A Tumor Rupture Related to a Vascular Lake During Drug-Eluting Beads Chemoembolization in Hepatocellular Carcinoma: A Case Report
Jinpeng Li1, Congcong shi2, Jutian shi1, Jinlong song1?Nan Wang1*
1Intervention ward one, Shandong Cancer Hospital and Institute, Shandong First Medical University and Shandong Academy of Medical Sciences, Jinan, Shandong, 250117, China
2Shandong Mental Health Center, Jinan, Shandong, 250000, China
*Corresponding Author: Dr. Nan wang, Intervention ward one, Shandong Cancer Hospital and Institute, China
Received: 17 March 2020; Accepted: 27 March 2020; Published: 04 May 2020
Article Information
Citation:
Jinpeng Li, Congcong Shi, Jutian Shi, Jinlong Song, Nan Wang. A Tumor Rupture Related to a Vascular Lake During Drug-Eluting Beads Chemoembolization in Hepatocellular Carcinoma: A Case Report. Archives of Clinical and Medical Case Reports 4 (2020): 336-343.
View / Download Pdf Share at FacebookAbstract
DEBs?Drug-eluting microspheres) is a new embolic agent in recent years, which can achieve the dual effects of embolization and local drug release, and achieve more satisfactory tumor response rate and survival time than C-TACE?conventional transcatheter arterial chemoembolization. VL (vascular lake) was a special complication of embolization of HCC with DEBs. Although it had been reported that the occurrence of VL could predict a satisfactory tumor response rate in the literature, but there was a risk of local tumor residue or tumor rupture, which should be paid more attention to. We report a case of hepatocellular carcinoma with tumor rupture after D-TACE treatment and complete response after (TAE) treatment. A 48-year-old man came to our hospital with liver tumor and clinically diagnosed as hepatocellular carcinoma (HCC). Vascular lake appeared during D-TACE treatment. The patient developed abdominal pain the second day after embolization, and was diagnosed as hepatocellular carcinoma rupture by abdominal puncture. Then selective TAE was performed. After TAE, the elevated tumor marker liver level (3008 ng/mL) decreased to the normal level. According to the mRECIST [4], the curative effect was evaluated as partial remission contrast baseline disease. During the follow-up to January 2020, the patient still had no recurrence of the disease, the quality of life was good, and the side effects of targeted drugs were mild.
Keywords
<p>Drug-eluting microspheres; Vascular lake; Spontaneous rupture; Hepatocellular carcinoma</p>
Article Details
1. Introduction
Transcatheter arterial chemoembolization (TACE) was the most widely used local treatment for unresectable hcc. With the rapid development of interventional medicine, the choice of embolic materials for liver cancer was becoming more and more extensive, and embolic microspheres gradually had the same important status as lipiodol [1]. When using embolic microspheres, the occasional phenomenon of "vascular lake" during operation often attracted the attention of clinicians. The incidence of the VL in DEB-TACE was poorly described in the literature, and many literatures had pointed out that the occurrence of VL could predict a satisfactory tumor response rate, but there was a risk of tumor rupture [2]. Due to the erosion and displacement of the microspheres with the redistribution of blood flow, the embolization was not complete, and the VL gradually expanded until ruptured with the increase of intratumoral blood pressure. Rupture of the tumor with subsequent intraperitoneal hemorrhage is a life-threatening condition. In patients diagnosed with HCC, rupture occurs in 3~15%, with a high in-hospital mortality rate of 25~75%. Because most of the patients treated with TACE were advanced liver cancer, the liver function was poor, and the rupture of liver cancer progressed rapidly, large amount of bleeding, most patients had no chance of surgical hemostasis [3]. At this time, TAE often become the preferred method to stop bleeding, but the success rate and effect of TAE were not very ideal because of various factors such as difficult to identify bleeding vessels.
Here we report the case of ruptured hepatocellular carcinoma in which the vascular lake phenomenon emerged during the D-TACE procedure and caused an intratumoral arteriovenous shunt, playing the most important role in its occurrence. We also discussed the mechanism of tumor rupture associated with VL and technical considerations to avoid this serious complication. We also provided a review of the literature.
2. Case Report
A 46-year-old male was admitted our hospital for "recurrent epigastric pain for 2 months". The patient was in good health and had no family history of tumor, but the history of hepatitis B was more than 10 years. Abdominal CT showed that an inhomogeneous mixed density lesion was seen in the left and right lobe of the liver, with a maximum diameter of about 10.4 cm × 8.5 cm. The lesion was obviously enhanced in arterial phase, and the portal vein and delayed phase were cleared rapidly (Figure 1). It was diagnosed as massive hepatocellular carcinoma and liver cirrhosis. Blood tumor markers: Carbohydrate antigen 19-9 (CA19-9) 46.35 U/mL (0~39 U/mL), Carcinoembryonic Antigen (CEA) 2.12 ng/mL (0~5 ng/mL), alpha-fetoprotein (AFP) 599 ng/ml (0~7.02 ng/mL)).
The patient had Child-Pugh A liver function, blood routine test and renal function were normal. Combined with the imaging findings and the history of chronic hepatitis B, the clinical diagnosis was considered as primary liver cancer. After multidisciplinary consultation in the hospital and full evaluation of the patient's condition, the final treatment plan was: TACE combined with sorafenib targeted therapy, while receiving antiviral therapy. Combined with the wishes and economic status of the patients, the patients received D-TACE treatment. Before operation, the patient signed the relevant treatment informed consent form and implantable medical material list.
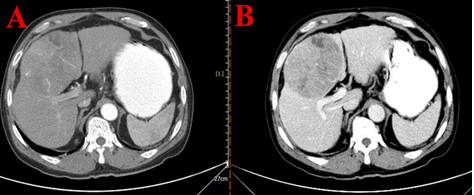
Figure 1: Computed tomography of the abdomen. The axial plane (A) as well as the portal vein plane; (B) in the computed tomography scan of the abdomen showed a hepatic tumor (asterisk) with 10.4 cm diameter.
On May 7, 2019?the patients were treated with D-TACE. Seldinger technique was used to puncture the femoral artery. Using coaxial catheter technique, 2.7F Progreat microcatheter (Terumo, Japan) was super selectively intubated into the tumor feeding artery. DSA angiography showed a mass of tumor staining at the junction of the left and right lobes of the liver. The tumor blood supply target was super selected by SP microcatheter and embolized by drifting lipiodol 8 mL?then tee was preferred to connect 1ml syringe with 20 ml syringe containing CalliSpheres drug loaded microspheres (100~300um) + epirubicin 60mg+ contrast agent. 1 ml syringe was used to connect the microcatheter and pulse injection at the speed of 1 ml/min. When the flow rate of the mixture was slow to stop, the embolization could be stopped, and the angiography could be continued after waiting for 5 min. The phenomenon of vascular lake could be seen by dsa angiography again, and showed an increasing trend, followed by embolization with callisSphere 500-700um blank microspheres, until the blood flow slowly tended to stop embolization, and the operation was terminated. The patient had no adverse reactions such as chest tightness, chest pain and lower limb discomfort during the operation and returned to the ward safely.
After operation, patients were given symptomatic treatment such as liver protection, antiemetic, acid inhibition, analgesia and so on. On the second day after operation, the patient showed hemorrhagic shock such as unbearable abdominal pain, shortness of breath, increased pulse rate and continuous decrease of blood pressure; Non-coagulable blood was drawn by abdominal puncture, and emergency blood examination showed that hemoglobin 132 g/L decreased to 92 g/L. Combined with the above clinical manifestations and examination results, it was diagnosed as tumor rupture and bleeding. Hemostatic drugs were given immediately, and hepatic artery embolization was performed in emergency. During the operation, it was found that the hepatic artery and its branches contracted obviously, while the vascular lake in the tumor showed an enlarged trend, accompanied by spillover of contrast medium. Super selective intubation was given to the feeding artery for gelatin sponge embolization, and good embolization could be seen in re-angiography. After operation, the bleeding symptoms stopped, the blood pressure was stable, and the hemoglobin 98 g/L was reexamined. After recovery, he was successfully discharged from the hospital and was given oral sorafenib 400 mg PO BID targeted therapy. During the follow-up 2 months after operation, abdomen CT examination showed that the liver lesions were significantly smaller than before, and there was no obvious enhancement on contrast-enhanced scan (Figure 2), the level of alpha-fetoprotein dropped to the normal range (7 ng/ml). According to the mRECIST [4], the curative effect was evaluated as partial remission contrast baseline disease (Figure 3). During the follow-up to January 2020, the patient still had no recurrence of the disease, the quality of life was good, and the side effects of targeted drugs were mild.
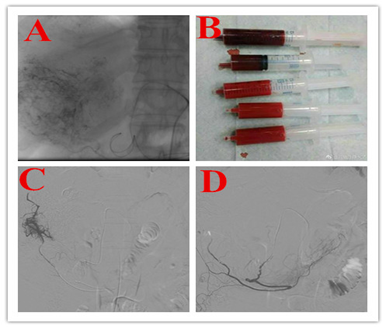
Figure 2: Transarterial embolization. After puncture of the right femoral artery, a catheter was advanced via the celiac trunc into the common hepatic artery, and the segmental arteries IV and V were selectively embolized with particles (Embosphere 100-300 μm). A highly vascularized tumor without active bleeding is shown in angiography before embolization (a) in segment IV. After tumor embolization, the former hyper vascularity of the tumor is absent (b).
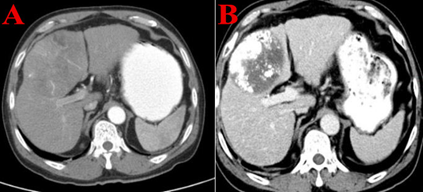
Figure 3: The follow-up Computed tomography of the abdomen. Before interventional therapy: The axial plane (A) in the computed tomography scan of the abdomen showed a hepatic tumor (asterisk) with 10.4 cm diameter. 2 months after interventional therapy: The abdomen showed a hepatic tumor (asterisk) with 7.4 cm diameter, According to the mRECIST, the curative effect was evaluated as partial remission contrast baseline disease.
3. Discussion
Most of the patients are in the middle and advanced stage and lost the opportunity of surgical resection. TACE has become the first choice for non-operative treatment of advanced hepatocellular carcinoma, which can significantly prolong the survival time of patients [5]. With the rapid development of interventional medicine, the choice of embolic materials for liver cancer is becoming more and more extensive, and embolic microspheres gradually have the same important status as lipiodol. A characteristic phenomenon (vascular lake) was found when using embolized microspheres?in the process of embolization, it can be seen that the contrast agent accumulates in the tumor area as a pool and lasts until the venous phase. VL is a special complication of DEBs embolization in the treatment of HCC [6]. It has been reported in the literature that the emergence of VL can predict a satisfactory tumor response rate.
However, if the VL phenomenon is not handled properly, there may be a risk of tumor rupture and bleeding. However, there is no guideline for the management of VL during the procedure and insufficient information about VL-associated complications, including tumor rupture [3]. The incidence of vascular lake is 12.1% ~ 25.5% (calculated by focal nodules) reported in the literature [6, 7]. The cause of the formation of VL is unknown. VL does not appear in angiography, but only occurs in the process of DEBs embolization. Seki et al. [2] analyzed the formation process of VL as follows: when DEBs slowly enters the tumor blood vessels with blood flow, DEBs does not evenly enter into all tumor blood vessels, causing changes in blood pressure and blood flow redistribution in the tumor. Due to the lack of muscle layer in the immature tumor blood vessel wall, the blood pressure in the tumor slowly increases with the injection of the microspheres, which can cause rupture of the unembolized tumor blood vessels. The contrast medium spills over into the tumor parenchyma, resulting in intratumoral rupture and bleeding, similar to the "tumor stroke" type in ruptured liver cancer [8].
Some scholars analyze the high risk factors of VL formation in the process of DEBs treatment of HCC [9, 10]. Seki et al. [2] reported that tumor diameter >3 cm and dose of beads used ≥10 mg were independent risk factors for VL and Cavalcante [6] reported: the predictors of VL include pseudocapsule, tumor diameter >3 cm and increased tumor marker AFP. During radiography, the vascular lake is divided into stable and unstable according to its shape (whether it is enlarged or not) and its position (whether it is close to the surface of the liver).The study showed that the phenomenon of "vascular lake" was more likely to occur in larger tumors. 84.8% of the tumors with "vascular lake" phenomenon occurred in tumors with a diameter greater than 3 cm. The incidence of "vascular lake" in tumors with a diameter greater than 3 cm was 38.9% (28/33), while the incidence of "vascular lake" in tumors with a straight diameter less than 3 cm was only 2.5% (5/198) [11]. And there was a risk of tumor rupture near the surface of the liver. In this study, we reported a patient with advanced HCC whose tumor size was about 10.4 cm × 8.5 cm (3 cm), located at the edge of the hepatic capsule, most of which protrude to the surface. The tumor with this characteristic is fragile because of its thin capsule and the phenomenon of vascular lake is easy to occur in the process of embolization. If the tumor is not handled properly, the tumor is easy to rupture and bleed spontaneously or after being subjected to a slight external force. After D-TACE, the end of the feeding artery of the tumor is widely embolized, which makes the tumor necrotic and liquefied, which increases the internal pressure of the tumor and is more likely to lead to rupture and bleeding.
At present, there is no clear standard for the treatment of VL, more for the operator's experience. Seki et al. [2] reported the VL with stable or continuous enlargement after DEBs treatment was embolized with gelatin sponge until the VL disappeared, while the cases with reduced VL after DEBs treatment were not further treated. In the course of actual operation, unstable VL is continued to embolize with DEBs, blank microspheres or gelatin sponge until achieved. SACE ? grade embolic end point [12]; For stable VL, if there is no change in size after multiple radiography, it can be followed up and observed. In this patient, liver rupture and bleeding was caused by unstable VL [13]. Due to the use of DEBs embolization and lipiodol during the treatment, the microspheres may be scoured and shifted along with the redistribution of blood flow due to their small size and fast blood flow velocity, resulting in incomplete embolization. VL gradually enlarged and ruptured with the increase of intratumoral blood pressure.
The principle of treatment for rupture and bleeding of liver cancer after TACE is rapid and effective hemostasis combined with antishock therapy. Because most of the patients treated TACE are advanced liver cancer, the liver function is poor, and the rupture of liver cancer progresses rapidly, and the amount of bleeding is large, there is no chance of surgical hemostasis in most cases. At this time, TAE often becomes the preferred method to stop bleeding, but the success rate and effect of TAE are not very ideal because of various factors such as difficult to identify bleeding vessels. Once hepatocellular carcinoma patients have tumor rupture and bleeding, there is a risk of intraperitoneal implantation and metastasis, the timely use of targeted drug therapy can significantly improve the therapeutic effect of the patients. In this paper, after the rupture and bleeding of liver cancer, the patients were treated with emergency interventional embolization and targeted therapy with sorafenib after operation, and the clinical effect was partially relieved [14].
In conclusion, the occurrence of rupture and hemorrhage of hepatocellular carcinoma after d-TACE may be related to clinical factors such as large diameter of tumor, located at the edge of liver, protruding surface growth, no use of solid embolic material and so on. Although this complication is rare, some patients can get a good prognosis after active treatment. Therefore, strengthening embolization with granular materials after embolization of drug-loaded microspheres may reduce the risk of rupture and bleeding to a certain extent when patients with liver cancer with vascular lake are treated with D-TACE. At the same time, postoperative monitoring of this kind of patients must be strengthened in order to detect and treat them as soon as possible.
Sources of Funding
This article is supported by Wu Jieping Foundation (320.6750.19088-23).
Ethical Approval
No ethical clearance required as it only involves case report.
Consent
Written informed consent was obtained from the patient.
Author’s Contributions
Involvement in managing the patient-LJP, WN, SJL.
Data collection- SCC, WN.
Manuscript editing -LJP,SJT.
Guarantor
Wangnan
Provenance and Peer Review
Editorially reviewed, not externally peer-reviewed.
Declaration of Competing Interest
The authors have no conflict of interests to declare.
Acknowledgements
No.
References
- Liu YS?Lin CY?Chuang MT?et al? Five-year outcome of conventional and drug-eluting transcatheter arterial chemoembolizational in patients with hepatocellular carcinoma. BMC Gastroenterology 18 (2018): 124-132?
- Seki A?Hori S?Shimono C?Management of vascular lake phenomenon on angiography during chemoembolizational with superabsorbent polymer microspheres. JPN J Radio 33 (2015): 741-748?
- Aoki T, Kokudo N, Matsuyama Y, et al. Prognostic impact of spontaneous tumor rupture in patients with hepatocellular carcinoma: an analysis of 1160 cases from a nationwide survey. Ann Surg 259 (2014): 532?
- Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis 30 (2010): 52-60.
- Seki A?Hori S?Kobayashi K?Transcatheter arterial chemoembolizational with epirubicin-loaded superabsorbent polymer microspheres for 135 hepatocellular carcinoma patients:single-center experience?Cardiovasc Intervent Radiol 34 (2011): 557-565?
- Cavalcante RN?Nasser F?Motta JM?et al? Occurrence of vascular lake phenomenon as a predictor of Improved tumor response in HCC patients that underwent DEB-TACE. Cardiovasc Intervent Radiol 40 (2017): 1044-1051?
- Crespi S?Martinetti L?Nicolini A? Outcome of HCC patients Presenting pooling phenomenom during TACE?Cardiovasc Intervent Radiol 36 (2013): S323-328?
- Malagari K, Pomoni M, Moschouris H, et al. Chemoembolization of hepatocellular carcinoma with HepaSphere 30-60 µm. Safety and efficacy study.Cardiovasc Intervent Radiol 37 (2014): 165-75.
- Raoul JL, Sangro B, Forner A, et al. Evolving strategies for the management of intermediate-stage hepatocellular carcinoma: available evidence and expert opinion on the use of transarterial chemoembolization. Cancer Treat Rev 37 (2012): 212-220.
- Crespi S, Martinetti L, Nicolini A. Outcome of HCC patients presenting pooling phenomenom during TACE. Cardiovasc Intervent Radiol 36 (2013): S323.
- Osuga K, Hori S, Hiraishi K, et al. Bland embolization of hepatocellular carcinoma using superabsorbent polymer microspheres. Cardiovasc Intervent Radiol 31 (2008): 1108-1116.
- Jin B?Wang DX?Lewandowski RJ?et al? The Impact of Chemoembolization Endpoints on Survival in Hepatocellular Carcinoma Patients. AJT 196 (2011): 919-928?
- Kong Jian?Zhang Yanfang?Li Yong?et al?Drug-Eluting Beads Chemoembolization in the Treatment of Hepatocellular Carcinoma:The Management of Vascular Lake Phenomenon. Journal of Clinical Radiology 7 (2019): 1312-1315.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
