Five Steps to Success - Advanced Interdisciplinary Endoscopic Therapy in a Case of an Intrathoracic Insufficiency of the Esophagogastrostomy and the Development of a Significant Esophagobronchial Fistula
Dörte Wichmann1*, Dietmar Stüker1, Karolin Thiel1, Helene Häberle2, Felicitas Ruckh3, Emanuel Zerabruck3, Michael Böckeler4, Jürgen Hetzel4
1Department of General, Visceral and Transplantation Surgery, University Hospital Tübingen, Germany, Hoppe-Seyler-Strasse 3, 72076 Tübingen, Germany
2Department of Anesthesia and Intensive Care Medicine, University Hospital Tübingen, Germany, Hoppe-Seyler-Strasse 3, 72076 Tübingen, Germany
3Interdisciplinary Endoscopic Unit at the University Hospital of Tuebingen, Germany, Hoppe-Seyler-Strasse 3, 72076 Tübingen, Germany
4Department of Internal Medicine VIII, Pneumology, University Hospital Tübingen, Germany, Ottfried-Müller-Strasse 14, 72076 Tübingen, Germany
*Corresponding Author: Dr. Dörte Wichmann, Department of General, Visceral and Transplantation Surgery, University Hospital Tübingen, Germany, Hoppe-Seyler-Strasse 3, 72076 Tübingen, Germany
Received: 03 April 2020; Accepted: 20 April 2020; Published: 15 May 2020
Article Information
Citation: Dörte Wichmann, Dietmar Stüker, Karolin Thiel, Helene Häberle, Felicitas Ruckh, Emanuel Zerabruck, Michael Böckeler, Jürgen Hetzel. Five Steps to Success - Advanced Interdisciplinary Endoscopic Therapy in a Case of an Intrathoracic Insufficiency of the Esophagogastrostomy and the Development of a Significant Esophagobronchial Fistula. Archives of Clinical and Medical Case Reports 4 (2020): 444-450.
View / Download Pdf Share at FacebookAbstract
Introduction: Endoscopic negative pressure therapy (ENPT) is an effective new method to treat patients with anastomotic insufficiencies of the upper gastrointestinal tract. Development of an esophagobronchial fistula in situation of postesophagectomy anastomotic insufficiency is a rare but challenging and potentially life-threatening complication. In cases of contact to the respiratory tract ENPT is non-operatively because of air leakage.
Case Report: We report about a patient with a bronchial fistula going out from an esophago-mediastinal cave caused by an anastomotic insufficiency. Five steps to an optimal endoscopic treatment were needed. Finally a combination of endobronchial stenting and active drainage of the mediastinal cave and the stomach was used.
Discussion: Successful outcome in this case is attributable to good interdisciplinary communication of all attending physicians and the imaginative combined usage of endoscopic devices.
Keywords
<p>Postoperative complication management; Endoscopic negative pressure therapy; Esophagobronchial fistula</p>
Article Details
1. Introduction
Patients with esophageal carcinomas or carcinomas of the esophageal gastric junction are critical patients because of low nutritional status, passed chemotherapy and visceral surgery with one or two cave resections [1]. Anastomotic leaks are considered to be a predominant reason for tracheobronchial fistulas following esophagectomy [2]. Leakage of intrathoracic anastomosis complicated by a tracheobronchial fistula is a devastating situation. Persisting contamination of respiratory system, mediastinum and pleural cavity results in rapidly progressing septic disease. A stent-based therapy to cover the fistula is possible.
Endoscopic treatment concepts for intrathoracic anastomotic insufficiencies are stent-based, to cover the leak, or endoscopic negative pressure therapy (ENPT) to use an active drainage of an existing cave with endoluminally or intracavitarily placement of the open-pore device [3-5]. Open-pore devices are polyurethane foam drainages or handmade open-pore film drainages (OFD). This device was introduced by G. Loske [6-8]. An open-pore film (Suprasorb CNP® Drainage Film, Lohmann & Rauscher International, Germany) could be wrapped at the distal end of a nasogastric tube or in position of the gastral perforations on a nasojejunal feeding tube. The gastric channel is oronasal redirected and connected to a electronic vacuum pump.
2. Case Report
A 57 years old patient suffered new from dyspnoe and respiratory partial insufficiency. He was treated with ENPT [1, 9, 10] for an insufficiency of the esophago-gastrostomy. Esophagectomy for an esophageal squamous cell carcinoma was made three week ago. Changes of the open-pore devices for ENPT were made every 3-5 days under general anesthesia with intubation in the rooms of the interdisciplinary endoscopy. The known insufficiency of the esophago-gastrostomy was located twenty-four centimeters from the dental arch. A gastroscope could pass the insufficiency into a paragastric mediastinal cave. We detected a fistula into the respiratory tract going out from the mediastinal cave. In the immediately conducted bronchoscopy we found an anergic fistula to the left main bronchus with putrid secretion into the lung with permanent aspiration (Figure 1).

Figure 1: Outline of the anatomical situation (yellow = esophagus and stomach, orange = insufficiency with mediastinal cave, blue = respiratory tract).
2.1 Stent
First step was the change of treatment concept from ENPT to a stent-based approach. A fully-covered self-expandable metal stent (SEMS) was placed in position of the anastomotic region [11]. Finally a jejunal feeding tube was placed.
2.2 Stent and Suction on the mediastinal cave
After endoscopic intervention patient was transferred to the ICU because of respiratory failure. Antibiotic treatment was extended. Furthermore a fluid leackage from the esophagus and the mediastinal cave into the lung was detected. Next endoscopy was required after 48 hours. Change of the treatment concept was indicated: An active drain of the mediastinal cave with an OFD for ENPT was indicated. A wrapped 16 Fr nasogastric tube was placed into the mediastinal cave, oronasal redirected and connected to an electric vacuum pump. After positioning of the open-pore device a fully-covered SEMS was placed over the anastomotic region. Finally a feeding tube was placed into the jejunum.
2.3 Pressure controlled ventilation
Persistent drain of fluids via the fistula was detected bronchoscopically. So we recommended for the ventilated patient a pressure controlled ventilation with a PEEP of 10-12 mmHg for some days to prevent the secretion into the lung. This was the third step.
2.4 Esophageal Stent and Vacuum Therapy in the mediastinal cave and in the stomach
Moreover we used the feeding tube for an ENPT of the stomach. The feeding tube was wrapped with the open-pore film at the gastral perforations of the tube and finally the gastral tube was connected to a vacuum pump. We treated the patient with this concept for 7 days. In the control endoscopy with gastroscopy and bronchoscopy we found a persistent but amended and decreased fistula.
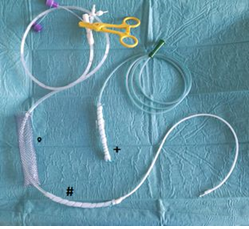
Figure 2: Image of the fully-covered esophageal stent (°) filled with a jejunal tube (#) with wrapped area in gastric position for continuous suction and a wrapped tube (+) positioned in the mediastinal cave.
2.5 Endobronchial Stenting and Vacuum Therapy in the mediastinal cave and in the stomach
Fifth step included an endobronchial stenting with removal of the esophageal SEMS. ENPT with OFD in mediastinal position and active gastral fluid removal with the wrapped feeding tube were continued.

Figure 3: Image of the endobronchial stent (*) and an open-pore film drainage on a naso-gastric tube for the mediastinal cave (+) and an open-pore film drainage on a triluminal tube (#) for the gastric suction (ventilation tube is closed with a yellow clamp) and jejunal feeding.

Figure 4: Endoscopic image of the anastomotic region with the bronchial fistula (**) and a view into the mediastinal cave (++), into the gastric lumen is a wrapped tube positioned for endoluminale negative pressure therapy.

Figure 5: Endoscopic finding of the anastomotic region with completely healed insufficiency.
The fifth treatment concept was maintained for four weeks. Removal of the mediastinal tube was done after two weeks because of good wound cleaning and decreased wound size. Patient recovered completely from the anastomotic insufficiency and the bronchial fistula. Bronchial stent was removed after 4 weeks. Patient could be discharged 12 weeks after oncological resection, 11 weeks after primary detection of an intrathoracic anastomotic insufficiency and 8 weeks after primary detection of an esophago-bronchial fistula. To treat this patient was an interdisciplinary maximum performance. In addition patient developed an anastomotic stricture. At the moment he is treated with endoscopic dilatation interventions every two weeks. No tumor recurrence is detected up to now.
3. Discussion
Development of a tracheobronchaial fistula after esophagectomy is a rare but life-threatening complication. Inflammatory erosion of the tracheobronchial tree could be a reason for such a fistula [2]. Patients suffered on mediastinitis, pleural infusion and aspiration pneumonia. Endoscopic interventions to treat intrathoracic insufficiency after esophagectomy are stent-placement and ENPT. Problems in stent-based treatment concepts are not-cover situations and stent-migration [2, 11]. In a review and meta-analysis by Rausa et al. [4] significantly higher leak closure rate, shorter treatment duration, a lower major complication and in-house mortality rate for ENPT compared to stent-based treatment were described. Negative pressure could not be established in cases of air-leakages.
We report about a demanding complication situation in a vulnerable patient. Finally we used endobronchial stenting and active mediastinal and gastral drainage. The path to optimal treatment needed 5 evolving steps, went by the whole interdisciplinary team. A lot of changes in the endoscopic treatment and relevant changes for the attending physician’s team at the ICU were made. Advanced endoscopic treatment was successful because of good interdisciplinary communication and imaginative endoscopic solutions with usage of currently endoscopic techniques.
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Wichmann D, Schempf U, Mothes B, et al. Endoscopic vacuum therapy for intrathoracic anastomotic insufficiencies following oncological resections. Annals of Esophagus 2 (2019).
- Schweigert M, Dubecz A, Beron M, et al. Management of anastomotic leakage-induced tracheobronchial fistula following oesophagectomy: the role of endoscopic stent insertion. Eur J Cardiothorac Surg 41 (2012): e74-e80.
- Virgilio E, Ceci D, Cavallini M. Surgical Endoscopic Vacuum-assisted Closure Therapy (EVAC) in Treating Anastomotic Leakages After Major Resective Surgery of Esophageal and Gastric Cancer. Anticancer Res 38 (2018): 5581-5587.
- Rausa E, Asti E, Aiolfi A, et al. Comparison of endoscopic vacuum therapy versus endoscopic stenting for esophageal leaks: systematic review and meta-analysis. Dis Esophagus 31 (2018).
- Loske G, Schorsch T, Muller C. Intraluminal and intracavitary vacuum therapy for esophageal leakage: a new endoscopic minimally invasive approach. Endoscopy 43 (2011): 540-544.
- Loske G, Schorsch T, Kiesow RU, et al. First report of urinary endoscopic vacuum therapy: For large bladder defect after abdomino-perineal excision of the rectum. Video paper. Chirurg 88 (2017): 42-47.
- Loske G, Muller CT. Tips and tricks for endoscopic negative pressure therapy. Chirurg 90 (2019): 7-14.
- Loske G, Schorsch T, Rucktaeschel F, et al. Open-pore film drainage (OFD): a new multipurpose tool for endoscopic negative pressure therapy (ENPT). Endosc Int Open 6 (2018): E865-E871.
- Kuehn F, Schiffmann L, Janisch F, et al. Surgical Endoscopic Vacuum Therapy for Defects of the Upper Gastrointestinal Tract. J Gastrointest Surg 20 (2016): 237-243.
- Loske G. Endoscopic negative pressure therapy of the upper gastrointestinal tract. Chirurg 90 (2019): 1-6.
- van Boeckel PG, Sijbring A, Vleggaar FP, et al. Systematic review: temporary stent placement for benign rupture or anastomotic leak of the oesophagus. Aliment Pharmacol Ther 33 (2011): 1292-1301.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
