SIGN Hip Construct Nail, the Amazing Solutionin HIP Fracture Fixation without using an Image Intensifier
Jibananda Halder*, Mir Shahidul Hasan, Paresh Chandra Halder
1Department of Orthopaedic Surgery, National Institute of Traumatology & Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh
2UH & FPO, Dumki, Patuakhali, Bangladesh
3Department of Anaesthesiology, Sheikh Sahera Khatun Medical College, Gopalganj, Bangladesh
*Corresponding author: Jibananda Halder, Department of Orthopaedic Surgery, National Institute of Traumatology & Orthopaedic Rehabilitation (NITOR), Dhaka, Bangladesh
Received: 29 September 2021; Accepted: 06 October 2021; Published: 18 October 2021
Article Information
Citation: Jibananda Halder, Mir Shahidul Hasan, Paresh Chandra Halder. SIGN Hip Construct Nail, the Amazing Solutionin HIP Fracture Fixation without using an Image Intensifier. Journal of Surgery and Research 4 (2021): 544-552.
View / Download Pdf Share at FacebookAbstract
Introduction: Hip fractures within the orthopaedic literature are typically characterized as a drag of High-Income Countries (HICs). The largest growth is arises in developing countries like Africa, Latin America and Asia, due to the aged population and the increasing prevalence of osteoporosis in these countries.
Aim of the study: The main purpose of this study was to evaluate outcomes of using the SIGN Hip Construct (SHC) without the use of an image intensifier to accomplish hip fracture fixation.
Methods: Within 2017 to 2020, an approaching case series of patients with intertrochanteric fractures treated with the SHC was conducted at National Institute of Traumatology & Orthopaedic Rehabilitation (NITOR), Dhaka and Sir Salimullah Medical College Hospital, Dhaka.
Results: Out of 33 patients with trochanteric fractures with SHC were operated on, 21 were admitted for follow-up after 6 weeks. 76% of patients were outpatient within four weeks after surgery. Clinical signs of fracture union were observed in all patients after 6 weeks; all but one of them had radiological evidence of callus formation. In the 6-week follow-up study, 1 (1.5%) cases of infection and 3 (9.09%) collapsed varus were recorded.
Conclusion: With SIGN Hip Construct, it can be safely perform hip fracture fixation without an image enhancer. This implant can a good alternative option for developing countries, where it’s hard to access fluoroscopy with lots of limitation and bindings.
Keywords
<p>SIGN hip constract nail, Hip fracture, The amazing solution of hipfracure fixation</p>
Article Details
1. Introduction
Within the orthopaedic literature, Hip Fractures are typically characterized as a drag of High Income Countries (HICs). But the fact is, the highest growth incidence is predicted to occur in developing and under developing countries in Africa, Asia and Latin America, the aging population and therefore the increasing prevalence of osteoporosis within these countries. Intertrochanteric fractures are described as any fracture from the additional capsular a part of the neck of the femur to some extent 7.5cm distal to the lesser trochanter. Those fractures are unite nearly continuously with conventional treatment, but the high rate of complications related to prolonged immobilization within the elderly has made stable reduction and internal fixation the well-liked treatment. Internal fixation of trochanteric fractures allows early mobilization, which can be an evaluation for elderly population and it will helps to make life easier. Too many classification systems are proposed, but none of them have gained clinical use. Kyle and Evans have presented an easy classification, which is predicated on degree of fracture stability. Implants used for fixation of those fractures include adjustable angle device (e.g. McKee and McLaughlin nail plates), pin-plate assemblies (e.g. S-P nail plate), sliding compression screw assemblies (e.g. DHS, DCS), intramedullary nails (e.g. Ender nails, intramedullary hip screws) and fixed angle devices (e.g. Jewet nail plate, blade plate). The sliding hip screw and cephallomedullary nail in HICs became the foremost commonly used implants. Furthermore, fluoroscopy required to securely implant these devices, which cannot be available in many hospitals.

Figure 1: SIGN hip construct nail
To conquer those challenges, SIGN Fracture Care International evolved the SIGN Hip Construct (SHC). The SHC is intended to use in developed countries at a low cost hospitals and may be used without C-arm fluoroscopy guidance. However, few research thus far has checked out the effects of remedy of intertrochanteric fractures with the SHC withinside the absence of fluoroscopy. In this study, the main intend is to document short-time period effects of the SHC for remedy of intertrochanteric fractures of the femur without using the Image intensifier.
2. Materials and Methods
A prospective case series of patients with intertrochanteric fractures treated with the SHC between 2017 and 2020 was conducted at National Institute of Traumatology & Orthopaedic Rehabilitation (NITOR), Dhaka and Sir salimullah Medical College Hospital, Dhaka. The SHC was selected to treat hip fracture patients as it is a suitable solution for our study center because it can be used without an image intensifier. Ethical clearancewas obtained from Natiional Institute of traumatology & Orthopaedic Rehabilitation (NITOR), Dhaka. The patients were provided a standard regiment of third-generation cephalosporins preoperatively which was continued postoperatively for 3 days. Clinical data for all patients was collected prospectively. Plain radiographs were performed preoperatively, postoperatively, and at the 6-week follow-up visit. Fractures were sub-classified as stable or unstable based on the presence of posteromedial comminution involving the lesser trochanter. Patients were invited for a follow-up visit at 6 weeks postoperatively. Outcomes measured during follow-up included rate of infection, varus collapse, and weight-bearing status Movement of the operated limb and partial weight bearing with axillary crutches were permitted beginning on the first postoperative day. Full weight bearing was allowed only when radiographs showed evidence of union.
3. Results
An overall of 33 patients with trochanteric fractures had been operated the use of the SHC and accompanied for at least six weeks. There were 21 male and 7 female patients (78% and 21%))
3.1 Surgical Technique
Before surgery, the SHC template and pre-op X-rays were used to estimate the specified length of compression screws also because the angle of placement. An equivalent was performed for the only interlocking screw required. Spinal anesthesia induction was performed and therefore the patient was placed within the lateral decubitus position.

Figure 2: Some pictures, how to introduce nail and screw without C arm
A direct lateral approach was made to the proximal femur. An incision was made in the fascia lata from the tip of the distal trochanter to the crest of the vastus. The vastus lateralis was cut below the crest of the vastus to expose the lateral aspect of the femur. The fractures were reduced by traction and palpation manipulation of the fracture site to assess the quality of the reduction. Patients were treated by two trained surgeons who were appointed by the SIGN organization in the use of the SHC.

Figure 3: Operation at NITOR
All of those Implants were introduced by ensuing standard techniques. SHC uses a 10*280 mm intramedullary nail which is inserted through a trochanteric entry point. Proximal fixation is achieved by a single locking screw and two lag screws that run along but not through the nail. After a hand drilled pilot hole was made, and then compression screws were inserted. Correct positioning of the pilot holes was achieved with a blunt hand drill (“pilot drill”). With a combination of the Z-angle Finder (coronal plane) and palpation of the anterior femoral neck (axial plane), the angle was determined. Distal fixation is accomplished with a single distal locking screw that is placed using a template. The operated limb movement and partial weight bearing with axillary crutches were permitted beginning on the first postoperative day. When the radiographs showed evidence of union then full weight bearing was allowed only.
|
Age group by years |
Total patients |
In Percentage (%) |
|
15 to 30 |
3 |
9.09 |
|
31 to 46 |
5 |
15.15 |
|
47 to 52 |
2 |
6.06 |
|
53 to 68 |
8 |
24.24 |
|
69 to 84 |
13 |
39.39 |
|
85 |
2 |
6.06 |
|
Total |
33 |
100 |
Table 1: Patients demographic
In this case 15 patients (44%) were presented to the hospital within 24 hours of injury. Within 2 to 10 days of injury, 15 patients were presented and 3 patients presented more than 10 days after. Who presented earlier generally lived within the region of the observation center while those who had delayed, they lived in other regions in Bangladesh. The most common injury mechanism was a fall from standing height, which was observed in 15 (45.45%) cases. There were 3 (9.09%) patients who fell from a height greater than standing height. Traffic accidents were the second leading cause and were observed in 11 (33.33%) cases. Among the traffic accidents there were 5 drivers, 3 passengers and 3 walkers. Four (12.12%) patients suffered bodily injuries. The majority (no=6, 18.18%) of the patients suffered a stable intertrochanteric fracture. Stable fractures were more frequently due to falls, while unstable fractures were due to higher-energy mechanisms.
|
Types of fracture |
MTA No (%) |
Fall From height No (%) |
Fall (standing) No (%) |
Assault No (%) |
Total No (%) |
|
Stable |
6(18.18) |
2(6.06) |
9(27.27) |
2(6.06) |
19(57.57) |
|
Unstable |
6(18.18) |
1(3.03) |
5(15.15) |
2(6.06) |
14(42.42) |
|
Total |
12(36.36) |
3(9.09) |
14(42.42) |
4(12.12) |
33(100) |
Table 2: Mechanism of injury and Stable versus unstable fracture
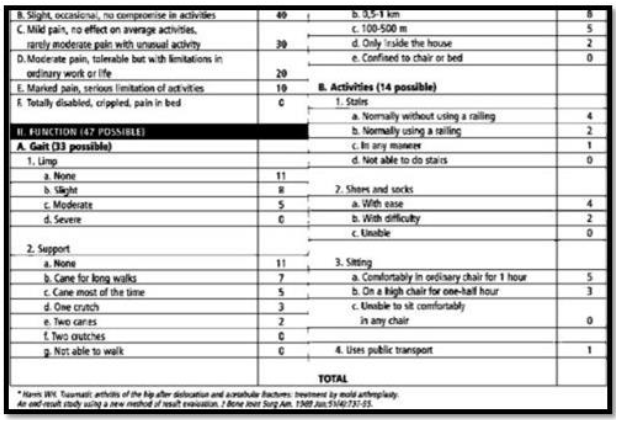
Figure 4: Graph showing various activities
In the graph we can see, that the score has a maximum of 100 points (best possible result) and covers
Function (7 items, 0-47 points),
Pain (1 item, 0-44 points),
Range of motion (2 elements, 5 points) and
Absence of deformities (1 item, 4 points).
|
Haris Hip score |
Number (n) |
Percentage (%) |
|
Excellent |
14 |
42.42 |
|
Good |
13 |
39.39 |
|
Fair |
3 |
9.09 |
|
Poor |
3 |
9.09 |
Table 3: Haris Hip score
In our study Harris Hip score (Excellent +Good), 27(81.81) 82%, satisfactory.
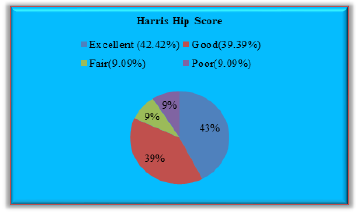
Figure 5: Outcome assessment on Harris Hip Score
Most cases (54.4%) had a delay of 10 days or more from the time of presentation to the date of surgery. This is often due to the lack of an operating room, as cases are processed in the order they arrived at the hospital. Some of the delays in surgery were due to comorbid medical conditions, such as diabetes mellitus and high blood pressure. The follow-up rate after six weeks was 67% (21). Total 12 patients who were late for follow-up and could be contacted by phone; inability to receive transportation in these patients, 7 patients who lost follow-up care could not be located. Patients who could not go to the clinic due to traffic reasons lived far from the center. Most of them (76%) were able to walk within 4 weeks after the operation. And 3 of the patients who had a delay in mobilization of more than 3 weeks, one had a concomitant spinal injury, one had severe postoperative anemia and another had generalized metastasis. Rest of the patients achieved the ability to walk within 4 weeks after the operation. At the 6 week follow-up, there was one patient case of infection (3.03%) and 3 of them cases of varus collapse (9.09%)
|
Time of injury to surgery (Days) |
Complication further than six weeks |
||||
|
Change of angle |
Infection |
None No. (%) |
Lost follow-up No. (%) |
Total No. (%) |
|
|
<7 |
0 (0) |
1 (3.03) |
6 ( 18.18) |
2 (6.06) |
9 (27.27) |
|
Aug-14 |
1 (3.03) |
0 (0) |
7 (21.21 ) |
1(3.03) |
9 (27.27) |
|
>15 |
2 (6.06) |
0 (0) |
9(27.27) |
4 (12.12) |
15 (45.45) |
|
Total |
3 (9.09) |
1 (3.03) |
22 (66.66) |
7 (21.21) |
33 (100) |
Table 4: Injury to surgery time, in relation to complication after 6 weeks

Figure 6: Case selection
4. Discussion
In this study, we tried provide the short-term results of the SIGN hip structure for the treatment of intervertebral fractures without the fluoroscopy Image guidance. We find out that SHC allows for mobilization within a reasonable period of time after operation in most cases. This result was obtained with a relatively low infection rate (3.03%). Varus collapse is not uncommon (9.09%). Another important thing, there have been no cases of femoral head resection with hip violation, which is a major concern for those patients. The postoperative surgical site infection continues to be a major concern in any surgical procedure performed in a low-resource environment, particularly when systematic use of open reduction techniques is used. Particularly, the rates of infections we measured in our patient population were similar to those reported by other studies. Those are included with HIC. For example, Edwards et al. (10) did a similar study in the UK and found the prevalence of deep and superficial wound infections to be 1.2%. Currently, there are no studies that directly compare infection rates between SHC and other types of hip implants.
Limitations of the study:
The major limitation of this study was, the sample size was too small. Otherwise, this will still be the largest published report on the implant. We are also limited by the short follow-up time period and the high rate of follow-up loss. Although this limits is our ability to comment on long-term clinical outcomes, research supports the safety of the device for broader use in developing environments. Our second major limitation was the absence of a comparison group, which limits the inferences that can be made. There are no other implantable devices that can be used in a similar setting without requiring C-arm, which makes such a study difficult to perform. Finally, no data were collected on patient-centered or functional outcomes, such as healthiness related quality of life.
Recommendation
In this study, our primary results provide the primary report of the security and feasibleness of the SIGN Hip concept is especially for developing country. Most significantly, the SHC could be a viable different to non-operative treatment that has been shown to be related to vital mortality and morbidity. Where in future work has to be done to assess long-run clinical and photography outcomes of the SHC. In this study we support the continuing use and analysis of the device.
5. Conclusion
SIGN Hip Construct is a safe surgical treatment option for intertrochanteric fractures in developing countries without the use of intraoperative image guidance.
Funding:
Self
Conflict of interest:
None
Ethical approval:
Yes
References
- Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int 7 (1997): 407-413.
- Elffors L. Are osteoporotic fractures due to osteoporosis? Impacts of a frailty pandemic in an aging world. Aging (Milano) 10 (1998): 191-204.
- Russell TA. Fracture of the hip and pelvis. Campbell’s operative orthopaedics. Grenshaw AH (8th edtn), St. Louis Missouri, USA: Mosby yearbook Inc 2 (1992): 895-987.
- Ganz R, Thomas RJ, Hammerle CP. Trochanteric fracture of the femur. Treatment and results. Clin Orthop 138 (1979): 30-40
- James PS, Andrew HS, Philip JK. Surgical treatment of orthopaedic trauma. Thieme publisher (2007).
- Evans EM. The treatment of the trochanteric fracture of the femur. J Bone joint Surg Brit 31 (1949): 190- 203.
- Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty- two inter trochanteric hip fractures. J Bone Joint Surg Am 61 (1979): 216-221.
- Singh M, Nagrath AR, Maini PS. Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg Am 52 (1970): 457-467.
- Bodoky A, Neff U, Heberer M, et al. Antibiotic prophylaxis with two doses of cephalosporin in patients managed with internal fixation for a fracture of the hip. J Bone Joint Surg Am 75 (1993): 61-65.
- Edwards C, Counsell A, Boulton C, et al. Early infection after hip fracture surgery: risk factors, costs and outcome. J Bone Joint Surg Br 90 (2008): 770-777.
- Jain R, Basinsk A, Kreder HJ. Nonoperative treatment of hip fractures. SICOT 27 (2003): 11-17


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 