Predictive Factors for Mortality in Patients with Malignant Pleural effusion Undergoing Pleurodesis via Video-Assisted Thoracoscopy in Senegal
Arroye Betou Fabrice Stéphane1*, Papa Amath Diagne2, Laurence Ngo Yon4, Charles Mve Mvondo5, Endale Mangamba Laurent-Mireille3, Ouethy Mireille3, Momar Sokhna Diop2, Souleymane Diatta2, Gabriel Ciss2
1Thoracic and Cardiovascular Surgeon, Department of Surgery and Specialties/Faculty of Medicine and Biomedical Sciences of the University of Yaoundé 1; Thoracic and Cardiovascular Surgery Department/ Laquintinie Hospital in Douala, Cameroon.
2Thoracic and Cardiovascular Surgeon, Faculty of Medicine, Pharmacy and Odontology / University of Cheikh ANTA DIOP, Department of Thoracic and Cardiovascular Surgery / Fann University Hospital, Dakar, Senegal.
3Pneumologist, Faculty of Health Sciences / University of Buea, Department of Internal Medecine / Laquintinie Hospital in Douala, Cameroon.
4Cardiovascular Surgeon, Department of Surgery and Specialties/Faculty of Medicine and Biomedical Sciences of the University of Yaoundé 1; Thoracic and Cardiovascular Surgery Department/ General Hospital in Yaounde, Cameroon.
5Cardiovascular Surgeon, Department of Surgery and Specialties/Faculty of Medicine and Pharmaceutical Sciences of the University of Douala; Thoracic and Cardiovascular Surgery Department/ General Hospital in Yaounde, Cameroon.
*Corresponding Author: Arroye Betou Fabrice Stéphane, Thoracic and Cardiovascular Surgeon, Department of Surgery and Specialties/Faculty of Medicine and Biomedical Sciences of the University of Yaoundé 1; Thoracic and Cardiovascular Surgery Department/ Laquintinie Hospital in Douala, Cameroon.
Received: 20 March 2025; Accepted: 25 March 2025; Published: 19 November 2025
Article Information
Citation: Arroye Betou Fabrice Stéphane, Papa Amath Diagne, Laurence Ngo Yon, Charles Mve Mvondo, Endale Mangamba Laurent-Mireille, Ouethy Mireille, Momar Sokhna Diop, Souleymane Diatta, Gabriel Ciss. Predictive Factors for Mortality in Patients with Malignant Pleural effusion Undergoing Pleurodesis via Video-Assisted Thoracoscopy in Senegal. Journal of Surgery and Research. 8 (2025): 526-533.
View / Download Pdf Share at FacebookAbstract
Background: This study aimed to identify predictive factors for mortality in patients undergoing pleurodesis via video-assisted thoracoscopy surgery
Methods: We conducted a prospective 10-month study including 51 patients with malignant pleural effusion who underwent pleurodesis via video-assisted thoracoscopy at the Department of Thoracic and Cardiovascular Surgery, University Hospital Centre of FANN in Dakar, Senegal. Sociodemographic, clinical, and therapeutic data were collected and analyzed using R software. Kaplan-Meier survival curves and the Cox model were employed to visualize survival probabilities and identify predictive factors for mortality.
Results: The mean age of patients was 50 ± 14 years, with a predominance of female patients (66.7% vs. 33.3%). The prevalence of malignant pleurisy was 49% (n = 25) for recurrent right-sided pleural effusion, 43% (n = 22) for recurrent left-sided pleural effusion, and 7.8% (n = 4) for recurrent bilateral pleurisy, with a mortality rate of 18% (n = 9). Occupational exposure (p = 0.015) and the use of traditional surgical techniques (p = 0.005) were significantly associated with reduced survival at 24 weeks. Predictive factors for mortality included sex (HR = 0.95; p = 0.02), the presence of comorbidities (HR = 0.98; p = 0.007), positive cytology (HR = 0.7; p = 0.02), and chemotherapy treatment (HR = 0.95; p = 0.04).
Conclusion: Our results show that factors such as sex, the presence of comorbidities, positive cytology, and the use of chemotherapy significantly influence patient survival. It is necessary to establish a multidisciplinary approach and increase access to the most appropriate diagnostic and therapeutic methods to optimize the survival of patients with malignant pleural effusion.
Keywords
<p>Malignant Pleural effusion, Predictive factors of mortality, Pleurodesis, Video-assisted thoracoscopy</p>
Article Details
Introduction
Malignant pleurisy, characterized by the presence of tumor cells in the pleural space, is a common complication of advanced cancers, particularly lung, breast, and ovarian cancers. This condition leads to fluid accumulation in the pleural cavity, causing symptoms such as dyspnea, chest pain, and a significant reduction in quality of life [1].
Globally, malignant pleurisy affects approximately 15% of cancer patients, with an estimated annual incidence of 150,000 to 200,000 cases in the United States alone [2]. In Africa, accurate data on the prevalence and incidence of this condition are scarce, primarily due to limited surveillance systems and comprehensive cancer registries. In Senegal, data are even more restricted, making it challenging to assess the true impact of malignant pleurisy on the population.
Management of Malignant Pleural effusion typically involves techniques such as repeated thoracentesis and chemical pleurodesis. However, these methods have notable limitations, including high recurrence rates, potential complications, and variable efficacy [3]. These challenges are further compounded in low-resource settings like Senegal, where limited access to quality healthcare, lack of specialized equipment, and insufficiently trained healthcare professionals intensify these difficulties [4].
In this context, video-assisted thoracoscopic surgery (VATS) pleurodesis has emerged as a promising alternative. This minimally invasive technique allows for direct visualization of the pleural cavity, enabling complete fluid evacuation and more effective pleurodesis [5]. Additionally, VATS is associated with lower recurrence rates and faster recovery compared to traditional approaches. However, its implementation in Senegal faces structural and financial obstacles, such as limited equipment and trained personnel.
Research on mortality predictors in patients with Malignant Pleural effusion is limited in Africa, particularly in Senegal, and often constrained by small sample sizes, inconsistent methodology, and insufficient follow-up [4]. This gap in local medical literature complicates efforts to plan care and develop effective management strategies.
Given this context, studying the predictive factors of mortality in patients with Malignant Pleural effusion who undergo VATS pleurodesis in Senegal is of great importance. Such research could help identify clinical and paraclinical variables that influence postoperative outcomes, refine management protocols, and better allocate scarce resources. Furthermore, it would help bridge the local data gap, supporting more effective healthcare planning for pleural conditions in this setting.
Materials and methods
Type, Period, and Location of the study
A prospective study was conducted over 40 weeks (10 months) from 1 January 2022 to 31 October 2022 in the Thoracic and Cardiovascular Surgery Department of the FANN University Hospital Centre in Dakar, Senegal. This department is a leading referral center in Senegal and West Africa for the management of thoracic and cardiovascular diseases. It is staffed by a multidisciplinary team of surgeons, anesthetists, and specialized healthcare professionals and is equipped to manage complex conditions, including lung cancers, pleural effusions, congenital heart malformations, and acquired cardiovascular diseases. The department is renowned for employing advanced techniques such as video-assisted thoracoscopy for minimally invasive procedures and plays a key role in providing advanced medical training to healthcare professionals, further enhancing its position as a center of excellence in the region.
Study population
The study included all hospitalized patients with confirmed neoplastic pleurisy, characterized by the presence of malignant cells in pleural fluid and/or malignant tumor proliferation in pleural biopsy histology. It also included cases of recurrent pleurisy of probable neoplastic origin, defined as any exudative pleurisy occurring in the context of confirmed primary malignancy, where neoplastic etiology could not be excluded by other causes of exudative pleurisy, particularly a negative GeneXpert result. Additionally, patients were required to have a minimum follow-up of six months post-operation to qualify for inclusion in the study.
Data collection procedure
Data were collected using a structured survey form. Sociodemographic, clinical, and therapeutic data were obtained from the department’s database, digital and physical medical records, and surgical protocol logs for all patients included in the study.
Statistical analysis
Data were recorded in an Excel spreadsheet (Microsoft Office, USA) and imported into R software version 4.4.1 for Windows. Categorical variables were summarized as counts (N), frequencies (n), and percentages (%). Quantitative variables were presented as means ± standard deviation (SD), minimum, and maximum values. The Shapiro-Wilk test was applied to assess the normality of quantitative variables. Fisher’s and Pearson’s independence tests, the non-parametric Mann-Whitney test, and the Log-rank test were used for statistical comparisons. Kaplan-Meier survival curves and the Cox proportional hazards model were used to identify predictive factors for mortality, calculating survival probabilities, hazard ratios, confidence intervals, and p-values. The confidence interval for the null hypothesis (Ho) was set at 95%, with a margin of error of 5% (Ho rejected if p < 0.05).
Results
Sociodemographic factors of the study population
The mean age of the study population was 50±14 years, with a range from 24 to 73 years. Female patients had a mean age of 48±13 years, ranging from 26 to 73 years, while male patients had a mean age of 53±14 years, with a range from 24 to 72 years. These ages were not statistically different (p = 0.2) (Table 1). The majority of female patients were housewives (n = 20, 48%), followed by those whose occupation was not specified (n = 5, 12%). Other occupations were represented in small proportions (Table 1).
|
Study population |
||||
|
Sociodemographic factors |
Overall |
Female |
Male |
p-value |
|
(N = 51) |
(N = 34) |
(N = 17) |
||
|
Age (years) [min - max] |
50±14[24-73] |
48±13[26-73] |
53±14[24-72] |
0.2 |
|
Occupations |
<0.001*** |
|||
|
Housewife |
20 (48%) |
20 (48%) |
0 (0%) |
|
|
Unspecified |
5 (12%) |
4 (9.5%) |
1 (2.4%) |
|
|
Farmer |
4 (11.9%) |
2 (4.8%) |
2 (7.2%) |
|
|
Teacher |
3 (7.1%) |
0 (0%) |
3 (7.1%) |
|
|
Shopkeeper |
2 (4.8%) |
1 (2.4%) |
1 (2.4%) |
|
|
Driver |
1 (2.4%) |
0 (0%) |
1 (2.4%) |
|
|
Student |
1 (2.4%) |
1 (2.4%) |
0 (0%) |
|
|
Mechanic |
1 (2.4%) |
0 (0%) |
1 (2.4%) |
|
|
Carpenter |
1 (2.4%) |
0 (0%) |
1 (2.4%) |
|
|
Soldier |
1 (2.4%) |
0 (0%) |
1 (2.4%) |
|
|
Painter |
1 (2.4%) |
0 (0%) |
1 (2.4%) |
|
|
Secretary |
1 (2.4%) |
1 (2.4%) |
0 (0%) |
|
The data are presented as mean ± standard deviation [minimum - maximum], frequency (N), and percentage (%). P-value: Wilcoxon rank sum test and Fisher’s exact test were performed to compare the mean age and the proportions of different occupations between genders. For these tests, the confidence interval for the null hypothesis (Ho) was set at 95%, with a margin of error of 5% (p significant if p < 0.05).
Table 1: Sociodemographic factors of the study population.
Prevalence and mortality rate of malignant pleuritis within our study population
The prevalence of malignant pleurisy was 49% for recurrent right pleurisy, 43% for recurrent left pleurisy, and 8% for bilateral recurrent pleurisy. The mortality rate was 18% (Table 2).
|
Malignant Pleurisy |
n (%) |
|
Recurrent right pleurisy |
25 (49%) |
|
Recurrent left pleurisy |
22 (43%) |
|
Bilateral recurrent pleurisy |
4 (8%) |
|
Deceased patients |
|
|
No |
40 (82%) |
|
Yes |
9 (18%) |
Table 2: Prevalence and mortality rate of malignant pleuritis within our study population.
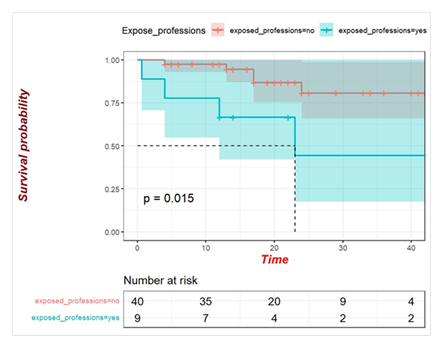
Impact of occupational exposure on the survival of patients with malignant pleurisy: Kaplan-Meier Survival Curve analysis.
Figure 1 illustrates that patients with malignant pleurisy who have occupational exposure to carcinogenic agents exhibit a significantly lower survival probability over time compared to those without such exposure. The turquoise line, representing the exposed group, declines more sharply, reflecting reduced survival, with this difference being statistically significant (p = 0.015). The confidence intervals around the curves suggest greater variability in the exposed group, likely attributable to the smaller sample size. Overall, occupational exposure emerges as a significant prognostic factor for mortality in this patient population (figure 1).
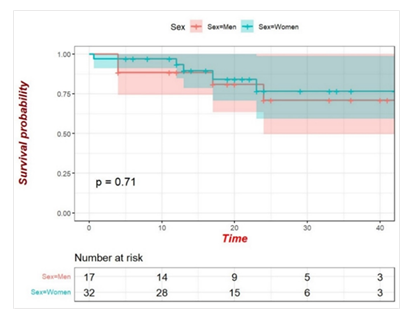
Comparative analysis of survival between men and women
The two groups exhibit similar survival trends, with overlapping confidence intervals represented in red and turquoise. The p-value (p = 0.71) indicates no statistically significant difference in survival probabilities between the two sexes. Overall, sex does not appear to be a significantly influencing factor for survival in this sample (Figure 2).
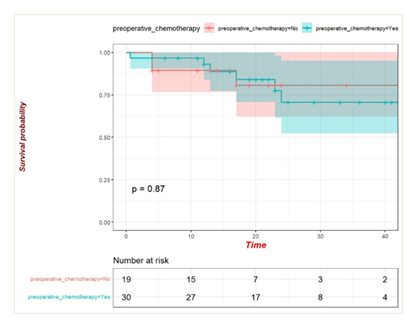
Preoperative chemotherapy and survival: Lack of impact as a predictive factor for mortality
The two groups exhibit similar survival probabilities over time, with overlapping confidence intervals suggesting comparable variability. The p-value (p = 0.87) indicates no statistically significant difference in survival between the two groups. Therefore, preoperative chemotherapy does not appear to be a major predictive factor for mortality in this patient sample (Figure 3).
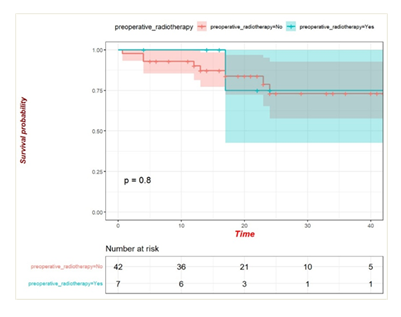
Preoperative radiotherapy: Lack of role as a predictive factor for mortality
Figure 4 indicates that preoperative radiotherapy does not appear to be a significant predictive factor for mortality in this patient sample. The two groups, those who received preoperative radiotherapy (turquoise) and those who did not (red), exhibit similar survival curves, with overlapping confidence intervals throughout the observation period. The p-value (p = 0.8) confirms the absence of a statistically significant difference between the groups. Therefore, preoperative radiotherapy does not seem to have a notable impact on survival outcomes, suggesting that it does not play a major role as a predictive factor for mortality in this population (figure 4).
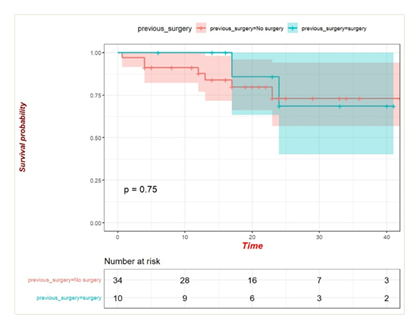
Impact of previous surgery on mortality: No significant predictive value
Figure 5 shows that previous surgery is not a significant predictive factor for mortality, as the survival curves for both groups (with or without previous surgery) are similar and show no statistically significant difference (p = 0.75) (Figure 5)
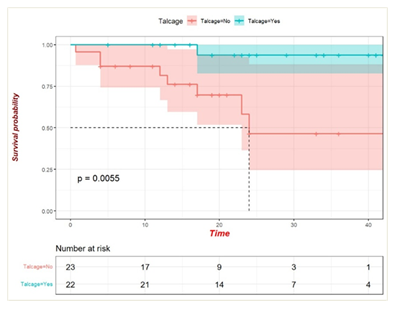
Impact of pleural symphysis via video-assisted thoracoscopy on survival: A significant predictive factor for mortality
Figure 6 indicates that pleural symphysis via video-assisted thoracoscopy is a significant predictive factor for mortality in this patient sample. Patients who underwent the procedure (turquoise curve) demonstrated markedly superior survival compared to those who did not (red curve). The difference between the two groups is statistically significant, as evidenced by the p-value (p = 0.0055). These results suggest that pleural symphysis via video-assisted thoracoscopy may have a positive impact on survival, making it an important factor to consider in patient management (Figure 6)
Predictive Factors of Mortality
Table 3 highlights several factors potentially predictive of mortality. Among these, male sex is associated with significantly higher mortality (p = 0.023), as are positive cytology (p = 0.021) and the absence of chemotherapy (p = 0.048). Paradoxically, the absence of comorbidities is linked to a shorter median survival (p = 0.007). In contrast, variables such as age, tumour location, type of pleurisy, and professional status do not show any significant association with mortality. These findings suggest that sex, cytological status, the presence of comorbidities, and the administration of chemotherapy play an important role in predicting mortality and should be considered to optimise patient management.
|
Factors |
Overall |
Median survival in months (extremes) |
Univariate analysis HR [95% CI] |
P-value |
|
Age (years) |
||||
|
< 50 |
24 |
19 (2 - 44) |
1 [0.7 – 1.2] |
0.655 |
|
> 50 |
27 |
16 (1 - 45) |
0.96 [0.7 – 1.2] |
|
|
Sex |
||||
|
Male |
16 |
19 (1 - 45) |
1 [0.7 – 1.2] |
0.023 |
|
Female |
34 |
16 (2 - 43) |
0.95 [0.7 – 1.2] |
|
|
Pleurisy |
||||
|
Recurrent right |
25 |
19 (2 - 45) |
1 [0.06 – 4.15] |
|
|
Recurrent left |
21 |
18 (1 - 44) |
0.94 [0.71 – 1.18] |
0.76 |
|
Bilateral |
4 |
16 (5 - 24) |
0.87 [0.35 – 2.16] |
0.32 |
|
Comorbidities |
||||
|
No |
4 |
13.5 (2 - 45) |
1[0.73 – 1.23] |
0.007 |
|
Yes |
46 |
19 (1 - 44) |
0.98 [0.73 – 1.23] |
|
|
Cytology |
||||
|
Negative |
47 |
19 (1 - 45) |
1 [0.6 – 1.25] |
0.021 |
|
Positive |
3 |
12 (8 - 13) |
0.7 [0.6 – 1.25] |
|
|
Location of tumour |
||||
|
Unknown |
17 |
21 (7 - 45) |
0.91 [0.48 – 1.35] |
0.222 |
|
Intrathoracic |
29 |
17 (1 - 44) |
0.95 [0.48 – 1.35] |
|
|
Extra thoracic |
4 |
16 (1 - 44) |
0.98 [0.67 – 1.28] |
|
|
Chemotherapy |
||||
|
No |
31 |
17 (1 - 42) |
1 [0.71 – 1.18] |
0.048 |
|
Yes |
19 |
22 (2 - 45) |
0.95 [0.71 – 1.18] |
|
|
Employee |
||||
|
No |
34 |
17 (1- 45) |
1 [0.71 – 1.2] |
|
|
Yes |
16 |
18 (7 – 44) |
0.96 |
0.515 |
Table 3: Cox Model Predictive of Mortality.
Discussion
Malignant Pleural effusion is a severe condition associated with poor prognosis, requiring appropriate therapeutic interventions to improve patient survival. Pleural symphysis via video-assisted thoracoscopy (VATS) is commonly used in palliative care to manage recurrent pleural effusions, but its impact on survival, particularly in specific settings such as Senegal, remains poorly studied. Identifying predictive factors of mortality in this population is essential to optimise clinical management, tailor therapeutic strategies, and improve patient outcomes. This study aims to explore the clinical and therapeutic determinants of survival in patients with Malignant Pleural effusion who underwent pleural symphysis via VATS in Senegal.
The findings of our study reveal that the mean age of patients with Malignant Pleural effusion undergoing pleurodesis by video-assisted thoracoscopy was 50 ± 14 years, with a predominance of female patients (66.7%), a prevalence of 49% for recurrent right pleurisy, 43% for recurrent left pleurisy, and 7.8% for recurrent bilateral pleurisy, along with a mortality rate of 18%. These results align and contrast with those of similar studies globally and in Africa.
Internationally, studies such as Ferrer et al. [6] reported a higher mean age of 65 years among patients with Malignant Pleural effusion, highlighting the association of pleurisy with advanced age in developed regions. Gender distribution varies across studies, with some showing a slight male predominance, possibly due to differences in cancer types leading to pleurisy, such as lung cancer, which is more common in men. The mortality rate in our study (18%) is slightly lower than rates often reported in developed countries, which may reach 20–30% in advanced malignancy cases [6].
In African settings, the findings are different. Studies like Diallo et al. [7] in Mali report a lower mean age of 41 years and a male predominance (sex ratio 2.3), reflecting the impact of different aetiologies. Tuberculosis, for instance, remains a significant cause of pleural effusions in Africa, often complicating the diagnosis and management of Malignant Pleural effusion. Mortality rates in African studies, such as 27% reported by Diallo et al., are generally higher, potentially due to delays in diagnosis, limited access to advanced therapies, and the prevalence of co-morbidities like HIV. The discrepancies in demographics, prevalence, and outcomes underline the importance of considering regional variations in disease aetiology, healthcare access, and diagnostic practices when analysing Malignant Pleural effusion and its management.
Our study revealed that occupational exposure (p = 0.015) and the use of traditional surgical techniques (p = 0.005) significantly reduced survival rates at 24 weeks. These findings align with existing evidence in the literature. Occupational exposure, particularly to asbestos, is widely recognised as a critical factor contributing to poor outcomes in malignant pleurisy, especially mesothelioma. This is primarily due to the aggressive nature of asbestos-related diseases and frequent delays in diagnosis. Robinson and Lake [8] demonstrated that prolonged asbestos exposure markedly decreases patient survival rates.
From a surgical perspective, recent studies, such as those by Rodriguez-Panadero [9], have shown that video-assisted thoracoscopic surgery (VATS) provides superior clinical outcomes compared to traditional open techniques. VATS significantly reduces post-operative complications, promotes faster recovery, and consequently improves survival rates. Furthermore, a review by Thomas et al. [10] identified VATS as the gold standard for managing malignant pleural effusions, with clear benefits for both survival and quality of life. Conversely, in African settings where access to advanced surgical technologies is often limited, traditional surgical techniques are still commonly used and have been associated with higher mortality rates, as noted by Diallo et al. [7].
These findings highlight the importance of implementing robust preventive measures to minimise occupational exposure risks, particularly through stringent regulation of asbestos use. They also underscore the need to expand the use of modern surgical techniques, such as VATS, especially in resource-limited settings. Lastly, the study calls for increased awareness and the development of early diagnostic strategies to improve clinical outcomes for patients with malignant Pleural effusion.
In our study, predictive factors for mortality in patients with malignant pleurisy undergoing pleurodesis via video-assisted thoracoscopy included sex (HR = 0.95; p = 0.02), presence of comorbidities (HR = 0.98; p = 0.007), positive cytology (HR = 0.7; p = 0.02), and chemotherapy treatment (HR = 0.95; p = 0.04). These findings align with existing literature. Studies, such as that by Clive et al. [11], have demonstrated that female sex is associated with better survival, possibly due to biological or hormonal differences. Comorbidities, such as cardiovascular disease or diabetes, significantly worsen prognosis, as confirmed by Clive et al., who emphasised the importance of holistic patient evaluation. Positive cytology, indicating malignant cells in pleural fluid, correlates with poorer outcomes, reflecting higher tumour burden, as reported by Ferrer et al. [12]. Chemotherapy, on the other hand, improves survival when the primary tumour is responsive, as evidenced by Fysh et al. [13], who found that systemic chemotherapy extended survival compared to supportive care alone. Together, these findings highlight the multifactorial nature of prognosis in malignant Pleural effusion and the need for tailored management strategies.
Conclusion
This study, conducted in Senegal, identified several predictive factors for mortality in patients with malignant Pleural effusion who underwent pleurodesis via video-assisted thoracoscopy. The findings highlighted the significant impact of sex, the presence of comorbidities, positive cytology, and chemotherapy on patient survival. Additionally, occupational exposure and the use of traditional surgical techniques were associated with a marked decrease in survival. These findings underscore the importance of an individualised approach tailored to the clinical characteristics of patients to improve outcomes in this specific context.
Ethical approval and consent to participate
Studies involving human participants were reviewed and approved by the Institutional Ethics Committee for Human Health Research at the University of Cheikh Anta Diop. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Data availability
The raw data supporting the conclusions of this article will be made available by the authors without any undue restrictions.
Conflicts of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
The authors confirm that this research was conducted without any external funding.
Authors' contributions
ABFS, SD, and GC designed the experimental approach and manuscript outline. ABFS, OM and SD recruited participants and performed laboratory analyses. ABFS and MSD conducted the statistical analysis. ABFS drafted the manuscript. SD, MSD and GS reviewed the manuscript. All listed authors contributed substantially, directly, and intellectually to the work and approved its publication.
Acknowledgements
We extend our heartfelt thanks to all the individuals who voluntarily agreed to participate in the study and to the staff of the Thoracic and Cardiovascular Surgery Department of Fann University Hospital for their support throughout the completion of this work.
References
- American Thoracic Society. Management of malignant pleural effusions. American Journal of Respiratory and Critical Care Medicine 162 (2000): 1987-2001.
- Roberts ME, Neville E, Berrisford RG, et al. Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline 2010. Thorax 65 (2010): 11
- Clive AO, Kahan BC, Hooper CE, et al. Predicting survival in malignant pleural effusion: Development and validation of the LENT prognostic score. Thorax 69 (2014): 1098-1104.
- Onyeanuna PE, Umeh OA, Nwosu N. Challenges in the management of malignant pleural effusion in low-resource settings. African Journal of Thoracic Diseases 6 (2019): 243-249.
- Bhatnagar R, Maskell NA. The modern diagnosis and management of pleural effusions. The British Medical Journal 21 (2014): 348
- Ferrer J, Roldán J, Teixidor J, et al. Predictors of pleural malignancy in patients with pleural effusion undergoing thoracoscopy. Chest 127 (2005): 1017-1022.
- Diallo S, Hassan M, Sissoko F, et al. Aetiologies of pleurisy in the pneumology department of Point G Hospital. Mali Médical 21 (2006): 39-41.
- Robinson BW, Lake RA. Advances in malignant mesothelioma. The New England Journal of Medicine 353 (2005): 1591-603.
- Rodriguez-Panadero F. Medical thoracoscopy. Respirology 23 (2018): 764-772.
- Thomas R, Fysh ETH, Smith NA, et al. Video-assisted thoracoscopic surgery for malignant pleural effusion: a review. Chest Journal 150 (2016): 109-124.
- Clive AO, Kahan BC, Hooper CE, et al. Predicting survival in malignant pleural effusion: development and validation of the LENT prognostic score. Thorax 69 (2014): 1098-1104.
- Ferrer J, Roldán J, Teixidor J, et al. Predictors of pleural malignancy in patients with pleural effusion undergoing thoracoscopy. Chest 127 (2005): 1017-1023.
- Fysh ET, Smith NA, Lee YC, Thomas R. Optimal management of malignant pleural effusions. Curr Opin Support Palliat Care 7 (2013): 138-146.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 