Was this a Bilateral Testicular Torsion? Dilemma of a Paediatric Surgeon-Case Report
Sonia Nogalska1*, Marcin Polok2, Agata Lukawska1, Marcin Rasiewicz2, Maciej Baglaj2
1Wroclaw Medical University, Wroclaw, Poland
2Department of Paediatric Surgery and Urology, Wroclaw Medical University, Wroclaw, Poland
*Corresponding Author: Sonia Nogalska, Wroclaw Medical University, wybrzeze Ludwika Pasteura 1, 50-367 Wroclaw, Poland
Received: 17 October 2019; Accepted: 30 October 2019; Published: 06 January 2020
Article Information
Citation:
Sonia Nogalska, Marcin Polok, Agata Åukawska, Marcin Rasiewicz, Maciej BagÅ‚aj. Was this a Bilateral Testicular Torsion? Dilemma of a Paediatric Surgeon-Case Report. Archives of Clinical and Medical Case Reports 4 (2020): 024-029.
View / Download Pdf Share at FacebookKeywords
<p>Bilateral Testicular Torsion; Paediatric Surgeon</p>
Article Details
1. Introduction
A testicular torsion in the newborn is a frequent cause of infertility amongst male patients. Extravaginal torsion of the spermatic cord may occur perinatally, before the tunica vaginalis settles in the scrotum [1]. It includes situations in which the torsion is prenatal (intrauterine), postnatal or related to an undescended testis [2]. Most commonly, testicular torsion is unilateral, and bilateral torsion is extremely rare.
2. Case Report
An 8-day-old boy was admitted to the Department of Paediatric Surgery and Urology from the Neonatology Department. His mother was a 37-year-old woman who gave birth by caesarian section (due to a gynaecological indication) at 38 weeks of gestation (gravida 2, para 2). The infant weighed 3530 g, and the final Apgar score was 10. During pregnancy and labor, the mother did not suffer any severe complications. Since birth the infant had a noticeable discoloration and swelling of the left hemiscrotum. A Doppler ultrasound showed that both testicles were in the scrotum, and the left testicle was enlarged (2.5 × 1.5 cm) with a lack of arterial blood flow-an image consistent with a gonadal torsion. In the right testicle there were no abnormal findings. During physical examination, the left testicle was significantly enlarged and hardened. The redness of the left scrotal skin was noted. The child was prepared for a surgical exploration.
Intraoperatively, the surgeons diagnosed an extravaginal torsion and macroscopic necrosis of the left testicle. From the scrotal approach, a left-sided orchiectomy was performed. Then, in order to fix the contralateral testicle in place, an exploration and orchiopexy of the right testicle was performed. This is a standard procedure in our clinic in the cases of testicular torsion. During exploration of the right scrotum (done in order to fix the right testicle), the tunicas of the testicle were brown, thickened and hardened. Macroscopically, the testicular parenchyma was brown and did not show the typical arterial blood flow, but there was no torsion of the exposed spermatic cord. A right-sided orchiopexy was performed, and a biopsy for the histopathological examination was taken. The postoperative course of the patient was uneventful. Four weeks after the surgery, a follow-up examination showed a right testicle sized 8 × 5 × 12 mm located in the scrotum. Further examinations at 10 and 13 months revealed no testicle in the right hemiscrotum. The testis was nonpalpable on physical examination and not visible on ultrasound, likely due to atrophy. The patient is still followed by the urological and endocrinological outpatient clinics.

Figure 1: Left testicle before amputation.

Figure 2: Right testicle, suspicion of a testicular torsion.
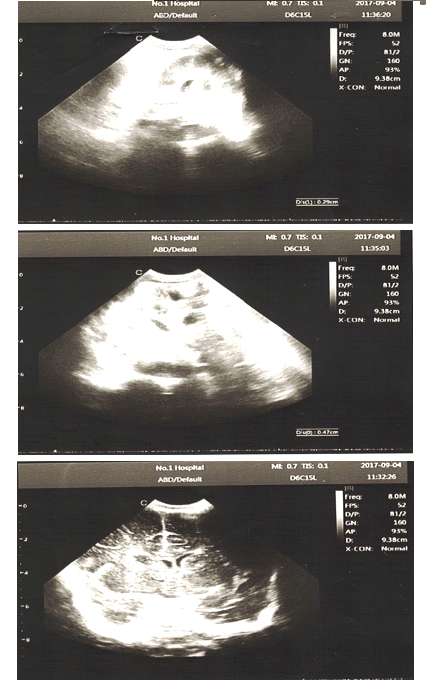
Figure 3: An ultrasound examination.
3. Discussion
Bilateral testicular torsion is a very rare entity. Testicles can twist synchronously or asynchronously. A meta-analysis by Monteilh et al. reviewed all English-language articles published from 2005 to 2015 about patients with neonatal testicular torsion (NTT) diagnosed within the first thirty days of life. In the group of 196 patients, there were only 14 observations of bilateral testicular torsion (of which 9 were asynchronous) [3]. What is interesting, Yerkes et al. point out, is that bilateral torsions occur in 11% to 21% of all perinatal torsions, of which 11% to 50% are asynchronous [4]. The first documented case of a simultaneous bilateral testicular torsion in a newborn infant was published by Frederick et al. [5]. They suggested that the cause of a bilateral testicular torsion may be based on an anatomic arrangement-for example, a loose attachment of the infant’s tunica vaginalis or an abnormal attachment of the Cremaster muscle [5].
In addition, Gorbonos et al. presented a case of torsions that occurred in two brothers. The first boy was diagnosed with bilateral extravaginal torsions on the 4th day of life, and two years later the second boy was born with left testicular torsion. They proposed the hypothesis that an autosomal, X-linked recessive mode of inheritance may exist in some cases of perinatal torsion. Interestingly, this could also mean that synchronous or asynchronous contralateral torsion may not always be the effect of the adherence of the tunica vaginalis to the scrotal wall. A familial predisposition to this affliction would necessitate the careful postnatal surveillance of the newborns with a family history of perinatal torsion [6].
Yerkes et al. emphasised that in their experience, in cases of bilateral asynchronous perinatal torsion, there were no signs or symptoms that would suggest acute or subacute torsion of the contralateral testis on the initial examination or even after exploration (in several cases) [4]. Comparing those situations to our patient’s case, acute symptoms and the lack of arterial blood flow were present only in the left hemiscrotum. There were no abnormalities found on the right hemiscrotum. The probable cause of the ischemia of the right testis, found intraoperatively in our patient, was a previous abrupt torsion of the spermatic cord that detorsed spontaneously right before the surgery. Yerkes et al. also suggest that in the cases of bilateral asynchronous torsion, both tests should be exposed before deciding to remove either testicle, to maximize the potential for hormonal function [4].
A study by Kaye et al. [7] presented a total of 16 neonatal torsions-from 13 prenatal only one case suffered from bilateral testicular torsion. One of the bilaterally torsed tests was infarcted and necrotic on biopsy, but it was still detorsed and fixed in place. Unfortunately, the tests were fully atrophied at the 3-month follow-up. In our material, at the 13-month follow-up of our patient, ultrasonography showed no tests in the right scrotum. On a recent visit in the outpatient clinic, the right testicle was not palpable in the scrotum or the inguinal canal. Because of this, we presumed that the right gonad had become atrophied. Kaye et al. [7] also proposed an algorithm for use in the cases of bilateral neonatal torsion. It suggested that an emerging bilateral exploration via an inguinal approach should be taken, erring toward orchiopexy rather than orchiectomy. The intention is to maintain the possibility of some residual Leydig cell function. They concluded that prenatal torsions are never salvageable and do not warrant emergent intervention, whereas postnatal torsions sometimes can be corrected, and surgical exploration should be undertaken [7].
Baglaj et al. [8] reviewed testicular torsion patients operated on during 29 years and found 3 cases of bilateral torsion. Two patients initially presented with unilateral scrotal symptoms and one had painless enlargement of both gonads. Interestingly, the study highlights that imaging studies in the newborns with bilateral torsions seem to have less value, especially in asynchronous cases. They often turn out to be inconclusive, so a surgical exploration should be taken in short order [8, 9].
In the case of our patient, during orchiectomy and exploration of the opposite hemiscrotum, ischemia of the right testis was found incidentally. Before the surgery, only one-sided acute scrotal findings were present, and the imaging studies showed no abnormalities in the right side of the scrotum. The probable cause of the ischemia was torsion and spontaneous detorsion of the right testicle. In every case of testicular torsion, interoperative exploration of the opposite hemiscrotum is obligatory to fix the contralateral testis. Our case shows that despite fixation, the atrophy of the gonad can still occur.
Conclusion
Bilateral testicular torsion is a rare event amongst infants; nevertheless, more and more publications considering this problem can be found. There are still single events and no well-established courses of action when such a problem occurs, so it can be quite a challenge for a pediatric surgeon. Nevertheless, the purpose of all actions taken should be to maintain the hormonal function of the affected testicle.
Acknowledgment
The publication was prepared under the project financed from the funds granted by the Ministry of Science and Higher Education in the "Regional Initiative of Excellence" programme for the years 2019-2022, project number 016/RID/2018/19, the amount of funding 11 998121.30 PLN.
References
- John M Gatti, Patrick Murphy J. Ostre choroby jader. Pediatria po dyplomie 13 (2009): 38-45.
- Ibrahim AHM, Ghali AM, Musalam AO, et al. Undescended testes: do we need to fix them earlier?. Ann Pediatr Surg 1 (2005): 21-25.
- Monteilh C, Calixte R, Burjonrappa S. Controversies in the management of neonatal testicular torsion: A meta-analysis. J Pediatr Surg (2018).
- Yerkes EB, Robertson FM, Gitlin J, et al. Management of perinatal torsion: today, tomorrow or never?. J Urol 174 (2005): 1579-1582.
- Frederick PL, Dushku N, Eraklis AJ. Simultaneous bilateral torsion of the testes in a newborn infant. Arch Surg 94 (1967): 299.
- Gorbonos A, Cheng EY. Perinatal testicular torsion in siblings. J Pediatr Urol 3 (2007): 514-515.
- Kaye JD, Levitt SB, Friedman SC, et al. Neonatal torsion: a 14-year experience and proposed algorithm for management. J Urol 179 (2008): 2377-2383.
- Baglaj M, Carachi R. Neonatal bilateral testicular torsion: a plea for emergency exploration. J Urol 177 (2007): 2296-2299.
- Roth CC, Mingin GC, Ortenberg J. Salvage of bilateral asynchronous perinatal testicular torsion. J Urol 185 (2011): 2464-2468.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
