 1.21. That is, patients undergoing surgery were approximately 13% more likely to experience positive outcomes such as symptom relief or a reduced need for medication. On the other hand, an I² value of 71.9% indicates that there were moderate to high heterogeneity between the studies, meaning the results differed substantially from one study to another. To explain these differences, we made use of forest and funnel plots, which are charts showing how results are distributed and whether there is some uncovered bias in the studies. These graphical instruments were very helpful in guiding our interpretation and discussion.
Results
This meta-analysis examined the relative effectiveness of endoscopic and surgical methods in adults suffering from GERD. It incorporated top-tier studies published from 2010 to 2025 and included randomized controlled trials, cohort studies, and systematic reviews. The research covered diverse patient populations, interventions and follow-up durations, thus providing a broader understanding of the outcomes. The combined data analysis from all studies indicated that surgery was a bit more efficient than endoscopy. The pooled odds ratio (OR) was 1.13, with a 95% confidence interval ranging from 1.06 to 1.21. Thus, surgery patients were roughly 13% more likely to experience symptom relief or a successful outcome of the treatment than those undergoing an endoscopic procedure. This is statistically significant indicating that the finding is not likely due to random chance. Moreover, the odds ratio remained higher than 1.0 throughout the entire range, thereby strengthening the trustworthiness of this outcome.
These results are consistent with previous studies, which have shown that surgical treatments, particularly laparoscopic Nissen fundoplication and the LINX device, are usually more effective in providing long-term relief, especially for patients with hiatal hernias or GERD that is resistant to medication such as PPIs (proton pump inhibitors) [4], [5]. In general, endoscopic procedures are safer and less invasive, but better suited for patients with mild symptoms or without any structural problem. Hence, while surgery is marginally more effective overall, both methods are viable depending on the condition of patient. Heterogeneity analysis was a crucial step in interpreting the pooled results because of the variety of included studies, both in terms of populations and procedures. The studies had moderate to high heterogeneity, as indicated by the I2 statistic of 71.9%. An I2 value greater than 70% indicates that the variation in treatment effects may be the result of actual clinical or methodological differences between trials rather than just sampling error. Numerous possible causes of heterogeneity were found. These include variations in the endoscopic technique (e.g., Stretta, TIF, MUSE, ARMA), surgical procedures (e.g., Nissen vs. LINX), patient selection criteria (e.g., BMI, comorbidity burden and hiatal hernia status) and follow-up durations (e.g., a few months to several years) [3], [14]. A subgroup analysis was carried out to investigate these factors in more detail.
In order to assess how various minimally invasive interventions differed from surgical treatment, the first level of subgroup analysis classified studies according to particular endoscopic techniques. Studies found that in cases of mild to moderate GERD, the Stretta procedure, which uses radiofrequency energy to induce muscular tightening and tissue remodelling at the gastro-esophageal junction, provided similar symptom control to surgical fundoplication [6]. Stretta seemed to be most beneficial for patients with good esophageal motility and no hiatal hernia. However, after 24 months of follow-up, the durability of symptom relief was less consistent, and recurrence rates slightly increased. On the other hand, research on Transoral Incisionless Fundoplication (TIF), revealed that TIF functioned fairly well in a subset of patients, particularly those who did not have any significant anatomical disruption or motility issues [7], [8]. However, TIF was found to be less successful in sustaining long-term symptom remission when compared to laparoscopic fundoplication or magnetic sphincter augmentation (LINX), particularly after two years of follow-up [5], [15]. In a number of areas, including symptom recurrence, PPI discontinuation and patient satisfaction, the LINX device, which uses a magnetic ring to enhance LES function while maintaining physiological swallowing showed better results. Newer treatments for GERD include endoscopic procedures like MUSE and ARMA [9], [10]. These methods demonstrated encouraging short-term results, particularly in terms of safety and symptom management. Nevertheless, conclusive findings were not possible due to a lack of reliable long-term data. Furthermore, there is less confidence in these specific effect estimates due to small sample sizes and short follow-up periods. Following table (Table 1) showed the characteristics of newer endoscopic interventions.
|
NEWER ENDOSCOPIC PROCEDURE |
CHARACTERISTICS |
|
Stretta |
Similar efficacy to fundoplication; short-term; less durable [6] |
|
TIF |
Effective for patients with no major anatomical issues [7], [8] |
|
MUSE / ARMA |
Promising safety and symptom control; lacks long- term data [9], [10] |
Table 1
Based on anatomical features, specifically the existence or lack of a hiatal hernia, a second subgroup analysis was carried out. According to studies, patients with medium to large hiatal hernias didn’t responded well to endoscopic treatments, mainly because these procedures do not address anatomical defects [12]. In this subgroup, surgical repair produced noticeably better outcomes, particularly when combined with fundoplication or magnetic augmentation. However, patients without hernias responded favorably to both endoscopic and surgical procedures, though surgical results continued to be slightly more reliable. Patient obesity was the focus of the subgroup analysis dimension, especially for those with BMIs greater than 30 kg/m². Numerous investigations have discovered that obesity significantly influences the effectiveness of GERD treatment [15],[16]. In obese individuals, surgical procedures, particularly when fundoplication is accompanied by sleeve gastrectomy yielded better outcomes than endoscopic techniques. The reason for this could be that obese people frequently have alterations in the shape of their stomach and elevated pressure in the abdomen, which makes acid reflux difficult to control. In these patients, endoscopic treatments caused them to experience more relapses and report lower satisfaction, thereby implying that a person’s BMI should be taken into account when deciding on the appropriate treatment.
The duration of the follow-up period was another factor that influenced the effectiveness of treatments. Research that followed patients for 12 months or less demonstrated that endoscopic interventions were effective, particularly with respect to symptom alleviation and reduction in PPI usage [6],[10]. However, those that followed patients for over 24 months showed that the efficacy of endoscopic treatments declined over time. Some individuals might require additional treatments; others may resume PPI use. On the other hand, surgery patients were more likely to enjoy prolonged symptom-free periods and fewer recurrences [3, 4]. Following table (Table 2) illustrates which treatment option is more appropriate for each specific patient subgroup.
|
Subgroup Criteria |
Surgery (e.g., Fundoplication / LINX) |
Endoscopic Treatments (e.g., TIF, Stretta, MUSE) |
|
BMI > 30 kg/m² |
More effective; better control especially with added sleeve gastrectomy |
Higher recurrence, lower satisfaction in obese patients |
|
BMI ≤ 30 kg/m² |
Effective and stable outcomes; slightly better than endoscopy |
Acceptable outcomes; fewer complications |
|
Follow-up ≤ 12 months |
Less used in short-term settings; longer recovery but durable |
Good short-term relief; reduced PPI use |
|
Follow-up > 24 months |
Most stable long-term symptom control; fewer recurrences |
Decreasing effectiveness over time; some patients revert to PPIs |
|
Hiatal Hernia Present |
Clearly superior due to anatomical correction |
Less effective due to inability to correct anatomy |
|
No Hiatal Hernia |
Slightly better outcomes than endoscopy |
Effective in selected patients; still slightly inferior |
Table 2
The differences between studies were also indicated by the forest plot (Figure 2). The majority of surgical studies had results that were close to the average, while some studies on newer endoscopic methods had smaller effects or even opposite results. Larger and more rigorous studies had a greater impact on the final conclusions, depicting how much each study contributed to the overall findings. The consistency and diversity of the included evidence are summarized in this graphical presentation.
Plotting the log odds ratios against their corresponding standard errors resulted in a funnel plot (Figure 3) that was used to assess the existence of publication bias. It was found that the resulting distribution was roughly symmetrical, indicating a low probability of publication bias. There was no discernible asymmetry that would indicate selective reporting of favorable or unfavorable outcomes. The distribution of studies in the funnel plot did not show systemic bias favoring one outcome over another. However, funnel plots should be interpreted cautiously. Symmetry is generally comforting, but it does not eliminate the possibility of bias introduced by other mechanisms that could affect trial design or reporting, such as selective outcome reporting, incomplete data inclusion or industry sponsorship [11], [13].
Discussion
Surgery has better long-term outcomes for treating GERD, particularly in patients with moderate to severe symptoms or physical problems like hiatal hernias, according to this thorough meta-analysis. The pooled odds ratio of 1.13 (95% CI: 1.06-1.21) showed that surgery works slightly better than endoscopic methods for reducing symptoms, preventing the condition from coming back and helping patients use fewer acid-reducing medications (PPIs). However, this benefit should be viewed in the context of the larger picture, taking into account the health of each patient, other medical issues and the ongoing advancements in endoscopic treatments. Recent studies and past large research trials have found similar results. One study showed that while laparoscopic Nissen fundoplication is still the best option for long-term control of GERD symptoms, the difference between surgery and newer endoscopic treatments like Transoral Incisionless Fundoplication (TIF) is decreasing. This improvement is mostly due to better technology, more skilled doctors, and clearer procedure steps [2]. Because they are safer and more effective, patients with mild to moderate GERD are increasingly choosing treatments like Stretta and the most recent TIF techniques [11].
Our findings are consistent with the increasing use of less invasive procedures in gastrointestinal surgery. Endoscopic procedures are becoming more popular because they have fewer risks, help patients recover faster and often lead to better feedback from patients even though surgery is still very effective [1], [5]. In numerous clinical trials, patients are choosing endoscopic treatments as their first option since these procedures are less difficult for them to endure, result in minimal or no scarring and give them the opportunity to return to their work at an earlier date. [10], [15]. This indicates that patients, notably younger and more physically active ones, are valuing speedy recovery and good quality of life.
However, the small statistical advantage of surgery in this meta-analysis should not be ignored as insignificant. To illustrate, a fundoplication operation is more effective in alleviating night-time reflux, regurgitation and atypical GERD symptoms, the problems that endoscopic treatments are often left at a partial solution level [4], [12]. The reason for this can be that, apart from fully reconstructing the natural barrier between the stomach and esophagus, fundoplication also takes care of the other issues like a weak diaphragm (crural repair) that may be causing the symptoms. Moreover, the subgroup analysis has shown that patients who were obese, had Barrett's esophagus or had a large hiatal hernia (more than 2 cm) were more likely to experience a return of their GERD symptoms after endoscopic treatment. It underscores the pivotal role of deciding the most appropriate therapy for each patient, which remains an essential aspect of managing GERD effectively [6]. The meta-analysis, quite surprisingly revealed that the differences between the individual studies were very large (I² = 71.9%). This indicated that there were differences in patient groups, study methods, types of treatments and ways of measuring results. Due to this, subgroup analysis was performed and they indicated that certain endoscopic interventions were more effective in some cases. In fact, Stretta treatment and fundoplication operation showed almost identical effects in patients with mild esophagitis and no major structural abnormalities [6]. Whereas, the comparison of LINX (a magnetic device) and TIF (Transoral Incisionless Fundoplication) resulted in the conclusion that LINX provided better symptom relief in the long run and more patients discontinued the use of PPIs, mostly after 3 to 5 years [5], [15].
They also differ as the LINX device utilizes a magnetic ring to augment the lower esophageal sphincter (LES) with which reflux is stopped while the patient is allowed to burp and vomit normally, something a traditional surgery may limit [5]. For instance, TIF (Transoral Incisionless Fundoplication) achieves the result by folding and tightening the tissue at the LES to rebuild the valve that prevents reflux. TIF generally does not have many side effects such as difficulty swallowing (dysphagia) or bloating that can still be quite pronounced in patients who have received a LINX device or fundoplication surgery. Nevertheless, this method relies more on the tissue integrity, which can become weakened overtime [8]. The meta-analysis also emphasized the significance of new endoscopic methods such as MUSE and ARMA, which were created to enhance older techniques. The MUSE unit integrates a camera, ultrasound and stapling into one instrument, and preliminary findings indicate that it can alleviate GERD symptoms almost free of any side-effect [9]. Nevertheless, these innovative methods are still undergoing research, and we are not yet sufficiently informed about their efficacy in the long run. Their inclusion in subsequent meta-analyses may change the relative effectiveness of the interventions as more longitudinal data become available. The funnel plot and Egger’s test did not pinpoint any clear evidence of publication bias, hence our findings appear to be unaffected by the non-reporting of studies. However, we must be careful with the extent to which some treatments appear to have been effective because of moderate heterogeneity, which indicates that studies vary widely [5].
Another major revelation from this evaluation is why it is so crucial to decide the correct therapy for each individual. The subgroup analysis revealed that young, low-weight patients, who follow the treatment well and have a straightforward GERD, represent the ideal candidates for endoscopic treatments such as TIF or Stretta [11], [15]. On the other hand, those who have complicated issues, e.g. paraesophageal hernias, obesity or have been suffering for a long time, generally get a better outcome from surgery, which can address the root cause of GERD thoroughly [12]. The decision to use endoscopic treatment or surgery is influenced by factors related to the patient's situation and finances as well. Studies indicate that endoscopic interventions are frequently carried out in outpatient clinics or day-care facilities, hence they are less expensive, take less time and generally do not require full anesthesia. Therefore, they are an excellent choice in low-resource setting or for patients who are elderly or have co-morbidities and thus surgical risk is high [10]. Surgery is usually effective in the long run, however, it is more expensive initially, the recovery period is longer, and there may be side effects such as swallowing difficulties, the surgical wrap shifting or gas accumulation that may require another operation later [4].
People who have undergone myotomy can still experience GERD, and this is particularly the case of patients with achalasia treated with POEM (per-oral endoscopic myotomy). In fact, while POEM is very effective in relieving dysphagia, research indicates that there is a higher chance of GERD occurring after POEM as compared to surgical myotomy because POEM does not have the anti-reflux barrier that surgery, such as fundoplication, provides [17]. Besides, a review points out that although POEM is minimally invasive and great for esophageal motility disorders, it is often necessary to resort to additional GERD therapies like drug treatment or another endoscopic procedure. In other words, it underlines the importance of anatomical correction in the case of a high reflux risk and echoes the concept of tailoring treatment strategies for GERD after POEM. The difference between treating GERD in children and adults is that the former is more complicated. Kids have different bodies, show different symptoms and metabolize medicine differently. A recent review recommended treatment according to a step-wise plan that is appropriate for the children. This plan comprises non-drug methods initially, for example, changing the child's position during feeding or modifying their diet. If these methods fail, medication may be used for a short time. Operations or endoscopies are only used in cases that are severe and difficult. The review also pointed to the latest therapeutic possibilities such as potassium-competitive acid blockers (P-CABs) and alginates, and emphasized the necessity of regulating the treatment closely and tapering off the medication when it is not needed anymore [18].
A recent investigation has proposed that endoscopic interventions yield the best results when they are performed after the failure of pharmacological therapy but prior to the aggravation of the disease and the necessity for surgical intervention. If one waits too long, the consequences may be detrimental and therefore, advocated for the early intervention of patients with a normal anatomical structure who are refractory to PPIs. Furthermore, they claimed that it is equally important to gather long-term follow-up data, to consider the cost-effectiveness of treatments and to employ biomarkers (biological signs) that assist in determining the optimal timing. This indicates that timing should be an integral part of the treatment agenda, and decisions ought to be made promptly and on the basis of the patient's individual condition [19].
Over the last five years, various studies have shown inconsistent outcomes regarding endoscopic and surgical treatments for GERD. For instance, a study that investigated patient satisfaction reported that patients preferred the endoscopic procedures [15]. Another study with a 10-year follow-up, however, came to the conclusion that surgery was more effective in symptom control and relapse prevention [3]. Our meta-analysis, reconciles all these recent research findings. It indicates that surgery still holds a slight advantage, the distance between the two types of treatments is narrowing, and the optimal treatment varies according to the patient's condition. Furthermore, the treatment of GERD is anticipated to go through continuous changes. The application of robotic surgery, AI-assisted endoscopy and non-invasive instruments such as impedance-pH monitoring and high-resolution manometry may facilitate doctors in making more accurate diagnosis and treatment plans [20]. Besides, hybrid operations combining the dexterity of endoscopy with the surgical firm anatomical support may be prevailing soon.
This meta-analysis, in addition to its numerous strengths such as thorough study search, well-defined selection criteria and an insightful subgroup analysis, also possesses a few limitations that should be acknowledged. Initially, the variation among the studies was from moderate to high (I² = 71.87%), which may have impacted the precision of the combined results. The reason for this could be that the studies differed in their design, the characteristics of the participants, the way the procedures were conducted, the duration of patient follow-up and the methods of outcome measurement. Moreover, not all studies provided complete information, particularly on long-term results, side effects, or quality of life, which made the detailed comparison of studies difficult. Additionally, most of the data, were from hospitals in wealthy countries, and therefore, the results may not be entirely applicable to low-resource settings. These limitations point to the necessity of more rigorously designed, long-term studies from various countries to strengthen the evidence in the future. As far as research perspective is concerned, it is necessary to have more robust studies that involve several hospitals and have a long-term follow-up of patients in order to have a clearer comprehension of the effectiveness of endoscopic treatments compared to surgery. Such studies should also evaluate cost-effectiveness in order to find out if the treatments are a financially viable option. Later on, it will be more valuable for researchers to focus on the aspects that matter most to patients, such as quality of life, getting better sleep and being able to eat comfortably. This will give a clearer picture of how these treatments influence patients' daily lives rather than just the medical outcomes.
This meta-analysis reveals that in the case of individuals with severe GERD or complicated situations such as those with large hernias, a surgical procedure, predominantly laparoscopic fundoplication or the LINX device, is still a bit more effective at symptom control. But, less invasive endoscopic procedures like TIF and Stretta are also quite effective for people with mild to moderate GERD and they have fewer side effects and a quicker recovery. Now that the difference in success between surgery and endoscopy is very small, it is obvious that the decision about treatment depends on the individual. Doctors and patients should decide together based on the patient’s body, health issues and personal preferences. Eventually, as endoscopic techniques become better and we have more long-term data, these minimally invasive methods may take a significant place in the treatment of patients.
Conclusion
This meta-analysis demonstrates that GERD (gastro-esophageal reflux disease) can be effectively treated with both surgical and endoscopic procedures. Though, surgery is still marginally more effective at managing symptoms and keeping the issue from returning, particularly in patients with severe GERD that doesn't improve with medication or for those with conditions like large hiatal hernia, surgical options like laparoscopic Nissen fundoplication and LINX (a magnetic device) tend to produce more long-lasting results. However, more recent endoscopic procedures like ARMA, MUSE, Stretta and Transoral Incisionless Fundoplication (TIF) have been emerged. These procedures allow for a quick recovery, are less invasive, have fewer side effects and require shorter hospital stays. They are therefore gaining popularity, particularly among patients who are elderly, unable to undergo surgery or prefer less invasive procedures. Doctors should use a customized approach to determine the best course of action because every GERD case is unique. The body weight of patient, the severity of the illness, the presence of hiatal hernia, the function of esophagus or any other health issue must be taken into account. Endoscopic procedures might be a good option for patients with mild to moderate GERD and has no complication. Surgery is still advised, though, in cases that are more complex and serious, or when alternative therapies have failed. As technology advances, shared decision-making in which physicians and patients collaborate to make decisions based on the most recent data will be helpful for achieving positive outcomes and making prudent use of healthcare resources.
References
- M Frazzoni and L Frazzoni, “Medical Management,” in Functional Diseases of the Esophagus, V. Landolfi and S. Tolone, Eds., in Updates in Surgery. , Cham: Springer Nature Switzerland (2026): 93-99.
- HT Lin, QJ Zhuang, JN Hu, and et al. “[Safety and efficacy of endoscopic and surgical anti-reflux procedures for gastroesophageal reflux disease: a systematic review and network meta-analysis],” Zhonghua Wei Chang Wai Ke Za Zhi Chin. J. Gastrointest. Surg 28 (2025): 10
- Y Tadé, D Newman, RW Walters, and et al. “Fundoplication significantly improves objective and subjective reflux outcomes—a meta-analysis,” Surg. Endosc 39 (2025): 4496-4504.
- E Reitano et al. “Antireflux Surgery: State of the Art From Diagnosis to Treatment,” Surg. Laparosc. Endosc. Percutan. Tech., Aug (2025).
- I Fatima et al. “S1021 Long-Term Safety and Efficacy of LINX Magnetic Sphincter Augmentation for GERD: Systematic Review and Meta-analysis,” Am. J. Gastroenterol 120 (2025): S220-S220.
- GM Pillai, PG Nair, M Arifuzaman, and et al. “eP284 STRETTA: Bridging the Gap Between Pills and Surgery for GERD Relief,” Br. J. Surg 112 (2025): znaf166.456.
- E Swei et al. “Effectiveness of transoral endoscopic fundoplication with or without hiatal hernia repair in patients with gerd and chronic cough,” Surg. Endosc., Oct (2025).
- PA Testoni and S Testoni. “New Techniques of Endoscopy,” in Functional Diseases of the Esophagus, V. Landolfi and S. Tolone, Eds in Updates in Surgery Cham: Springer Nature Switzerland (2026): 55-67.
- Q Meng, Z Yu, J Zhou, et al. “Endoscopic therapy with Medigus Ultrasonic Surgical Endostapler (MUSE) for gastroesophageal reflux disease: a case description,” Quant. Imaging Med. Surg 15 (2025): 10357-10365.
- D Chavan et al. “Role of anti-reflux mucosal ablation in ‘reflux-predominant’ refractory gastro-esophageal reflux disease patients - a randomized sham controlled trial,” Endoscopy (2025): a-2740-9297.
- G Costamagna and C Ciuffini. “Endoscopic Treatment of Gastroesophageal Reflux Disease,” in Functional Diseases of the Esophagus, V. Landolfi and S. Tolone, Eds., in Updates in Surgery. , Cham: Springer Nature Switzerland (2026): 123-129.
- P Maimaitiyusupu, A Aili, M Yisireyili, et al. “Comparative efficacy of sleeve gastrectomy with fundoplication versus standard sleeve gastrectomy in obesity and gastroesophageal reflux disease: A randomised trial,” Diabetes Metab 27 (2025): 6955-6967.
- H Hosaka et al. “The Role of Endoscopy in Gastroesophageal Reflux Disease”, Accessed: Dec. 01, 2025. [Online].
- O Ma, K Brar, S McCluskey, et al. “Long- term outcomes after per-oral endoscopic myotomy versus laparoscopic Heller myotomy in the treatment of achalasia: a systematic review and meta-analysis,” Surg. Endosc 39 (2025): 5985-5994.
- M Novia et al. “Magnetic sphincter augmentation for gastroesophageal reflux after sleeve gastrectomy: a prospective study,” Surg. Endosc., Sept (2025).
- S Yu et al. “A Non-invasive, Closed-Loop Electronic Stent for Real-Time Management of Gastroesophageal Reflux Disease,” Adv. Fiber Mater., Oct (2025).
- AST Kum, BCM Nunes, ETH Moura, et al. “Gastroesophageal reflux disease over time in endoscopic versus surgical myotomy for treatment of achalasia: Systematic review and meta-analysis,” Endosc. Int. Open 13 (2025): a-2621-5421.
- F. Calabrese et al., “Updated treatment options for gastroesophageal reflux disease in children: practical guide for clinicians,” Expert Opin. Pharmacother 26 (2025): 1631-1648.
- YN Gou, QB Shen, JY Hao, et al. “[Selection of timing for endoscopic treatment of gastroesophageal reflux disease: a discussion from an evidence- based medicine perspective],” Zhonghua Wei Chang Wai Ke Za Zhi Chin. J. Gastrointest. Surg 28 (2025).
- S-W Liu et al. “Recent advances in machine learning for precision diagnosis and treatment of esophageal disorders,” World J. Gastroenterol 31 (2025).


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 