Pulmonary Glandular Papilloma with Abundant Extracellular Mucin and BRAF V600E, AKT1 E17K Mutations: A Case Report
Zhenyun Yang1, Fengyu Song1, Jin Zhong1,2*
1Department of Internal Medicine, University of California, Riverside, School of Medicine, Riverside, CA, USA
2Pathology and Laboratory Medicine Service, VA Greater Los Angeles, Los Angeles, CA, USA
*Corresponding Author: Jin Zhong, Department of Internal Medicine, University of California, Riverside, School of Medicine, Riverside, CA, USA
Received: 25 June 2022; Accepted: 11 July 2022; Published: 21 July 2022
Article Information
Citation: Zhenyu, Yang, Fengyu Song, Jin Zhong. Pulmonary Glandular Papilloma with Abundant Extracellular Mucin and BRAF V600E, AKT1 E17K Mutations: A Case Report. Archives of Clinical and Medical Case Reports 6 (2022): 532-533.
View / Download Pdf Share at FacebookAbstract
Pulmonary glandular papillomas of the lung are very rare benign pulmonary tumors with only a few cases described in the literature. It is challenging to make the diagnosis based on clinical features, imaging findings and small core biopsies. Here we present a case of pulmonary glandular papilloma with abundant extracellular mucin, which was initially diagnosed as mucinous invasive adenocarcinoma with small core biopsy. Differential diagnosis and its molecular analysis are discussed. Physician should think about the possibility of glandular papilloma for any pulmonary nodules.
Keywords
<p>Pulmonary glandular papilloma; Adenocarcinoma; BRAF V600E; AKT1 E17K mutation</p>
Article Details
1. Introduction
Solitary pulmonary papillomas are very rare tumors with an incidence only less than 0.00395% [1]. Based on the histological findings, solitary pulmonary papillomas can be classified as squamous, glandular, and mixed of both. Among these three categories, solitary pulmonary glandular papilloma is the rarest. There are not many cases of solitary pulmonary papillomas reported in medical literatures, with only a few focusing on the glandular subtype. It has been shown that both squamous and mixed solitary pulmonary papillomas can be malignant but glandular solitary pulmonary papillormas, in general, were previously reported as benign tumors with only one malignant case reported in South Korea in 2017 [2]. The clinical features, imaging findings, and molecular analyses of the solitary pulmonary glandular papilloma are typically not very specific. KRAS or BRAF mutations have been reported in glandular papilloma (3). Solely based on clinical features, imaging findings, and molecular analysis, glandular pulmonary glandular papillomas can often be diagnosed as invasive mucinous carcinoma and other adenoma, particularly, with small endobronchial biopsies.
We describe a case of pulmonary glandular papilloma with abundant extracellular mucin, which was initially diagnosed as mucinous invasive adenocarcinoma in biopsy. The present case shows both BRAF and AKT 1 mutations.
2. Case Study
The patient was a 78-year-old man with a past medical history of hypertension, diabetes, hyperlipidemia, osteoarthritis, colonic mass and prostate cancer status post prostatectomy who presented with CT incidental findings of pulmonary nodule. Pulmonary nodule in right lower lobe is 2.2 cm in long axis, which was increased in size when compared to CT performed 5 months prior (2.0 cm in long axis). PET/CT showed mild FDG uptake with differential diagnosis including solitary metastatic lesion versus primary lung malignancy. A CT-guided biopsy was performed, biopsy (Figure 1A) showed abundant extracellular mucin with uniform columnar cells. The cells have acinar pattern of growth, intracytoplasmic mucin and small basally oriented nuclei, the biopsy was diagnosed as invasive mucinous adenocarcinoma. Next Generation Sequencing (NGS) was done on the biopsy tissue, both BRAF V600E and AKT1 E17K mutations were identified. The patient then underwent right lower lobe lobectomy and lymph nodes dissection. The resection showed a 2.2 x 2.0 x 1.7 cm unencapsulated, ovoid, well-circumscribed mass with ill-defined, pushing borders. The mass appeared to be semi-translucent and gelatinous. Microscopic evaluation showed (Figure 1B) a parenchymal nodule composed of mucinous, ciliated columnar and basal layer appearing cells in papillary, micropapillary and acinar patterns of growth. The tumor was associated with extensive detached papillary and micropapillary formations in alveolar space, extensive expansion and filling of alveolar spaces with mucin. The lobectomy was diagnosed as glandular papilloma.
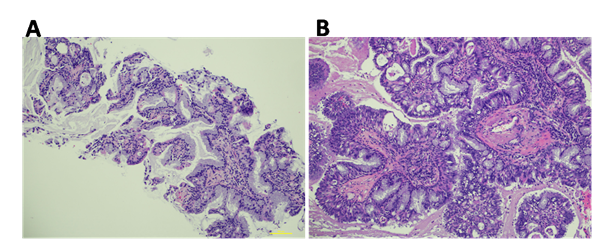
Figure 1: Histomorphology of the tumor. A) Biopsy shows uniform columnar cells with acinar pattern of growth, intracytoplasmic mucin and small basally oriented nuclei. B) Resection shows mucinous, ciliated columnar and basal layer appearing cells in papillary, micropapillary and acinar patterns of growth.
Glandular papilloma is thought to be a rare benign papillary tumor, though one malignant case has been reported [2]. Patients often present with obstructive symptoms such a cough and wheezing. Lesions may be incidentally found on CT. PET avidity has been reported. The present case is incidentally detected by chest CT with mild FDG uptake by PET/CT. Glandular papilloma has been reported to carry either BRAF V600E or KRAS mutations [3], the present case has both BRAF V600E and AKT1 E17K mutations. Interestingly, all these mutations (BRAF, KRAS and AKT1) have been detected and well documented in lung adenocarcinoma [4].
The standard treatment of solitary glandular papilloma of the lung is surgical resection, particularly, lobectomy. It has been shown that surgical resection is very effective treatment with very high successful rate and very low recurrence, often leading to long term, tumor-free survivals [5]. In the present case the patient underwent lymph nodes resection besides lobectomy given the diagnosis of invasive mucinous carcinoma in small biopsy.
Overall, the clinical features, imaging findings and molecular mutation scan be similar between primary invasive lung adenocarcinoma and pulmonary glandular papilloma. The histomorphology of glandular adenoma focally can be indistinguishable from invasive adenocarcinoma for small biopsy, in particular, when the glandular adenoma has extensive extracellular mucin as in the present case. Complete excision is often necessary for definitive diagnosis. Physician/pathologist should think about the possibility of the glandular papilloma for pulmonary nodule even the small biopsy shows features of mucinous adenocarcinoma. Intraoperative evaluation for the lobectomy may be considered if glandular papilloma is on the differential diagnosis.
Conflict of Interest
None to declare
Funding Statement
No funding received for this work.
References
- Wu CW, Chen A, Huang TW. Diagnosis and management of glandular papilloma of lung: A case report. World J Clin Cases; 8 (2020): 1104-1107.
- Sung WJ. Glandular papilloma of the lung with malignant transformation, Yeungnam Univ J Med 34 (2017): 298-302.
- Evangelou Z, Froudarakis M, Ntolios P, et al. Solitary glandular papilloma of the lung with molecular analysis: A case report and literature review. Pathol Res Pract 216 (2020): 152905.
- Griffin R, Ramirez RA. Molecular Targets in Non-small lung Cancer. Ochsner J 17 (2017): 388-392.
- Flieder DB, Koss MN, Nicholson A, et al. Solitary pulmonary papillomas in adults: a clinicopathologic and in situ hybridization study of 14 cases combined with 27 cases in the literature. Am J Surg Pathol 22 (1998): 1328-1342.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
