Stercoral Colitis Complicated with Ischemic Colitis in a Myotonic Dystrophy Patient: A Rare Case Report
Mustafa Almayoof1, Hissa Hamad Almarry2, Eihab Subahi1, Arwa Ajaj3, Gamal Alfitori4
1Department of Medical Education, Internal medicine Residency Program, Hamad Medical Corporation, Doha, Qatar
2Department of Medical Education, Dermatology Residency Program, Hamad Medical Corporation, Doha, Qatar
3Medical student, Qatar University, College of Medicine, QU health, Doha, Qatar
4Department of Internal medicine, Hamad medical corporation, Doha, Qatar
*Corresponding Author: Mustafa Almayoof, Department of Medical Education, Internal medicine Residency Program, Hamad Medical Corporation, Doha, Qatar.
Received: 09 May 2022; Accepted: 25 May 2022; Published: 29 July 2022
Article Information
Citation: Mustafa Almayoof, Hissa Hamad Almarry, Eihab Subahi, Arwa Ajaj, Gamal Alfitori. Stercoral Colitis Complicated with Ischemic Colitis in a Myotonic Dystrophy Patient: A Rare Case Report. Archives of Clinical and Medical Case Reports 6 (2022): 546-549.
View / Download Pdf Share at FacebookAbstract
Stercoral Colitis (SC) is a rare and serious inflammatory condition of the large bowel wall occurs due to distention and increase in the intraluminal pressure secondary to impaction of hard stool. Ischemic colitis may complicate SC and may progress to perforation, and subsequently peritonitis and death if not recognized and treated urgently. Myotonic Dystrophy (DM) has been associated with disorders of the gastrointestinal tract and manifests as reflux, constipation, and dysphagia. Severe colonic impaction, colitis and intestinal pseudo-obstruction, are rarely reported with this condition in the literature. We describe a case of stercoral colitis in a (DM) patient that was successfully treated with conservative measures. We herein present 23-year-old male known case of Myotonic dystrophy (DM) with history of chronic constipation on laxatives, presented with 3 days of abdominal distention, pain, absolute constipation and occasional fecal vomiting. Abdominal exam showed distended abdomen with generalized tenderness with no rigidity or rebound- tenderness. Lab tests were significant for leukocytosis and lactic acidosis. CT (computed tomography) abdomen with contrast: showed marked distention of the rectosigmoid colon with impacted stool, bowel wall thickening and surrounding fat stranding without any finding suggestive of perforation. The patient was diagnosed as case of (SC) with ischemic colitis and treated conservatively with manual evacuation, enema, and laxatives. He dramatically improved and was discharged home. Our conclusion is that stercoral colitis can occur in young patients with a history of chronic constipation like in (DM) patients. Chronic constipation complicated by fecal impaction is the major risk factor for (SC). Computed tomography (CT) is the gold standard imaging modality for the diagnosis of (SC). Elevated lactic acid should raise the suspicion of ischemic colitis complicating the (SC) which requires urgent intervent
Keywords
<p>Stercoral colitis; Ischemic colitis; Myotonic dystrophy; Stercoral perforation</p>
Article Details
Abbreviations
:
SC: stercoral colitis; DM: myotonic dystrophy; CT: computed tomography
1. Background
Stercoral Colitis (SC) is a type of colitis involving large bowel (mainly recto-sigmoid) secondary to fecal impaction. Chronic constipation complicated by fecal impaction is the major risk factor for developing this condition. Fecal impaction may be asymptomatic when there is simple stool impaction but can lead to complications such as bowel wall inflammation, ulcer formation, ischemic pressure necrosis, and subsequently perforation, peritonitis, sepsis, and death [1-3]. Ischemic colitis may complicate SC which occurs secondary to increased intraluminal pressure to the degree that compromises the blood supply to the bowel, if not treated urgently will progress to perforation which carries a high mortality 32-59% [2, 3]. Stercoral colitis seems to be more common in elderly patients with comorbid conditions such as stroke, dementia, Parkinson disease, orthopedic surgery [3, 4]. Few cases of SC have been reported in young patients with metabolic, psychiatric, pharmacotherapy (especially narcotics) and neuro-muscular diseases causing prolonged constipation [5, 6]. Myotonic dystrophy (DM) is a genetic, progressive neuromuscular disease which can affect any part of the gastrointestinal tract and may present with chronic constipation, intestinal pseudo-obstruction, and megacolon. To our knowledge, this is the first case report of SC in DM patient [7, 8]. There are many case reports for SC complicated by perforation in the literature, however very few reports focused on ischemic colitis as a complication of SC. The aim of this case report is to describe the diagnosis and management of SC with ischemic colitis in a patient with a rare neuromuscular condition.
2. Case presentation
23-year-old male known case of Myotonic dystrophy (DM) (with positive genetic, and Electromyography testing for DM). He has chronic constipation since childhood on laxatives with baseline bowel motion every 3rd to 4th day, patient ambulating and has learning impairment. He presented to our emergency department with a 3 day history of increased abdominal distention and generalized, moderate, non-radiating abdominal pain. This was associated with repeated vomiting of fecal matter, and no gas-feces discharge in the last 7 days before presentation. Patient denied any fever, palpitation, or shortness of breath. On examination vitals were PR:110 beat\min. RR:24 breath\min, TEMP.: 36.7 C, BP: 100\60 mmHg, and saturation: 94% on room air. Generally, he looked ill, with dysmorphic facial features of DM (long, thin face with hallow temples and dropping eyelids). Chest examination showed decreased air entry to the right lower zone, Abdominal examination showed distended, abdomen with tenderness all over, with no rigidity or rebound tenderness, and the digital rectal examination showed impacted stool with manual evacuation attempted. Labs showed WBC: 13.3\mcL (normal 4-10), hemoglobin: 15.9 gm\dl (normal 13-17), CRP: 249 (normal; <5), lactic acid: 6.1 (normal 0.5- 2-2), urea:14.2 mmol\L (normal 2.5-7.8), creatinine: 88 umol\L (normal 62-106), blood and urine culture were obtained, which were subsequently negative. A Chest x-ray: showed right-sided pleural effusion, and the abdominal Xray figure (1) showed dilated bowel, with abundant fecal material in the colorectal region. Computed Tomography (CT) scan for abdomen and pelvic with contrast figure (2) showed marked dilatation of rectosigmoid colon with wall thickening and surrounding fat stranding. The dilatation extended to the hepatic flexure with significant fecal loading. The CT findings were suggestive of stercoral colitis with significant fecal loading with no signs of bowel perforation.
Based on the clinical presentation, lab results, and the findings on CT, a diagnosis of stercoral colitis complicated with ischemic colitis was made. There were no clinical or radiological findings to suggest perforation or peritonitis. Urgent conservative treatment with manual evacuation, NG decompression, phosphate enema, and laxative, were established. Also, oxygen support, and IV antibiotics.

Figure 1: showed dilated large bowel with fecal loading (stars).
The patient responded very well to these measures and was able to pass a large amount of stool, with dramatic clinical and biochemical improvement. He started on a new dietary regimen, and regular stimulant laxatives and was discharged home after 7 days of hospital stay in a stable condition. Follow up after 2 months showed that he remained well, back to his baseline with improvement in his constipation.
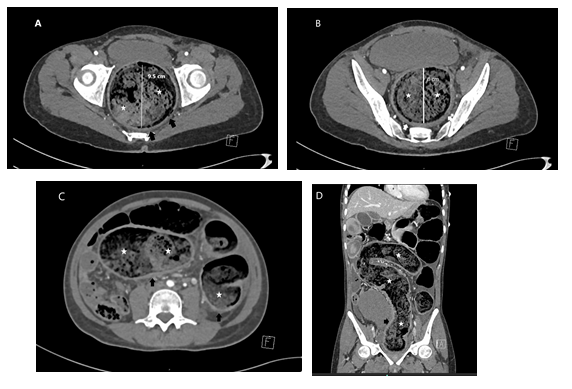
Figure 2: A-D. Axial contrast CT- images (A-C) showing fecal loading (stars) with rectal and sigmoid dilatation measured 9.5 cm, and 8cm respectively. Peri rectal, and Peri colonic fat stranding (black arrows), and diffuse mural thickening in sigmoid colon and rectum (white arrows). (D) coronal CT images also demonstrate colorectal dilatation with abundant fecal material (stars). Pericolic fat stranding (black arrow), and mural thickening.
3. Discussion
Stercoral Colitis (SC) is a rare and serious inflammatory condition involving the large bowel. Chronic constipation complicated by fecal impaction is the major risk factor [3]. Fecal impaction usually occurs in the recto-sigmoid region as it is the narrowest part of the entire colon, and the stool becomes harder and more dehydrated as it progresses through the large bowel. Fecal impaction may be simple and uncomplicated, with just dilatation of colorectal wall or it might be complicated with SC caused by increase in the intraluminal pressure and inflammation of the bowel wall. If the pressure persisted and increased, it may compromise the blood supply resulting in ischemia at the antimesenteric side of the colon, this side of the colon is more vulnerable to ischemia, which will progress if left untreated to bowel wall ulceration, and subsequently perforation, peritonitis, and death [1, 2, 9]. Patients with stercoral colitis usually present with abdominal pain, which may be diffuse or localized in a patient with a history of chronic constipation. This is sometimes associated with abdominal distension, nausea and vomiting as in our patient. If perforation occurs patient may be hemodynamically unstable, with fever, and rigidity on abdominal examination. The clinical presentation is usually not specific for SC and it can happen in other causes of abdominal pain [1,3,10]. The differential diagnosis for SC includes diverticulitis, ulcerative colitis, infectious colitis, malignancy, acute mesenteric ischemia, large bowel obstruction, bowel perforation, and intra-abdominal abscess [1]. Computed Tomography (CT) is the modality of choice, finding of dilated bowel with impacted stool, thickening of the bowel wall, and pericolic fat stranding is diagnostic for SC. Early treatment with manual evacuation, enema, and laxatives may prevent the progression to perforation and subsequent peritonitis, sepsis, and death [1-3]. Ischemic colitis is the condition that results when blood flow to the colon is reduced to the level insufficient to maintain cellular metabolic function. Laboratory findings of elevated lactic acid support the diagnosis of ischemic colitis. Lactic acidosis with imaging finding of SC indicate ischemic colitis complicated SC, and any delay in treatment will increase the risk of colonic perforation which carries a high mortality [2]. Myotonic Dystrophy (DM) is an autosomal dominant, progressive neuromuscular condition with multi-systemic involvement. Disorders at any level of the gastrointestinal tract are relatively common and manifest as disturbances in motility, such as impaired esophageal transport, delayed gastric emptying, and chronic constipation with its consequences. The function of the intestinal smooth muscle and its supply by the enteric nervous system may be damaged in myotonic dystrophy leading to dysmotility [7, 8]. In our case the patient is known case of DM with history of chronic constipation, CT scan showed marked distention of rectosigmoid colon with impacted stool, bowel wall thickening and surrounding fat stranding, findings suggest SC without evidence of perforation, labs showed lactic acidosis, and leukocytosis, the diagnosis of SC complicated by ischemic colitis was made, and started on urgent conservative treatment with manual evacuation, enema and laxative, which led to dramatic clinical and biochemical improvement. The prognosis of stercoral colitis is highly dependent on early diagnosis and management. Though most of SC cases occur in elderly patients with comorbid conditions, there has been no reported significant difference between the age or sex of the patient and mortality. The biggest predictors of mortality are perforation (32% to 59% mortality), a large segment of affected bowel (>40 cm), and ischemic bowel, which is indicated by an elevated lactic acid, or septic shock [3]. The surgical intervention is usually reserved for patients who present with signs of peritonitis secondary to colonic wall perforation, or those who do not respond to the conservative treatment [1,9,10].
In our case the patient did not have an endoscopic and histopathological confirmation of SC with ischemic colitis as he improved with conservative measures, the usual endoscopic features of SC complicated with ischemic colitis include mucosal edema, erythema, ulceration, and obstructing large fecalith at the angulation of sigmoid-descending colon junction. Tissue biopsy usually demonstrate focal active colitis with regenerative glandular changes and neural hyperplasia [2].
4. Conclusion
Stercoral colitis can occur in young patients with history of chronic constipation like in Myotonic Dystrophy (DM) patients. Chronic constipation complicated by fecal impaction is the major risk factor for (SC). Computed Tomography (CT) is the gold standard imaging modality for the diagnosis of (SC). The findings on CT of a dilatation in bowel wall (mainly recto-sigmoid) with fecal impaction, thickening of the bowel wall, and pericolic fat stranding is diagnostic for (SC). Elevated lactic acid should raise the suspicion of ischemic colitis complicating the (SC) which requires urgent intervention to prevent the perforation with its consequent high mortality. Early conservative treatment with manual evacuation, bowel enemas, and laxatives showed to be effective to prevent progression to perforation and concomitant surgery.
Consent for publication
Written informed consent was obtained from the patient's father for publication of this case report and any accompanying images.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- A Tajmalzai, DM Najah. Stercoral colitis due to massive fecal impaction: a case report and literature review. Radiology Case Reports 16 (2021): 1946-1950.
- M Naseer, J Gandhi, N Chams, et al. Stercoral colitis complicated with ischemic colitis: A double-edge sword,” BMC Gastroenterology 17 (2017): 1-6.
- E Ünal, MR Onur, S Balc?, et al. Stercoral colitis: diagnostic value of CT findings,” Diagnostic and interventional radiology (Ankara, Turkey) 23 (2017): 5-9.
- M Forootan, N Bagheri, M Darvishi. Chronic constipation,” Medicine (United States) 97 (2018).
- CP Canders, R Shing, A Rouhani. Stercoral Colitis in Two Young Psychiatric Patients Presenting with Abdominal Pain,” Journal of Emergency Medicine 49 (2015): e99-e103.
- E Proulx, C Glass, “Constipation-Associated Stercoral Colitis,” Pediatric Emergency Care 9 (2018): e159–e160.
- Bellini et al., “Gastrointestinal manifestations in myotonic muscular dystrophy,” World Journal of Gastroenterology : WJG 12 (2006): 1821.
- AM Glaser, JH Johnston, WA Gleason. Myotonic dystrophy as a cause of colonic pseudoobstruction: not just another constipated child,” Clinical Case Reports 3 (2015): 424.
- MF Celayir, HM Köksal, M Uludag. Stercoral perforation of the rectosigmoid colon due to chronic constipation: A case report,” International Journal of Surgery Case Reports 40 (2017): 39.
- S Chakravartty, A Chang, J Nunoo-Mensah. A systematic review of stercoral perforation. Colorectal disease: the official journal of the Association of Coloproctology of Great Britain and Ireland 15 (2013): 930-935.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
