Telemedicine-Guided Stroke Thrombolysis in a COVID-19 Patient Admitted in a Field Hospital
Tarso A. D. Accorsi*, Alexandra R. D. Brigido, Fabio C. Habrum, Flavio A. de Carvalho, Karine De Amicis Lima, Carlos H. S. Pedrotti, Eduardo Cordioli
Telemedicine Department, Hospital Israelita Albert Einstein, Sao Paulo, Brazil
*Corresponding Author: Dr. Tarso A. D. Accorsi, Telemedicine Department, Hospital Israelita Albert Einstein, Sao Paulo, Brazil
Received: 20 May 2020; Accepted: 03 June 2020; Published: 15 July 2020
Article Information
Citation:
Tarso A. D. Accorsi, Alexandra R. D. Brigido, Fabio C. Habrum, Flavio A. de Carvalho, Karine De Amicis Lima, Carlos H. S. Pedrotti, Eduardo Cordioli. Telemedicine-Guided Stroke Thrombolysis in a COVID-19 Patient Admitted in a Field Hospital. Archives of Clinical and Medical Case Reports 4 (2020): 690-698.
View / Download Pdf Share at FacebookAbstract
Telemedicine might be crucial during the current pandemic, helping in re-structuring the health system. This paper is a case report of a COVID-19 patient admitted to a field hospital who presented an infection-triggered ischemic stroke. She was examined by allocated general practitioners and had a life-threatening situation. The correct application of treatment guidelines is a challenge in this scenario and the feasibility of telemedicine-guided treatment is still uncertain. This report aims to demonstrate the effectiveness of teleconsultation in an emergency. There was a retrospective data compilation from the patient's medical record and subsequent exposure of the main findings. The patient presented typical viral pneumonitis on chest CT scan, she was on supportive treatment and presented acute neurological deficit on the tenth day after respiratory manifestation. Immediate skull CT scan did not show blood and there was stippling in sylvian branches of a left middle cerebral artery. There was telemedicine-guided confirmation of the diagnosis, tomographic interpretation, decision-making, and thrombolytic administration. There is a demonstration of the feasibility of teleconsultation in a time-effective manner, reinforcing the need to expand the telemedicine program in multiple scenarios.
Keywords
<p>Telemedicine; Stroke; Pandemics; Referral; Consultation</p>
Article Details
1. Introduction
Telemedicine has become essential during the current COVID-19 pandemic due to its cost-effective and safely-quickly capacity to evaluate patients in multiple situations [1]. The exponential COVID-19 incidence increase has implied new severe cases and reorganization of the health system [2]. Field hospitals were built and massive physician recruitment was carried out. The frontline medical team is usually heterogeneous in training and experience [3]. Admitted patients with COVID-19 acute respiratory distress evolve with twelve media days of hospitalization and multiple systemic complications, including thrombotic events such as stroke [4, 5]. Stroke treatment is related to a better prognosis, but presumably in field hospitals, the management of these patients is more difficult [6]. In this scenario, teleconsultation is an efficient method to increase access to specialists with decision support in life-threatening situations [7].
This is an in-edit case of telemedicine-guided stroke thrombolysis in a COVID-19 patient. This report was approved by our local institutional Ethics Committee. The enrolled patient was admitted to Pacaembu Pandemic Field Hospital (São Paulo, Brazil) with access to the emergency telemedicine service of Hospital Israelita Albert Einstein (São Paulo, Brazil) through a portable system.
2. Materials and Methods
2.1. Case presentation
A 60-year-old female patient was admitted for respiratory distress. After presenting with seven days of fever, myalgia and prostration, intense dry cough, odynophagia, anosmia, and ageusia, the patient sought basic governmental health service and was referred due to COVID-19-presumed pneumonia with desaturation. Her past medical history was relevant for systemic arterial hypertension, hypothyroidism, and resolved laryngeal neoplasia. She had not been vaccinated against influenza during the last flu season. On admission, she was neurologically and hemodynamically stable. Her hypoxemia was resolved after 50% oxygen therapy, and the chest radiography showed bilateral interstitial infiltrate (Figure 1).
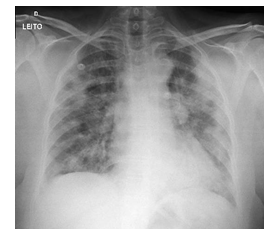
Figure 1: Anteroposterior chest radiography (bilateral interstitial infiltrate).
The chest CT scan revealed multiple ground-glass pulmonary opacities sometimes associated with thickening of the interlobular septa and fine intermingled septa in addition to sparse consolidation foci, presenting bilateral multifocal distribution and peripheral and posterior predominance. There was a greater extension in the lower lobes with an estimated extension of pulmonary involvement greater than 50% (Figure 2).
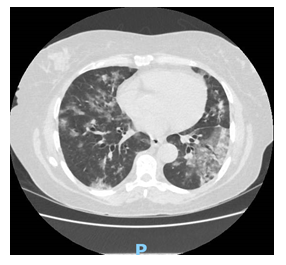
Figure 2: Axial mid-thorax CT scan (multiple ground-glass pulmonary opacities).
COVID-19 infection was reinforced and PCR for SARS-CoV-2 and influenza collected. Laboratory tests showed leukocytosis with neutrophilia, high C-reactive protein, and platelets, and D-dimer drew attention (Table 1: admission).
|
Laboratory tests |
Admission |
Stroke onset |
Two days after stroke |
Normal range |
|
Hb |
10.2 |
10 |
8.9 |
12-15.5 mg/dL |
|
Ht |
29.2 |
28.7 |
28 |
35-45 % |
|
WBC |
16.6 |
11.6 |
11.5 |
3.5-10.5 x 10³ /μL |
|
PLT |
51.6 |
61.4 |
52.7 |
15-45 x 104 /μL |
|
CRP |
412 |
150 |
71.6 |
< 3 mg/L |
|
BUN |
16.3 |
12.6 |
12.6 |
7-18.2 mg/dL |
|
SCr |
0.98 |
0.89 |
0.76 |
0.55-1.02 mg/dL |
|
Na |
133 |
133 |
143 |
135-145 mEq/L |
|
K |
4.2 |
3.8 |
3.8 |
3.5-5.5 mEq/L |
|
D-dimer |
1649 |
1627 |
1720 |
< 500 ng/mL |
|
cTnT |
12 |
10 |
- |
< 5 pg/mL |
|
LDH |
428 |
- |
- |
135-214 U/L |
|
Blood glucose |
- |
119 |
135 |
70-100 mg/dL |
|
ALT |
28 |
31 |
- |
19-25 U/L |
|
AST |
11 |
14 |
- |
9-32 U/L |
|
pH |
7.44 |
7.48 |
7.42 |
7.35-7.45 |
|
PaO2 |
101 |
128 |
- |
> 80 mmHg |
|
PaCO2 |
36.5 |
35.5 |
- |
35-45 mmHg |
|
HCO3 |
25.1 |
26.8 |
30.6 |
22-26 mEq/L |
|
SaO2 |
97.5 |
98.6 |
- |
> 94% |
|
BE |
1.4 |
3.4 |
5.9 |
-3 to +3 mmol/L |
|
AG |
9.6 |
15.2 |
- |
10-14 mEq/L |
|
Arterial lactate |
13 |
12 |
- |
< 18 mg/dL |
Hb=hemoglobin; Ht=hematocrit; WBC=white blood cell; PLT=platelet; CRP=C-reactive protein; BUN=blood urea nitrogen; SCr=serum creatinine; Na=sodium; K=potassium; cTnT=cardiac troponin T; LDH=lactate dehydrogenase; ALT=alanine aminotransferase; AST=aspartate aminotransferase; PaO2=partial pressure of arterial oxygen; PaCO2=partial pressure of carbon dioxide; HCO3=bicarbonate concentration; SaO2=arterial oxygen saturation; BE=base excess; AG=anion gap
Table 1: Inpatient laboratory data.
Initial therapy comprised ceftriaxone, azithromycin, oseltamivir, and hydroxychloroquine. She was on amlodipine and had stable blood pressure. The PCR confirmed COVID-19 infection. On the tenth day after the onset of symptoms third day of hospitalization, the patient presented with sudden right hemiplegia and aphasia without loss of consciousness. The neurological deficit was promptly recognized by the general practitioner, and immediate evaluation in the emergency room was conducted. Initial blood pressure was 100/70 mmHg and quickly increased to 170/100 mmHg. The heart rate was 114 bpm, SatO2 95% on 2 L/min nasal, and capillary glycemia 98 mg/dL; EKG was normal. New blood tests were provided (Table 1: stroke onset). Telemedicine evaluation was performed after 10 minutes and immediate skull CT was requested. After 30 minutes, the CT was available (Figure 3).
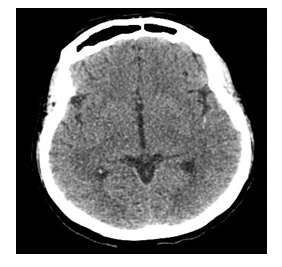
Figure 3: Skull CT scan (no blood and stippling in sylvian branches of the left middle cerebral artery - red arrow).
Telemedicine radiological and neurological assessment of CT concluded no hemorrhagic stroke or stippling in sylvian branches of the left middle cerebral artery. Acute ischemic stroke was in progress with 45 minutes deficit; telemedicine-performed NIHSS was 12 with a checklist without thrombolysis contraindication. The patient care team administered specific treatment and telemedicine-guided thrombolysis with 0.9 mg/kg IV alteplase, 10% in bolus, and 90% in 1h. There was on-site and telemedicine patient monitoring. No side effects occurred. After thrombolysis, the patient was referred to a step-up COVID-19 reference hospital. A posteriori evaluation of cervical and cranial vessel angiotomography revealed diffuse atherosclerotic degeneration and the presence of non-adherent hypoattenuating thrombus in the left common carotid artery (0.5 cm × 1.9 cm thickness) (Figure 4).

Figure 4: Coronal cervical angiotomography (non-adherent hypoattenuating thrombus in the left common carotid artery).
Besides, the CT showed the right common carotid artery kinking, multiple calcified and non-calcified parietal plaques in the common carotid arteries, and carotid bulbs in the origins of the internal carotid arteries without determining significant stenosis but with deep ulcerations. Occlusion of the upper M2 branch and distal left M3 segment with a paucity of collateral network downstream ipsilateral was also observed. In the subsequent two days, the patient’s NIHSS improved to 9, maintaining right hemiparesis, and aphasia of predominant motor evolved and remained hemodynamically, respiratory and laboratory stable (Table 1: Two days after stroke). A new angiotomography performed 48 hours after thrombolysis revealed carotid thrombus and an incidental finding of filling defects compatible with acute pulmonary thromboembolism in posterior subsegmental arteries of the right upper lobe. Thus, weighing the risks and benefits, anticoagulation was initiated. The patient remains hospitalized in rehabilitation with progressive recovery.
3. Discussion
Since the COVID-19 outbreak, several case series have been published describing the disease’s profile [4, 6, 8]. Despite pulmonary involvement and respiratory distress in most hospitalized patients, the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection can also be associated with renal, cardiac, hepatic, and neurologic complications [4]. Furthermore, the long duration of hospitalization increases the risk of secondary bacterial infections, gastrointestinal bleeding, and thromboembolic events [8]. A retrospective multicenter cohort China study enrolled 191 COVID-19 hospitalized patients and showed a high average hospital stay: 12 days (range 9-15) in survivors, 7.5 days (range 11-15) in non-survivors, 8 days (range 4-14) in survivors in intensive care units (ICU) and 7 days (range 2-9) in non-survivor ICU patients [4].
Regarding neurologic COVID-19 patient affection, two studies from Wuhan, China, including 214 and 221 patients, revealed a 2.8% and 5% stroke incidence, respectively.9,10 In the study conducted by Li et al. 2020, 11 patients had an ischemic stroke and among these, five were related to large artery disease, three small artery disease, and three cardioembolic events. The median duration to the onset of stroke after COVID-19’s first symptoms was 10 days (interquartile range 1-29 days), but neurological symptoms were also related to its initial presentation. Cerebrovascular events were more frequent in older patients (median age of 71.6 years in the stroke group) with severe disease and stroke risk factors such as hypertension, diabetes, coronary artery disease, and previous cerebrovascular disease. A higher frequency of hepatic and renal dysfunction during hospitalization was also found [4, 10].
We report a case of a COVID-19 female inpatient whose clinical profile is very similar to the one described by the studies: a sixth decade of life, comorbidities, and clinical worsening on the seventh day of infection. Our patient had a chronic risk factor (hypertension) and acute COVID-19 manifestations that possibly triggered her stroke on the tenth day of symptoms exactly like the median cited. On the other hand, the underlying causes related to a high risk of developing acute stroke observed in COVID-19 patients, especially in those with multiple organ dysfunctions, remain unclear. Potential mechanisms of how this disease increases stroke risk have been described but not yet proven [8, 11]. An increased risk of acute ischemic stroke has also been noted in patients with other respiratory tract infections [12]. Elevated CRP indicating high inflammatory state, a hallmark of severe disease, and abnormalities of coagulation cascade as evidenced by increased D-dimer levels might play a role in strokes with COVID-19 infection [11-13]. Recent autopsy data suggests thrombotic microangiopathy in multiple organs, especially in the lungs, but no brain autopsy reports are currently available [14, 15].
Despite the numerous publications during the last few months, COVID-19 is an emerging disease and still, now there is no certain treatment based on RCT related to significant better prognosis [16]. In the case described, the patient initially received antimicrobials directed at community-acquired pneumonia that could be associated with COVID-19 pneumonia in addition to antiviral treatment for possible influenza, while her radiographic and tomographic findings were extremely suggestive of COVID-19 pneumonia. As COVID-19 infection appears to be a risk factor itself for stroke, a life-threatening condition, well-established protocols to make a quick diagnosis and correctly treat this complication are essential for patients’ recovery [12, 17, 18]. After all, in this scenario, there is no defined stroke prophylactic strategy beyond support interventions such as adequate mechanical ventilation when necessary and early and correct treatment of COVID-19 emergent complications [12, 16].
In the present case, the COVID-19-related ischemic stroke was promptly recognized and first attended by a general practitioner, but the measurement of neurological deficit, radiographic image interpretation, and specific treatment was specialist telemedicine guided. Up to this point, the patient did not require advanced airway and was safely treated by a field hospital general practitioner following institutional protocols. Only after thrombolysis, she was transferred to an intensive care unit at a tertiary center. Otherwise, in a field hospital, that represents the saturation of the health system, general practitioners might have several doubts regarding stroke management and presumably, they would seek decision support. In the era of increasing health care costs, telemedicine is a low-cost resource that represents optimal high-value care [19]. A review of the Cochrane Library and Centre for Review and Dissemination confirmed that telemedicine is cost-effective for being applied in major medical fields [20].
There was already evidence of telemedicine helping compensate for many conditions with improvement in overall mortality and hospitalization [21]. Teleconsultation is also an efficient way to reduce the lack of specialists to provide care, including in-patients [20, 22]. In addition to diagnostic aid and therapeutic safety, telemedicine can also be useful to interpret emergency radiographic images [23]. The telemedicine strategy used to conduct a COVID-19 complication illustrates that the pandemic is changing the way we deliver care and has highlighted the enormous potential of telemedicine in stroke care. This case reinforces the need to expand the effort of teleconsultation in the emergency field. Besides, the acute neurological event presented points the need for continuous monitoring of critically ill patients and a structure for emergency care in field hospitals [24].
4. Conclusion
COVID-19 pandemic has forced the health system to structure. Telemedicine is a low-cost easy tool facilitating better prognosis of life-threatening situations such as COVID-19-induced stroke.
Acknowledgments
We would like to thank the "Instituto Israelita de Responsabilidade Social Albert Einstein (IIRS)" and the telemedicine Hospital Israelita Albert Einstein emergency medical team: Deborah de Sa P. Belfort, Fernando G. Scarpanti, Iuri R. Magalhaes, Jose R. de O. Silva Filho, Leon P. C. Sampaio, Maria T. S. de S. Lira, and information technology support for the relevant services provided.
Conflicts of Interest Statement
The authors declare they have no conflicts of interest.
References
- Loeb AE, Rao SS, Ficke JR, et al. Departmental Experience and Lessons Learned With Accelerated Introduction of Telemedicine During the COVID-19 Crisis. J Am Acad Orthop Surg (2020).
- Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed (2020).
- Secretaria Especial de Comunicação. Hospital de Campanha do Pacaembu começa a funcionar na próxima semana. São Paulo, 27 de mar. de (2020).
- Guan WJ, Ni ZY, Hu Y, et al. China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 382 (2020): 1708-1720.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395 (2020): 497-506.
- Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. Jama (2020).
- Kuehn BM. Telemedicine Helps Cardiologists Extend Their Reach. Circulation 134 (2016): 1189-1191.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395 (2020): 1054-1062.
- Mao L, Jin H, Wang M, et al. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol (2020): e201127.
- Li Y, Wang M, Zhou Y, et al. Acute Cerebrovascular Disease Following COVID-19: A Single Center, Retrospective, Observational Study.
- Tan CW, Low JGH, Wong WH, et al. Critically Ill COVID-19 Infected Patients Exhibit Increased Clot Waveform Analysis Parameters Consistent with Hypercoagulability. Am J Hematol (2020).
- Qureshi AI, Abd-Allah F, Alsenani F, et al. Management of Acute Ischemic Stroke in Patients with COVID-19 Infection: Report of an International Panel.
- Ye Q, Wang B, Mao J. The Pathogenesis and Treatment of the `Cytokine Storm' in COVID-19. J Infect (2020).
- Fox SE, Akmatbekov A, Harbert JL, et al. Pulmonary and Cardiac Pathology in Covid-19: The First Autopsy Series from New Orleans. medRxiv (2020).
- Yao XH, Li TY, He ZC. A pathological report of three COVID-19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi 49 (2020): E009.
- Ye Q, Wang B, Mao J. The Pathogenesis and Treatment of the `Cytokine Storm' In COVID-19. J Infect (2020).
- Khosravani H, Rajendram P, Notario L, et al. Protected Code Stroke: Hyperacute Stroke Management During the Coronavirus Disease 2019 (COVID-19) Pandemic. Stroke (2020): STROKEAHA120029838.
- Smith MS, Bonomo J, Knight WA 4th, et al. Endovascular Therapy for Patients With Acute Ischemic Stroke During the COVID-19 Pandemic: A Proposed Algorithm. Stroke (2020): STROKEAHA120029863.
- Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med (2020).
- Dierckx R, Inglis SC, Clark RA, et al. Telemedicine in heart failure: new insights from the Cochrane meta-analyses. Eur J Heart Fail 19 (2017): 304-306.
- Lopes MACQ, Oliveira GMM, Ribeiro ALP, Guideline of the Brazilian Society of Cardiology on Telemedicine in Cardiology 2019. Arq Bras Cardiol 113 (2019): 1006-1056.
- Delgoshaei B, Mobinizadeh M, Mojdekar R, et al. Telemedicine: A systematic review of economic evaluations. Med J Islam Repub Iran 31 (2017): 113.
- Weinstein RS, Krupinski EA, Doarn CR. Clinical Examination Component of Telemedicine, Telehealth, mHealth, and Connected Health Medical Practices. Med Clin North Am 102 (2018): 533-544.
- Sellner J, Taba P, Öztürk S, et al. The need for neurologists in the care of COVID-19 patients. Eur J Neurol (2020).


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
