Bilateral Approach with Botulinum Toxin Type A Injections in Patients with One-Sided Facial Hyperkinetic Movements
Chrisanthi Karapantzou1,2*, Joao Pedro Vale3, Frank Joachim Haubner4, Konstantinos Zagoridis4, Konstantinos Agas4, Konstantinos Karagogos4, Nikoleta Zagoridou4, Martin Canis5
1University ORL Department, Ludwig-Maximilians University Munich, Germany
2Interbalcan Medical Hospital, ORL Department, Thessaloniki, Greece
3Belage Clinic, Lisbon, Portugal
4University ORL Department, Ludwig-Maximilians University Munich, Germany
5University ORL Department, Ludwig-Maximilians University Munich, Germany
*Corresponding Author: Chrisanthi Karapantzou, University ORL Department, Ludwig-Maximilians University Munich, Germany.
Received: 17 February 2022; Accepted: 25 February 2022; Published: 04 March 2022
Article Information
Citation: Chrisanthi Karapantzou, Joao Pedro Vale, Frank Joachim Haubner, Konstantinos Zagoridis, Konstantinos Agas, Konstantinos Karagogos, Nikoleta Zagoridou, Martin Canis. Bilateral Approach with Botulinum Toxin Type A Injections in Patients with One-Sided Facial Hyperkinetic Movements. Archives of Clinical and Medical Case Reports 6 (2022): 149-172.
View / Download Pdf Share at FacebookAbstract
Background: Main subject of our investigation was to clarify, if a bilateral approach with Botulinum toxin type A injections is more efficient from cosmetic and functional aspect, compared to unilateral injections, in patients with one-sided facial hyperkinetic movements, like synkinesis and hemi facial spasm.
Methods: Our patient cohort included 30 patients suffering from unilateral hyperkinetic facial contractions. We performed a total of 60 injections, 30 of them only on the affected side and 30 on both facial sides. All participants underwent 2 botulinum toxin sessions, with a 4 months period lying between the injections. Our statistical analysis was divided into 4 hypothesis testing - sub-groups, based on the results of the subjective satisfaction rates our patients delivered 2 months and 6 months after the initial botulinum toxin session. Furthermore 2 doctors evaluated the results based on pre-and after photographs on a Quartile Grading Scale for objective evaluation for the same time periods. Each one of the observers received one patient group, either with bilateral or with ipsilateral treatments, without knowing which group they received.
Results: Summarizing the statistical results we analyzed from both sources (patients and doc-tors-observers), we found statistically significant differences in satisfaction rate between the two groups (p=.004) and a better objective evaluation on patients who underwent combined treatments.
Conclusions: Our work confirmed the initial assumption that patients with facial asymmetry of different etiology benefit from a bilateral therapeutic approach with botulinum toxin injections, instead of one-sided injections into the hyperkinetic or dyskinesia facial side.
Keywords
<p>Mimic muscles, Botulinum Toxin</p>
Article Details
1. Introduction
An intact face and a normal functioning system of mimic muscles reflect a person’s character and personality. The emotional expressiveness and sociability are features which are determined by facial mimicry. This is the main reason which explains a low extraversion level that is being ob-served in people suffering from hyperkinetic facial disorders. Clinical findings of excess facial movements and facial asymmetry lead to more reserved behaviors, especially in social settings. All these movement dysfunctions stigmatize subjects, leading to low self-esteem, depression and even social isolation [1-4]. Facial disorders that are found frequently in practice and might potentially have such a major impact on quality of life, are synkinesis and hemi facial spasms. Depending on the affected area, both conditions can lead to vision difficulties through periocular muscle spasms and to dysarthria and dysphagia, when the particular region is involved [1]. The consecutive dynamic and even static imbalance of the facial muscles has a major impact on the face, as it leads to aesthetic changes. It is not only the pathological movement of the affected side that is responsible for this facial asymmetry, but also the response of the muscular system of the healthy facial side, as it often develops a hyper dynamic activity [5]. This condition can be recognised easily at rest, as well as during dynamic mimic muscle activation, as the healthy side may develop deeper or more prominent rhytids, due to enhanced muscular activity of the antagonistic muscles [6]. On the other hand, the pathological side can have voluntary or involuntary muscular contractions or lead to a flattening of overlying facial areas, depending on the underlying dyskinetic condition (5). Compensatory hyperkinetic movements on the healthy side, may lead consecutive to following clinical signs: deeper rhytids on the frontalis region, a narrow eye aperture, nose deviation, prominent nasolabial folds, perioral asymmetry with movements of the mouth corner laterally upwards [7,8]. Analytically, synkinesis has typical features of synchronous and uncontrolled movements of specific areas of mimic muscles, which appear secondary to facial nerve palsy. These sequelae might have an early onset, even 1-2 months after the palsy [9]. Typically, a muscle group of in-tended activation is followed by unintended activation of neighboured muscle groups. The most common forms are the ‘’oculo-oral ‘’with midfacial muscle contraction and lifting of the mouth corner during voluntary eye closure and the ‘’oro-ocular’’, where patients experience an uninten-tional eye closure or eye narrowing, while trying to project their lips, like in kissing or voluntarily smiling [10]. It can be defined as the co-existence of muscular movements of different facial areas, which don’t appear under normal conditions. Its pathogenetic mechanism is complicated, but the most acceptable theory discusses a paradox regeneration of axon during recovery, following facial palsy [11].
In cases of hemifacial spasm, which is a dysfunction that affects the peripheral nervous system, patients develop one-sided, tonic-clonic spasms of the mimic muscles. The symptomatology starts initially with an intermittent, forced eye closure and expansion of the spastic movements into caudal direction. In 97% of the cases there is a unilateral manifestation, while there is described a bilateral appearance in only 3% [2]. The disorder may appear following a facial nerve irritation like trauma, brain tumor or very often due to a compression of the facial nerve at its exit place in the brainstem, caused by the anterior inferior cerebellar artery. A retrograde transmission which is created by nerve compression is postulated to irritate the facial nucleus [12,13]. Next, the nucleus reacts to his inability to process this unusual stimulation, with creation of uncontrolled facial twitching. These recurring muscular contractions persist even at rest and can even lead to sustained facial tonus phenomena, that appear with ‘’locked’’ expressions like closed eyes, contracted cheeks or mouth corners. Patients experience not only pain, but also sudden loss of depth perception, due to limitation of binocular vision [14-16].
2. Results
Our patient cohort included 30 patients, 8 diagnosed with hemifacial spasm and 22 with synkinesis secondary to facial palsy. All participants where suffering at least 2 months from symptoms that resulted in facial asymmetry. We performed a total of 60 injections, 30 of them only on the affected side and 30 on both facial sides. All participants underwent 2 botulinumtoxin sessions, with a 4 months period lying between the injections. We divided our 30 patients into two groups as following:
Group A: 15 patients who received bilateral botulinum toxin type A injections into both facial sides dyskinetic and healthy.
Group B: 15 patients who received unilateral botulinum toxin type A injections only into the affected facial side.
Main aim of this work was to analyze if a combined functional – cosmetic bilateral treatment is superior to an unilateral functional treatment for patients with dyskinetic movement patterns, that lead to facial asymmetry. Our statistical analysis was therefore divided into 4 hypothesis testing- subgroups, based on the results of the subjective satisfaction rates our patients delivered 2 months and 6 months after the initial botulinum toxin session (both patient groups included):
3. Hypothesis
Control of the hypothesis that there exist significant differences in the me-dian satisfaction rate between participants of group A and participants of group B, 2 months after the initial botulinum toxin injection treatment. We performed diagnostic controls, testing the existence of outliers, normality distribution and homogeneity of variance in both patient groups. According to these tests we could not find outliers, as graphically demonstrated on the boxplot diagram of figure 1. The satisfaction rate of the two patient groups showed a normal distribution on the Shapiro-Wilk-test (group B/bilateral injections = .155, group A /one-sided injections = .473) (Table 1) [17]. Further, an equality of variance could be confirmed between the two subject groups (Levene’s test, p = .889), [18]. Study participants of group A (one-sided botulinum toxin injections) showed a lower median satisfaction rate (Μ= 57.33, SE= 3.58) compared to group B (bilateral botulinum toxin injections) (M=72.66, SE= 3.30) (Table 2). This difference of -15.33, 95% CI [-25.31, -5.35], is statistically significant t(28) = -3.147, p= .004 and reflects an effect size estimation of r=0.51 (Table 3) [19].
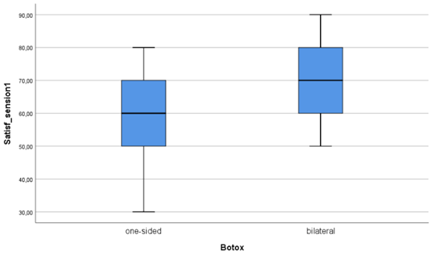
Figure 1: Boxplot diagram for the existence of outliers for the satisfaction rate between the two groups, in 2 months’ time after the initial botulinum toxin treatment.
Table 1: Test of normality of the satisfaction rate between the two groups, 2 months after the initial botulinum toxin treatment.
Table 2: Group statistics of the mean satisfaction rate of both groups, 2 months after the initial botulinum toxin 153 treatment.
Table 3: Levene’s test for equality of variances between the two groups, 2 months after the initial botulinum toxin treatments.
4. Hypothesis
Control of the hypothesis that there exist significant differences in the median satisfaction rate between participants of group A and participants of group B, 6 months after the initial botulinum toxin injection treatment. We performed diagnostic controls, testing the existence of outliers, normality distribution and homogeneity of variance in both patient groups. According to these tests we could not find outliers, as graphically demonstrated on the boxplot diagram of figure 2. The satisfaction rate of the two patient groups showed a normal distribution on the Shapiro-Wilk-test (group B/bilateral injections = 0.082, group A /one-sided injections = 0.188), [17] (Table 4). Further, an equality of variance could be confirmed between the two subject groups (Levene’s test, p = 0.512) (Table 6), [18]. Study participants of group A (one-sided botulinum toxin injections) showed a lower median satisfaction rate (Μ= 70.00, SE= 3.90) compared to group B (bilateral botulinum toxin injections) (M=86.00, SE= 3.20) (Table 5). This difference of -16.00, 95% CI [ -26.34, -5.65], is statistically significant t(28) = -3.167, p= 0.004 and reflects an effect size estimation of r=0.51 (Table 5, 6), [19].
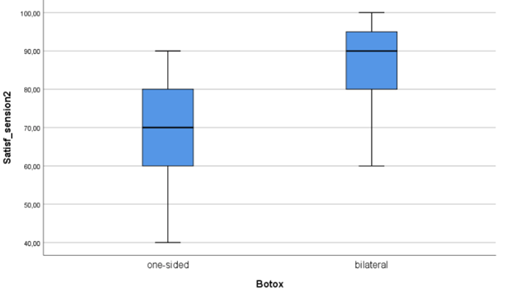
Figure 2: Boxplot diagram for the existence of outliers for the satisfaction rate between the two groups, in 6 months’ time after the initial botulinum toxin treatment.
Table 4: Test of normality of the satisfaction rate between the two groups, 6 months after the initial botulinum toxin treatment.
Table 5: Group statistics of the mean satisfaction rate of both groups, 6 months after the initial botulinum toxin treatment.
Table 6: Levene’s test for equality of variances between the two groups, 6 months after the initial botulinum toxin treatments.
5. Hypothesis
Control of the hypothesis that there exist significant differences in the median satisfaction rate between participants of group B, 2 and 6 months after the initial botu-linum toxin injection treatment. Patients of this group expressed a lower satisfaction rate 2 months after their initial treatment (M=57.33, SE=3.58), compared to their responses 6 months after the first session (M=70.00, SE=3.90) (Table 7). This difference of -12.66, 95% CI [-15.045, -7.432], is statistically significant t [14] = -6.141, p < .001, reflecting a high effect size estimation of r= 0.85 (Table 8) [19].
Table 7: Paired samples statistics summarizing the mean satisfaction rate of group B, 2 months and 6 months after the initial treatment.
Table 8: Paired samples statistics summarizing the mean satisfaction rate of group B, 2 months and 6 months after the initial treatment.
6. Hypothesis
Control of the hypothesis that there exist significant differences in the median satisfaction rate between participants of group A, 2 and 6 months after the initial botu-linum toxin injection treatment. Patients of this group expressed a lower satisfaction rate 2 months after their initial treatment (M=72.66, SE=3.30), compared to their responses 6 months after the first session (M=86.00, SE=3.20) (Table 9). This difference of -13.33, 95% CI [ -14.068, -6.252], is statistically significant t[14] = -10.583, p < .001, reflecting a high effect size estimation of r= 0.94 (Table 10), [19].
Table 9: Paired samples statistics summarizing the mean satisfaction rate of group A, 2 months and 6 months after the initial treatment.
Table 10: Paired samples statistics summarizing the mean satisfaction rate of group A, 2 months and 6 months after the initial treatment.
Additionally, we performed a comparison between the objective evaluation of doctor 1 and doctor 2, based on the QCS scale, with the assistance of the IBM® SPSS® Statistics 26 as statistical software platform [16]. According to the data we received (Table 10.), we created figure 3 and figure 4. With 30 valid scores out of 30 and no one excluded, doctor 1 who received group A patient pre- and after botulinum toxin photographs had a median score of 3,5 and doctor 2 who received group B a median score of 3,0. The maximum score that could be achieved according to the QGS scale was 4,0, reflecting the major imaginable improvement after botulinum toxin treatment in subjects with pre-existing facial asymmetry.
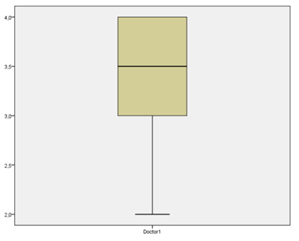
Figure 3: Boxplot diagram of the evaluation by doctor 1 of group A, that received a combined bilateral botulinum toxin treatment (x axis). The y axis reflects the score points on the QCS scale (max. 4, min. 0).
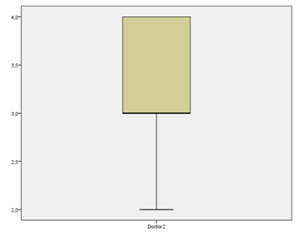
Figure 4: Boxplot diagram of the evaluation by doctor 2 for group B, that received a one-sided botulinum toxin treatment (x axis). The y axis reflects the score points on the QCS scale (max. 4, min. 0).
Although mild and transient side effects like ptosis, orbicularis weakness and epiphora or mouth deviation might occur, we didn’t experience any difficulties in bilateral treatments, except 2 female patients, who received one sided injections. These two patients developed a slight mouth deviation after their first toxin application into the M. orbicularis oris on the affected side, which we could correct through a one-point additive injection into the M. orbicularis oris fibers of the con-tralateral, healthy side after 7 days.
7. Discussion
Botulinum toxin type A injections are the most common therapeutic approach for one sided facial muscle spasms, that lead to visible facial asymmetry, as seen in patients with post-paretic synkinesis or hemifacial spasm. The inhibition of the hyperkinetic muscle fibers through neurotoxin injections on the affected side aims to improve facial function and manage pain caused by mimic muscle contractions. The chronic character of these clinical entities demands repetitive, follow up treatments in intervals of 3-4 months between injections [1, 2]. Patients often develop over time hyperdynamic rhytids on the healthy facial side, or a visible facial asymmetry compared to the contralateral side. The repeated toxin injections on the affected side lead to a ‘’flattened’’, atrophic appearance of the target muscles. Harrison et al. and Li et al. discussed even irreversible local facial atrophy not only in animal studies, but also in patients with hemifacial spasms who received one-sided treatments, what could theoretically be related to denervation atrophy caused by botulinum toxin, as a part of the muscle may lose normal nerve nutrition and produce segmental atrophy in the muscle fibers [25, 26]. All these parameters contribute in patient dissatisfaction, as they might experience relief of the symptoms on the affected side, but develop parallely facial imbalance and asymmetry [3- 5]. Individuals are not only confronted to difficulties in daily activities and functioning, but deal also with facial asymmetry, that affects their aesthetic appearance. This phenomenon leads even to misinterpretations of emotions, as facial mimicry plays a crucial role in emotional expressiveness, sociability and quality of life [2, 4, 22, 23]. Facial harmony has the potential to enhance patient self-confidence and satisfaction. Our work points out the necessity of a bilateral botulinum toxin treatment approach, in order to achieve a balance between functionality and cosmetic improvement of the face. We examined and confirmed the hypothesis that a bilateral botulinum toxin injection approach is superior to classical unilateral injections on the affected side in facial asymmetry, secondary to synkinesis or hemifacial spasm. We collected data of 30 patients we recruited, suffering either from synkinesis or hemifacial spasm. Our subjects received two cycles of botulinum toxin during a period of 4 months’ time. They were divided in two groups of 15, each. Group A included patients who received unilateral injections and group B patients who underwent combined, bilateral injections by the same, experienced injector. Patient photographs were taken 2 months and 6 months after the initial session (Figure 8). Every participant documented subjective satisfaction rate on a scale from 0% to 100%, 2 months after every botulinum toxin session. Furthermore, two independent doctors supported our research question and rated as observers pre- and after photographs of our patients, taken 2 months and 6 months after their initial therapy. One doctor (doctor 1) received all photographs taken from group A, while the other one all photographs from group B. With the as-sistance of the QCS scale the two doctors were asked to evaluate the improvement on facial symmetry, without knowing if their group underwent a one-sided or a two-sided therapy [16].
Summarizing the statistical results we analyzed from both sources (patients and doc-tors-observers), the superiority of bilateral versus unilateral botulinum toxin injections in facial asymmetries caused mainly by hemifacial spasm and synkinesis, could be confirmed. Although the median subjective satisfaction was already 2 months after the first treatment pleasant, there could be achieved rates of up to 86% for bilateral approaches and of 70% for unilateral therapies. The difference in satisfaction rate between the two groups is statistically significant (p=.004), proving the assumption of a better outcome experienced by patients after combined treatments. The two observers’ comparison between patient photographs based on the QCS scale, revealed a lower median score for group A (3.0), while there could be reached a higher median score [3,5] for group B (bilateral injections). The results of our research point out the importance of combined functional - aesthetic botulinum toxin therapies, which don’t focus only on the affected facial side, as practiced by the majority of injectors (Figure 9-11). Parallel injections on the healthy facial side, into antagonistic mimicry muscles, which have to overwork to balance out the inhibited, injected muscles on the pathological side, turn out to be a necessity. The mean doses we applied on the affected side were 26, 28 Units and on the non-affected side 11,62 Units, what gives an analogy of estimatedly 3:1. This fact leads to the assumption, that even very few toxin addition on the non-affected facial side, can achieve a significant improvement in facial function and symmetry.
This very promising, innovative therapeutic aspect in the management of facial hyperkinetic syndromes, opens a new way in restoring facial asymmetries successfully, with the single use of botulinum toxin. It is known that injectable fillers can simultaneously support weak muscles and enhance toxin efficacy through a fine-tuned balance between antagonist and synergist groups [31, 32]. Although we couldn’t find literature discussing bilateral toxin injection for facial symmetry restoration as presented in our work, there exist few research projects that tested only partial facial asymmetry restoration with neurotoxin administration. We can confirm the conclusion made in an interesting review work published by Heydenrych I., that a new dynamic balance between the paralyzed and non-paralyzed sides can be achieved, although in that work neurotoxin was applied in smile muscles to neutralize the overacting, asymmetric side [4]. Armstrong et al. studied the treatment of 24 patients with facial symmetry associated to facial synkinesis, with a focus on the orbital and oral regions [29]. The results found 68 out of 72 treatments having an improved cosmesis [29]. This is one of the few existing examples, that supports our results of a positive impact in the overall aesthetic appearance, through botulinum toxin as monotherapy. Although there occurred dose-related complications in higher dose groups of this study in 20 out of 39 patients, we couldn’t confirm the same following our dilution and injection protocol, as we had only a slight mouth deviation in 2 out of 15 patients after their first one sided injection session. Major complications described by other authors as diplopia, exposure keratopathy, inadvertent lip biting, impaired chewing ability, dysarthria and worsening in appearance were not reported [29]. Gladly, there was no adverse event reported by patients who underwent bilateral toxin applications during our project. Although there exist some descriptions of addressing the compensatory hyperkinesia in the non-paralyzed side of the face, there was also an article published by Jahromi et al. that suggested that contralateral injections of the non-paralyzed face with botulinum toxin may improve the recovery time of a facial palsy, in cases where the palsy has a reversible cause. This very interesting perspective lacks randomized controlled trials in humans, is limited to reversible causes of facial palsy, but gives a future direction, proving that the field of botulinum toxin applications is still growing [33]. The ‘’Munich Injection Concept’’ for the management of asymmetries we used (figure 5,6), can assist injectors, simplifying the assessment of the face in similar, demanding therapeutic concepts [21]. In bilateral, combined functional-aesthetic facial injections, precision and safety are essential for a successful outcome [21]. Asymmetry, secondary to dyskinetic conditions, can lead indeed to abnormal resting tone and impaired facial expressions with negative psychological consequences. Normal muscle function can be improved, as muscle contractions can be restored regarding their coordination and symmetry [4, 10, 27, 28]. Our protocols can function as essential tools in combined treatments, as they define injection depth and injection points we suggest, based on our experience, to maximize effectivity and safety [21]. Thus, further research on combined treatments, as here introduced, is mandatory to optimize the assessment of the asymmetric face. Emphasis on improving facial harmony from therapeutic and cosmetic aspect, signifies a new challenging era in botulinum toxin applications.

Figure 8: Female patient with synkinesis (right), hyperdynamic rhytids on the healthy frontalis side (left) and visible asymmetry on her eye brow levels. Photographs taken during her initial status, 2 months and 6 months (starting from the top), after a bilateral botulinum toxin injection approach.
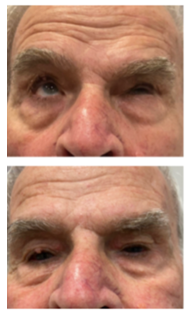
Figure 9: Male patient with hemifacial spasm (left). Prior and 6 months after the application of the combined aesthetic-functional, bilateral botulinum toxin concept in the periocular and frontal area.
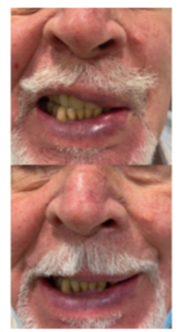
Figure 10: Male patient with hemifacial spasm (left). Prior and 6 months after the application of the combined aesthetic-functional, bilateral botulinum toxin method in the midface and perioral area.

Figure 11: Female patient with hemifacial spasm (left). Prior and only 2 months after the combined aesthetic-functional botulinum toxin treatment into the periocular and frontal zone.
8. Materials and methods
The gold standard among conservative therapeutic treatments in the management of hyperkinetic movements associated to synkinesis and hemifacial spasm are botulinum toxin injections on the affected facial side [1, 2]. The aim is to restore facial function and minimize muscular tension and aching caused by the uncontrolled spasms. The neurotoxin is injected directly, ipsilateral, into the muscles that are involved in each one of these clinical entities. Botulinum toxin type A is a minimal invasive, very effective method with good patient tolerability. It is a tool which offers safe results when the injections are performed by experienced injectors, who choose proper injection techniques and dosages. Moreover, respecting facial anatomy regarding the depth of injection and a proper choice of the target muscles, are required. Therefore, profound knowledge of anatomy is indispensable before treating these patients. Improvement is observed in 2-10 days post injection and may last up to 3 to 5 months [1]. We had made through years the observation, that patients who received injections on both facial sides – affected and non-affected - have benefited from a functional and a cosmetic aspect more from our treatments, than patients who received only one-sided injections on the hyperkinetic side. In order to support our hypothesis, we designed and performed a prospective, blinded, mo-nocentric study on 30 patients, between March 2019 and September 2021. All patients were treated by the main author in the ORL Department of the Interbalcan Medical Hospital in Thessaloniki and with permission of the Hospital’s Ethics Commission. We performed a total of 60 injections, 30 of them only on the affected, hyperkinetic side and 30 on both facial sides, including the healthy side. Our 6 male and 24 female subjects had an age range from 37 years to 86 years. 8 patients of our cohort suffered from hemi facial spasm and 22 from synkinesis secondary to facial palsy, with an onset of at least 2 months after manifestation. All participants underwent 2 botulinum toxin sessions, with a 4 months period lying between the initial and the second treatment. We divided our 30 patients into two groups as following:
Group A: 15 patients who received bilateral botulinum toxin type A injections into both facial sides (dyskinetic and healthy).
Group B: 15 patients who received unilateral botulinum toxin type A injections only into the dyskinetic facial side.
In order to assess our patients with safety, we applied injections using an injection protocol that the first author and colleagues developed in the ORL University Department of the Ludwig Maximilians University in Munich, which we introduce here as ‘’Munich injection protocol for facial asymmetry restoration’’ [21]. This protocol includes specific injection points, dosages and injection depth (Figure 5, 6). Aim of the development of this helpful tool was to provide safe injections regarding injection depth and placement of injections, in order to minimize diffusion into neighbored muscles and limit complications following injections, especially in the midface and lower face areas [21]. Injections were performed using a 33 Gauge, 12 mm long needle, and with a dilution of a 100 Units botulinum toxin (Botox®) vial with 3 ml of NaCl. In functional disorder treatments we normally use a 4 ml neurotoxin dilution as suggested by Laskawi and in aesthetic applications a dilution of 2,5 ml for the standard 100 Units bottle, as practiced in cosmetic medicine [1,15]. For this study we diluted the toxin with 3 ml of NaCl, increasing toxicity on each injection point, in order to restore functionality and gain a softer cosmetic outcome, compared to the even less diluted toxin, used in strict aesthetic indications. The treatment begins when the upper facial third is affected, with more than 5 injection points (a 2.5 to 5 Units), placed on the healthy side of the frontalis muscle to inhibit hyperdynamic rhytids (Figure 5, 6), (Table 1), [21]. The periocular area can be approached with 3 injection points (a 2.5 Units) into the lateral fibers of the M. orbicularis oculi, in order to open the orbital margin on the ptotic side and elevate the eyebrow (Figure 5, 6). The upper point at this area should be placed 5 mm lower than the eyebrow tail hairs, in order to ensure eyebrow elevation, as some frontalis muscle fibers can anatomically insert below the boarder of the lateral eyebrow (Figure 5), [21]. If hyperdynamic rhytids are observed on the pathological side along the nasal dorsum, there can be placed one or two in-jection points (a 2.5 Units) into the middle part of the transverse part of the nasalis muscle (Figure 5, 6), [21], in order to avoid diffusion into the M. levator labii superioris alaeque nasi. The treatment of the middle facial part, which is often involved in hemifacial spasms and synkinetic disorders, is a real challenge. In the midface, contracted muscles on the pathological side are observed and treated carefully with very low doses, starting with single injections of 2.5 Units per point. Overcorrections should be avoided, as they lead to visible asymmetries in this region. According to the Munich in-jection concept, contralateral midface muscles on the healthy side must be injected, as they appear prominent, due to their normal activity [21]. Through neurotoxin injections we achieve their ‘’flattening’’, as they give the impression of asymmetry, when compared to the affected side. Main muscles we choose for injections on the non-affected midface side are the M. levator anguli oris and the M. zygomaticus minor. This approach allows us to flatten the midface and reduce normal upper lip activity into upward direction. The perioral area can be assessed with a single injection into the M. zygomaticus major of the affected side, as it is responsible for drawing the angle of the mouth, allowing smiling often much more superiorly than on the contralateral dyskinetic side. 2.5 Units can be placed into the fibers of the M. orbicularis oris superior to the upper lip and sometimes into the M. risorius, in order to balance out the hyperdynamic activity we observe on the healthy side (Figure 5, 6), [21]. If there appear spasm-like contractions in the affected mental area, we inject 2 points a 2.5 Units into the M. mentalis and place also 2.5 Units with a single injection into the contralateral mentalis (Figure 5, 6). Injections into the lower part of the M. depressor anguli oris and depressor labii inferioris, should be avoided, as this has the danger of lower lip asymmetry (Table 11), [21]. Photographs were always taken with the use of the same camera, in the same room, without day-light effects, at rest and during standardized facial movements: Upward movement of the eyebrows, gentle and tight eye closure, smiling, teeth showing, kissing, while activating the glabella muscles and during nasal creasing.

Figure 5: Munich Concept - Injection point protocol for restoring of facial asymmetry.
Source: Anatomy of Human Face and Neck Muscles Digital Art by StockTrek Medical Images (Editing Karapantzou)
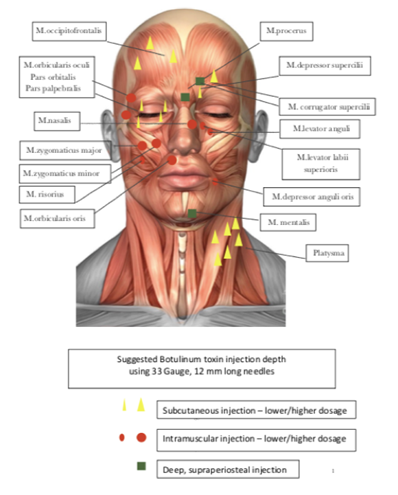
Figure 6: Munich Concept – Injection depth protocol for restoring of facial asymmetry.
Table 11: Anatomy, injection points and injection depth according to the ‘’Munich concept – injection protocol’’ for combined facial botulinum toxin injections [21].
8.1. Objective evaluation
The effectivity of the clinical neurotoxin application was evaluated by the comparison of photographs of the treated faces, taken at rest and during activity of the mimic muscles, prior, 2 months and 6 months after the initial treatment. Two independent medical doctors, one ORL and one General doctor - Aesthetic practitioner, compared those photographs, using the QCS scale (Quartile Grading Scale), without knowing which subjects belonged to group A or B (Table 12, Table 13), [16]. One doctor received all patients from group A (doctor 1) and the other all patients from group B (doctor 2). Every doctor received 30 pre-and after injection photographs, out of a total of 60 pre- and after photographs taken, as we took photographs 2 months and 6 months after the initial session. The QCS scale we used had the following structure, giving the opportunity of evaluation from 0-4 points (0 = no improvement, 4 = major improvement): The two doctors filled out the evaluation form of Table 2, without having information if they were given group A or group B patient photos. The first doctor we mention as ‘’doctor 1’’ received photographs of group A (one-sided injections) and the second doctor we mention as ‘’doctor 2’’ received photographs from group B (bilateral injections). The filled evaluation forms were given to the main author and forwarded for statistical analysis.
|
0 |
(<1-25%)= no improvement after treatment |
|
1 |
(1-25%)= minimal improvement |
|
2 |
(26-60%)= moderate improvement |
|
3 |
(51-75%)= no improvement |
|
4 |
(<1-25%)= Suffficient improvement |
|
5 |
(<1-25%)= major improvement |
Table 12: Quartile Grading Scale for objective evaluation.
|
Group A/B Patient Number |
Evlution Score after 1. Session |
Evlution Score after 1. Session |
|
1 |
||
|
2 |
||
|
3 |
||
|
4 |
||
|
5 |
||
|
6 |
||
|
7 |
||
|
8 |
||
|
9 |
||
|
10 |
||
|
11 |
||
|
12 |
||
|
13 |
||
|
14 |
||
|
15 |
Table13: Doctors objective evaluation form including patient number and evaluation score after the 1. And 2. Botulinum toxin session. Doctor 1 received photographs from Group A (bilateral treatment) and doctor 2 received photographs from Group B (one sided treatment). No one between the observers knew which patient group he was asked to evaluate.
8.2. Subjective evaluation
Subjective satisfaction rate was evaluated on a scale of 0%-100% (figure 7), where 0% reflected missing improvement and 100% the presence of the maximal imaginable improvement. This evaluation was completed by the patients twice, 2 months and 6 months after the initial treatment. Therefore, they were handed out forms with a satisfaction rating scale to be filled out, twice. The filled forms were collected by the main author. We received a total of 60 subjective satisfaction rate results from our 30 participants.
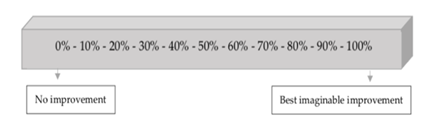
Figure 7: Subjective satisfaction rating scale.
Author Contributions
Funding
This research received no external funding
Institutional Review Board Statement
25/22.12.21 Ethics Approval by the Ethics Commission of the Interbalcan Medical Hospital, Thessaloniki, Greece
Informed Consent Statement
Yes
Data Availability Statement
Yes
Conflicts of Interest
The authors declare no conflict of interest.
References
- Laskawi R, Roggenkämper P. Botulinumtoxin-Therapie im Kopf-Hals-Bereich; 2. Auflage, Urban & Vogel Medien und Medizin Verlagsgesellschaft GmbH & Co. KG, Munchen 6 (2004).
- Karapantzou C. Blepharospasmus vom Levator-Inhibitions-Typ, Klinik-Therapieoptionen: Analyse von Patienten nach Lid-Frontalis-Suspensions-Operation; Süddeutscher Verlag für Hochschulschriften (2016).
- Choi KY. Analysis of Facial Asymmetry. Arch Craniofac Surg 16 (2020): 1-10.
- Heydenrych I. The Treatment of Facial Asymmetry with Botulinum Toxin: Current Concepts, Guidelines and Future Trends; Indian J Plast Surg 53 (2020): 219-229,
- Sadiq SA, Khwaja S, Saeed SR. Botulinum toxin to improve lower facial asymmetry in facial nerve palsy. Eye (Lond); 26 (2012): 1431-1436.
- Sahan A, Tamer F. Restoring facial symmetry through non-surgical cosmetic procedures after permanent facial paralysis: a case report 26 (2017): 41-42,
- Salles AG, da Costa EF, Ferreira MC, et al. Epidemiologic Overview of Synkinesis in 353 Patients with Longstanding Facial Paralysis under Treatment with Botulinum Toxin for 11 years. Plast. Reconstr. Surg 136 (2015): 1289-1298,
- Cooper L, Lui M, Nduka C. Botulinum toxin treatment for facial palsy: A systematic review. J Plast Reconstr Aesthet Surg, 70 (2017): 833-841.
- Celik M, Forta H, Vural C. The development of synkinesis after facial nerve paralysis. Eur Neurol 43 (2000): 147-151.
- Mehdizadeh OB, Diels J, White WM. Botulinum Toxin in Treatment of Facial Paralysis. Facial Plast. Surg Clin N Am 24 (2016): 11-20.
- Huang X, Wang W, Ding W. Mechanisms and Management of Postparalysis Facial Synkinesis, Chinese. J of Plast and Reconstr Surg 3 (2021): 89-94.
- Gardner WJ, Sava GA, Hemifacial spasm: a reversible pathophysiologic state. J Neurosurg 19 (1962): 240-247.
- Dou NN, Zhong J, Zhou QM, et al. The mechanism of hemifacial spasm: a new understanding of the offending artery. Neurol Res 37 (2015): 184-188.
- Kemp LW, Reich SG. Hemifacial Spasm. Curr Treat Options Neurol 6 (2004): 175-179.
- BOTOX® Cosmetic Prescribing Information, Allergan Inv. Irvine, August (2015)
- Mohamed L Elsaie, Shady I, Wael S. Ablative Fractional 10 600 nm Carbon Dioxide Laser Versus Non-ablative Fractional 1540 nm Erbium-Glass Laser in Egyptian Post-acne Scar patients. Journal of Lasers in Medical Sciences 9 (2018): 32-35.
- Sam S. Shapiro, Martin Bradbury Wilk: An analysis of variance test for normality (for complete samples), Biometrika 52 (1965): 591-611,
- Howard Levene. Robust tests for equality of variances. In: Ingram Olkin, Harold Hotelling et al. (Hrsg.): Contributions to Probability and Statistics: Essays in Honor of Harold Hotelling. Stanford University Press 5 (1960): 278-292,
- Rosenthal R, Rosnow RL, Rubin DB. Contrasts and effect sizes in behavioral research: A correlational approach. Cambridge: Cambridge University Press (2000).
- L Sachs. Angewandte Statistik. Springer (1997): 427-431,
- Karapantzou C, Vale JP, Haubner F, et al. Restoring Functionality and Aesthetic Appearance in Hyperkinetic Disorders of the Face with Botulinum Toxin. Clin Surg. 7 (2022): 3412.
- Wiener A, Touloei K, Glick BP. A Novel Long-term Therapy of Facial Synkinesis with Botulinum Neurotoxins Type A and Fillers. J Clin Aesthet Dermatol 4 (2011): 45-49.
- Beurskens CHG, Oosterhof J, Nijhuis-van der Sanden MWG. Frequency and location of synkinesis in patients with peripheral facial nerve paresis. Otol Neurotol 31 (2010): 671-675.
- Chua CAN, Quhill F, Jones E, et al. Treatment of aberrant facial nerve regeneration with botulinum toxin. Orbit 23 (2004): 213-218.
- Li Y, Huang Y, Ding Q, et al. Evaluation of concentrations of botulinum toxin A for the treatment of hemifacial spasm: A randomized double-blind crossover trial. Genet.Mol.Res 14 (2015): 1136-1144.
- Harrison AR, Berbos Z, Zaldivar RA, et al. Modulating neuromuscular junction density changes in botulinum toxin-treated orbicularis oculi muscle. Invest Ophthalmol. Vis Sci 52 (2011): 982-986,
- Robinson MW, Baiungo J. Facial rehabilitation: evaluation and treatment strategies for the patient with facial palsy. Oto-laryngol Clin North Am 51 (2018): 1151-1167.
- Choi KH, Rho SH, Lee JM, et al. Botulinum toxin injection of bith sides of the face to treat post-paralytic facial synkinesis. J Plast Reconst Aesthet Surg; 66 (2013): 1058-1063.
- Armstrong MW, Mountain RE, Marray JA. Treatment of facial synkinesis and facial asymmetry with botulinum toxin type A following facial nerve palsy. Clin Otolaryngol Allied Sci 21 (1996): 15-20,
- Kahn JB, Gliklich RE, Boyev KP, et al. Validation of a patient-graded instrument for facial nerve paralysis: the FaCE scale. Laryngoscope 111 (2001): 387-398.
- De Maio M. Myomodulation with injectable Fillers: An Innovative Approach to Addressing Facial Muscle Movement. Aes-thetic Plast Surg 42 (2018): 798-814.
- De Maio M, Heydenrych I, Boca Raton, Florida: CRS Press. Myomodulation (2020)
- Hamidian Jahromi A, Konofaos P. Contralateral Facial Botulinum Toxin Injection in Cases with Acute Facial Paralysis May Improve the Functional Recovery: Where We Stand and the Future Direction.World J Plast Surg 10 (2021): 89-92.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
